Keywords
INTRODUCTION
The past twenty years have seen the growing range of valve lesion etiologies turn nonvalvular conditions into the primary causes of aortic regurgitation (AR) in Spain.1 Valves present relatively small lesions of the leaflets and concomitant dilatation of the ascending aorta (AA) with AR that can be explained thanks to our improved knowledge of the aortic root's (AoR) role in valve function.2 The geometric relations and dynamic behavior of AoR components have been seen to ensure valve competence when leaflets have no structural lesions.3 The sinuses of Valsalva (SV), sinotubular junction (STJ), and commissures are highly specialized structures: a genuine "supravalvular" aortic apparatus.4,5 Consequently, in AA aneurysms that have evolved over a lengthy period, when geometric changes that distort the insertions of the leaflets occur, the conditions under which these open and close are modified rendering them incompetent.6 In response to this, valve-sparing surgical (VSS) techniques have been developed in aortic aneurysm surgery. Furthermore, interest in AR repair has increased to the point when it is currently offered as an alternative to valve replacement with prostheses.7,8 Until now, decisions on VSS and/or valve repair in AR have been based on the anatomical lesions found by the surgeon in the operating theater, with the patient in induced cardiac arrest and the aorta empty. However, the development of intraoperative transesophageal echocardiography provides a real-time view of the aortic root and valve before thoracotomy.9 Our objective is to conduct in vivo analysis of AR functional anatomy using transesophageal echocardiography (TEE). We aim to describe the underlying lesions and mechanisms, study the diagnostic precision of TEE by comparison with direct surgical inspection, and establish its value in identifying optimal candidates for aortic VSS.
METHODS
Study Population
We operated on 335 consecutive patients diagnosed with aortic valve disease and/or AA dilatation at our center between January 2002 and January 2005. In the present study, we have included 66 who met the following criteria: a) isolated grade ≥2 AR with <25 mm Hg mean transvalvular aortic gradient measured by Doppler echocardiography; b) indication for surgery on the grounds of severe AR or proximal aorta dimensions; c) surgical exploration with aortotomy and direct, independent surgical inspection of lesions; and d) availability of the customary preoperative or intraoperative transesophageal echocardiography study. We excluded patients undergoing urgent surgery for AR or presenting acute aortic syndrome. We excluded no patients on grounds of age, left ventricular dysfunction, chronic AR cause or concomitant mitral valve or coronary artery surgery.
Surgical Anatomy of Aortic Regurgitation
Anatomical lesions were diagnosed according to previously established criteria for direct and macroscopic inspection.10 Descriptions of lesions and mechanisms were transcribed, unaltered, from surgeon's reports or by one of the authors (PGG) based on personal communications provided by the surgeon when conducting a surgical inspection.
Systematic inspection of the AoR was conducted in all cases. Surgeon's reports provided data on: the anatomical form of AA dilatation, number of cusps, leaflet lesions (calcification, commissural fusion and thickening indicating rheumatic disease, lineal fenestrations and thickening of the free border of the commissures, vegetations or perforations, absence of structural lesion and prolapse), flap or dissection and aorta wall rupture.
The surgeon classified underlying mechanisms of regurgitation in four groups: a) functional, if there is no organic lesion or prolapse but functional aortic annulus (STJ and/or annulus) dilatation exists, as in patients with AA or AoR aneurysm; b) restrictive leaflet movement with quite extensive macroscopic structural lesions; c) perforations; and d) prolapse, defined by differences in the free border length of each leaflet, when 1 or 2 of these exceed the rest. Prolapse is subclassified as absolute (the leaflet free border is below its insertion in the SV wall) and relative (the leaflet free border is at the same level as its insertion in the SV wall but below the level of the free border of the remaining leaflets).
Although surgeons knew echocardiographic studies were being conducted they were unaware of the ongoing comparative study. The decision to attempt aortic VSS was based on surgical and not echocardiographic findings. In the remaining cases, or when functional surgery failed, aortic valve replacement (with or without combined replacement of the AA with the supracoronary tube) or AA replacement by a valved conduit using the Bentall procedure, were used at the surgeon's criterion.
Transesophageal Echocardiography
All patients underwent preoperative or intraoperative color Doppler TEE. Transesophageal echocardiography was with Acuson Siemens-Sequoia C-256 (Mountain View, California, USA), Image Point HX (Philips, Andover, Massachusetts, USA) or EnVisor C (Philips, Andover, Massachusetts, USA) equipment using 5-7 MHz transesophageal multiplane probes. Moving and static images were saved in DICOM format. All studies were recorded on magneto-optic disk and in digital format. Reports were by 2 of the authors before the patient entered cardiocirculatory arrest. Each parameter was measured 3 times and the mean was used for statistical analysis.
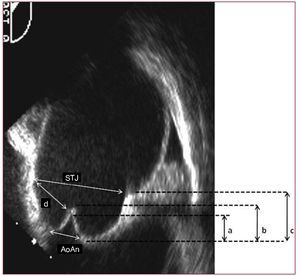
We obtained standard short-axis mid-esophageal projection images of the aortic valve and long-axis mid-esophageal projection images of the AA and aortic valve, rotating the angle to 120º-145°. In both cases, we analyzed the number and absence or presence of organic lesions on the cusps. We considered aortic prolapse had occurred in the presence of sinuous or redundant free border valve leaflets when they appeared normal in systole but in diastole presented complete leaflet eversion or diastolic protrusion in the ventricular outflow tract. We measured annulus, SV, STJ, and AA dimensions and the geometric relation between them, such as the STJ coefficient: annulus (normal, <1.2), SV height (normal, height/annulus ratio <1), tenting height and effective leaflet height (Figure 1).
Figure 1. Mid-esophageal long-axis projection image of the aortic root We identify the annulus and sinotubular joint (STJ) dimensions and the geometric relation between them: STJ:annulus, annulus-STJ distance relations or the height of the sinuses of Valsalva (c), the effective height of each leaflet (b) and the height of tenting (a). (AoAn indicates aortic annulus.)
Statistical Analysis
Quantitative variables are expressed as mean (SD) and categorical variables as percentages of frequencies. For quantitative variables, we compared groups using ANOVA for normal distributions and Kruskal-Wallis for non-normal distributions; for categorical variables, we used #c2 or the Fisher exact test. Taking surgical inspection as our point of reference, we determined sensitivity, specificity, positive and negative predictive values and the precision or general diagnostic accuracy of TEE to diagnose underlying mechanisms and lesions to the cusps or geometric distortion of the AoR and AA. Diagnostic values are expressed as percentages with 95% confidence intervals (CI) and their corresponding kappa values.
We used the Cohen kappa coefficient to determine the level of agreement between TEE-based decisions on repair or valve replacement and decisions based on surgical inspection.We retrospectively analyzed the relation between echocardiographic mechanism, jet direction and geometric relations (Figure 1) and the success of aortic VSS techniques and the AA replacement procedure. We used the Fisher exact test for categorical variables and the Mann-Whitney U test or the Scheffé multiple comparisons test for quantitative variables Multivariate analysis was by logistic regression for variables with P<.05 in univariate analysis. Statistical analysis was with SPSS 12.0 for Windows.
RESULTS
Aortic dilatation, whether or not it is associated with degenerative valve disease, is the primary cause of isolated AR in patients indicated for surgery in our hospital, the reference center in our geographic area for aortic conditions (53%). Up to in 40% of patients with arteriosclerotic aneurysm of the AA and 7/16 patients with annuloaortic ectasia, we found fibroelastic degeneration of leaflets associated with aortic aneurysm. Less frequent causes were valve lesions such as congenital aortic valve disease (21.2%), infectious endocarditis (4%), and rheumatic disease (4.5%). In only 2 patients was the etiology considered unclear (3%).
Surgical Findings
Surgical inspection enabled us to characterize 35 patients who we grouped together under the label of nonvalvular cause AR. This was characterized by AR with no apparent macroscopic structural lesion of the leaflets and/or >2.1 cm/m2 diameter dilatation of the aorta at the level of the SV or the AA.
We described 3 anatomical forms of aortic dilatation: AA aneurysm (type 1), when dilatation of the aorta occurs distal to the STJ and SV geometry is conserved (9 patients); aneurysm of the aortic root (type 2), when dilatation of the sinuses occurs with or without dilatation of the AA, but the aortic annulus is <25 mm (6 patients); annuloaortic ectasia (type 3), when the annulus is >25 mm (18 patients). In only 2 patients with nonvalvular AR, the AA and the AoR were normal, with dilatation of the annulus and STJ as the only geometric distortions.
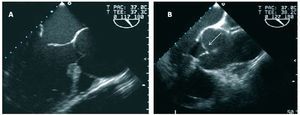
In our series, 2 nonvalvular cause AR mechanisms were found in surgery (Figure 2): functional or tethering of macroscopically normal leaflets due to dilatation of the STJ (14 patients; 41.2%) and valve prolapse (19 patients; 55.9%). The latter was classified by the surgeon as absolute in 6/19 and relative in 13/19 patients. The underlying mechanism was considered to be a lineal fenestration of the free border, paracommissural, in only 2 cases (2.9%) and relatively little calcification of the leaflets in 1 (<1%).
Figure 2. Long-axis projection echocardiographic images of the aorta showing the basic mechanisms of nonvalvular cause aortic regurgitation. A: functional, in which dilatation of the sinotubular joint displaces the commissures outwards, restricts the movement of the leaflets and avoids their coaptation in the center in diastole. B: Relative prolapse and aortic root aneurysm.
Diagnostic Value of Transesophageal Echocardiography
Table 1 summarizes the diagnostic values of TEE in classifying the specific lesions in all 66 patients. The general diagnostic accuracy of TEE to classify etiology (87%; 95% CI, 78-95; kappa =0.82) and characterize the anatomical forms of aortic dilatation (>88%; 95% CI, 80-96; kappa =0.83) is excellent. However, in the detailed description of anatomical lesions of the leaflets, although good, diagnostic accuracy is not optimal (83%; 95% CI, 73-92; Kappa =0.778). Description of the AR mechanism achieved an adequate level of agreement between groups (Kappa =0.8), which in terms of diagnostic precision means 85% (95% CI, 77-94). Valve prolapse was the principle discrepancy in the anatomical and functional evaluation of AR by TEE (23/27). Other diagnostic false negatives were fenestrations of the free border presenting in degenerative conditions (7/9). In both cases, the false echocardiographic diagnosis of the mechanism of regurgitation was tethering of the valve leaflets due to AA dilatation.
Predicting Reparability With Transesophageal Echocardiography
We performed aortic VSS on 32/66 patients and valve replacement on 34/66. Intraoperative TEE predicted aortic VSS was applicable, associated or not with valve repair techniques, as initial surgical procedure in a high percentage of cases (90%). It also predicted the success of the procedure in 80%. Similarly, TEE correctly predicted valve replacement in most cases in which initial surgical inspection clearly ruled out attempting VSS (25/34).
The use of TEE in anatomical and functional classification of lesions associated significantly with applicability of aortic VSS (P<.001). Leaflet tissue quality was the principle factor associated with the decision to repair. Perforations (14% vs 4%), vegetations (7.1% vs 0) or post-inflammatory lesions (9.5% vs 0) and calcifications led to valve replacement using prostheses in a significantly greater number of patients in our series (P<.05). In contrast, flexible leaflets and AR in patients with aortic aneurysm suggested they could be considered candidates for repair (78% vs 55%; P=.03).
In our series, the use of TEE to descried the mechanism was the parameter that best facilitated prediction of AoR reparability (P<.0001). Aortic VSS was successful in 73% of cases of functional annulus dilatation (tethering). But 78% of the cases of prolapse, 90% of those with thickened or calcified leaflets and up to 100% of leaflets with perforations were treated with aortic valve replacement.
In nonvalvular AR, together with the mechanism and direction of the regurgitating jet (central, 71% success vs 29% failure; P=.001), the symmetry or absence of differences in effective leaflet height (difference of success b, 0 [0.1], vs failure, 2.8 [0.6]; P=.005) was the variable that independently associated with the possible success of remodeling surgery without leaflet repair (Table 2).
Finally, we found a statistically significant association between the different anatomical-clinical forms of the aneurysm and the AA replacement procedure (P=.004): in type 1, supracoronary conduit, with or without valve prosthesis (13/19); remodeling of the root in type 2 (3/5), or reimplantation of the native valve in a prosthetic conduit in subvalvular position or implantation of a valved conduit using Bentall's procedure in type 3 or in Marfan's syndrome with any anatomical form of dilatation (19/24) (Figure 3).
Figure 3. Transesophageal echocardiography images of the different anatomic-clinical forms of ascending aorta dilatation A: supratubular dilatation. B: aortic root dilatation. C: annuloaortic ectasia.
DISCUSSION
Surgical management of AR has changed as nonvalvular forms associated with AA conditions have become the most frequent causes.1 To a great extent, success with these techniques depends on the functional anatomy of the root and the aortic valves, which underlines the importance of preoperative lesion diagnosis. Our study shows that, as in mitral valve failure, TEE is of great value in preoperative evaluation of the underlying mechanisms and anatomical lesions of valvular and nonvalvular cause AR and, particularly, in the optimal selection of candidates for aortic VSS techniques.
Diagnosis of Anatomical Lesions
When we analyze the diagnostic value of preoperative TEE for each specific form of AR, we find optimal figures for sensitivity and specificity (>95%) of descriptions of AA aneurysm and valvular-cause lesions . Moreover, all cases of bicuspid valves were correctly diagnosed by TEE. This coincides with data recently published by Alegret et al.11 However, we found discrepancies in nonvalvular AR. Principally, these occurred in diagnoses of relative prolapse and free border fenestrations. In these cases, the valve lesion was incorrectly diagnosed as normal leaflets and functional failure.
In root aneurysm, SV dilatation can cause leaflet tissue remodeling. This remodeling is an attempt to compensate for the mechanical overload on the leaflet when the aorta loses its geometry and free border lengthening and thickening occur.12 Hence, relative prolapse is a common lesion in these patients. In many of them, who underwent surgical and echocardiographic inspections under clearly different conditions of aortic filling, the leaflet lesion caused by very subtle stretching can go unnoticed in TEE and AA dilatation may be incorrectly diagnosed as the only lesion. In our series, although in both mechanisms tenting height increases, the symmetry of effective leaflet height can help differentiate the entities.
Identifying prolapse is essential in the context of aortic VSS. Not correcting preexisting prolapse is the primary cause of early failure of repeat valve implantation or root remodeling procedures13 and effective low coaptation height in repaired valves identifies those that progress to regurgitation and require repeat intervention.14 Recently, in AR series very like ours, Le Polain de Waroux et al15 and El Khoury et al16 have described a lesion type that constitutes the principle diagnostic errors of echocardiography. They are characterized by a regurgitant jet with an eccentric direction. In our series, central jet direction is associated with aortic VSS success. Therefore, presence of an eccentric jet in nonvalvular AR, still in the absence of apparent structural leaflet lesion, forces the surgeon to explore carefully the anatomy and length of the free border of the leaflets to diagnose prolapses or fenestrations that might go unnoticed.
Diagnosis of Mechanisms
One of echocardiography's principle contributions in valvular disease is that it facilitates obtaining detailed images of the valve and the AoR functioning in physiological conditions with blood pressure. In AR, no unanimously accepted criterion for adequate patient selection exists as yet. Decisions on VSS and/ or valve repair are made on the basis of the anatomical lesions found by the surgeon in the theater, with the heart in arrest and the aorta empty. However, we cannot ignore the effect in vivo arterial pressure has on leaflet or aorta behavior with alterations to the elasticity (as happens in degenerative conditions). The development of intraoperative TEE has enabled us to make a systematic approximation to the structural-functional interrelations—ie, to the mechanisms of regurgitation—prior to thoracotomy. Our results show the significant relation between echocardiographic diagnosis of AR mechanism and success with these surgical techniques. Patients with functional AR due to STJ dilatation with leaflet tethering are the best candidates for aortic VSS. Therefore, as Le Polain et al15 show, in aortic repair the role of the TEE in diagnosing the mechanism can be crucial for the surgeon when determining the probability of successfully applying aortic VSS in the surgical treatment of AA aneurysm.
Diagnosis of Reparability
In aortic aneurysm surgery, a high probability of success in aortic VSS is an incentive to the early application of the techniques, before the extreme dimensions of the aorta17 and severe AR limit the results.18 Despite the fact that few patients are subjected to VSS techniques, the anatomical and functional classification of lesions in our patients associated significantly with the applicability of aortic VSS.
The quality of leaflet tissue is a principle factor guaranteeing reparability.19 Moreover, in the absence of extensive leaflet lesions, the direction of the regurgitant jet has been considered the principle echocardiographic criterion that distinguishes functional AR from valvular AR, in both echocardiographic series15 and surgical classifications.16,20 However, the Belgian echocardiographic and surgical series15,16 and the French functional classification20 disagree about the significance of jet direction. Lansac et al20 consider the central jet is characteristic of AR when this is due to functional annulus dilatation; the Belgians also found a central jet in AR secondary to restrictive disease of the leaflets. The geometric relation parameters of the leaflets with respect to the SV that we propose enable us to explain these diverging findings. Only the different effective height of the leaflets attained statistical significance in multivariate analysis. Therefore, faced with an eccentric jet in the absence of structural lesion of the leaflets, although TEE may indicate possible diastolic tenting of the valve leaflets,21 we must confirm their symmetry to diagnose prolapses that might otherwise go unnoticed.
In order to treat aortic aneurysm, various aortic VSS techniques have been developed (remodeling and reimplantation). Their objective is to repair AR correcting the lesions and preserving AoR dynamics.22 The present study shows a close relation exists between the echocardiographic description of the different anatomical-clinical forms of AA dilatation and the choice of aorta replacement procedure. However, patients with Marfan's syndrome23 or a family history of dissection underwent valve reimplantation regardless of aneurysm morphology. Therefore, the choice of one procedure or another depends—together with the experience of the surgeon—on the underlying disease and the anatomical form of the aneurysm.
CONCLUSIONS
Intraoperative TEE permits precise description of the valve and AoR lesions and of the mechanisms of valve incompetence, in all forms of AR. It generally coincides with surgical observations, adequately predicts the applicability of aortic VSS techniques and of the AA replacement procedure. Nonvalvular functional AR, secondary to aneurysm of the aorta with leaflets without structural lesion is the best candidate for techniques of aortic valve conservation with or without leaflet repair.
ABBREVIATIONS
AA: ascending aorta
AoR: aortic root
AR: aortic regurgitation
STJ: sinotubular junction
SV: sinuses of Valsalva
TEE: transesophageal echocardiography
VSS: valve-sparing surgery
See editorial on pageS 513-5
Correspondence: Dr. P. Gallego.
Servicio de Cardiología. Hospital Universitario Virgen Macarena. Avda. Dr. Fedriani, 3. 41071 Sevilla. Spain
E-mail: pastoragallego@teleline.es
Received April 13, 2009.
Accepted for publication November 25, 2009.