Exposure to secondhand smoke (SHS) causes cardiovascular disease, respiratory disease, and cancer. The aim of this study was to estimate the mortality attributed to SHS in people aged ≥ 35 years in Spain and its autonomous communities (AC) by sex from 2016 to 2021.
MethodsEstimates of SHS-attributable mortality were calculated by applying the prevalence-dependent method where SHS exposure was derived from the adjustment of small-area models and based on the calculation of population-attributed fractions. Sex, age group, AC, and cause of death (ischemic heart disease and lung cancer) were included. The estimates of attributed mortality are presented with their 95% confidence interval (95%CI). Crude and age-standardized rates were estimated for each sex and AC.
ResultsFrom 2016 to 2021, SHS exposure caused 4,970 (95%CI, 4,787-5,387) deaths, representing 1.6% of total mortality for ischemic heart disease and lung cancer. The burden of attributed mortality differed widely among the AC, with Andalusia having the highest burden of attributed mortality (crude rate: 46.6 deaths per 100 000 population in men and 17.0/100 000 in women). In all the AC, the main cause of death in both sexes was ischemic heart disease. The highest burden of mortality was observed in nonsmokers.
ConclusionsThe burden of SHS-attributable mortality was high and varied geographically. The results of this study should be considered to advance tobacco control legislation in Spain.
Keywords
Secondhand smoke (SHS) has been recognized as a human carcinogen since 2006; it is causally associated with ischemic heart disease and lung cancer in nonsmokers, and there is no known safe threshold for exposure.1 According to the World Health Organization, exposure to SHS causes more than 1 million deaths a year.2
Protection from SHS exposure in Spain improved with the approval of Law 28/2005 on Health Measures Against Smoking3 and its subsequent amendment through Law 42/2010.4 Both laws marked a public health milestone and positioned Spain at the forefront of international efforts to legally address the problem of involuntary exposure to tobacco smoke.
Two indicators can be used to assess SHS exposure in the general population: prevalence of exposure and burden of mortality attributable to exposure. The first estimates of SHS exposure in Spain were generated from responses to the 2006 National Health Survey5 and the 2009 European Health Survey.6 Three studies have analyzed mortality attributable to SHS in Spain. The first 2, published in 20027 and 2011,8 estimated that approximately 1000 never smokers aged ≥35 years died of ischemic heart disease or lung cancer each year. The third study, based on data for 2020, estimated that SHS caused 747 deaths a year, but in this case, the population included smokers, former smokers, and never smokers.9
Spain has 17 autonomous communities that operate with varying degrees of self-governance. More accurate estimates of mortality attributable to SHS in each of these regions would help identify priority areas for intervention. To our knowledge, no studies to date have calculated deaths attributable to SHS exposure in the different regions of Spain. The aim of this study was to estimate SHS-attributable mortality in both men and women aged ≥35 years in each of the country's autonomous communities for the period 2016 to 2021.
METHODSMortality attributable to SHS was estimated using a prevalence-based method and population attributable fractions (PAFs), with adjustments for age group (35-54, 55-64, 65-74, and ≥75 years), sex, place of residence (autonomous community), and cause of death (ischemic heart disease or lung cancer). This study followed the STREAMS-p (Strengthen the design and REporting of Attributable Mortality Studies using a Prevalence-based method) guidelines.10
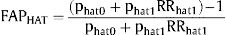
PAFs were calculated as:
where pSHS0 and pSHS1 are the respective prevalences of nonexposure and exposure to SHS, and RRSHS1 is the relative risk of death due to ischemic heart disease or lung cancer among exposed vs unexposed individuals.
For each group (defined by sex, age group, place of residence, and cause of death), mortality attributable to SHS was estimated by multiplying the observed mortality by the PAF: AM=OM × PAF.
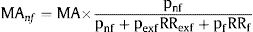
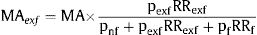
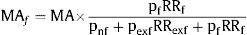
Mortality attributable to SHS was also analyzed separately for never smokers, former smokers, and smokers. The corresponding equations are shown below:
Never smokers:
Former smokers:
Smokers:
where AM refers to attributable mortality and pnf,pexf and pf denote the respective prevalences of never smokers, former smokers, and smokers and RRexf and RRf the risk of death due to ischemic heart disease or lung cancer among smokers and former smokers vs never smokers.
We estimated crude and age-standardized attributable mortality rates. Age-standardized rates were calculated using the direct method with adjustment for sex and place of residence and application of the European standard population proposed by Eurostat's Task Force based on projections for the period 2011 to 2030.11
Attributable mortality rates with their 95%CIs were calculated using a naïve Bootstrap method and Efron's percentile method.
Data sourcesData from the 2017 Spanish National Health Survey (n=23 089)12 and the 2020 European Health Survey for Spain (n=22 072)13 were used to estimate the prevalence of smoking and exposure to SHS in two 3-year periods: 2016 to 2018 (2017 survey) and 2019 to 2021 (2020 survey). SHS exposure was assessed by analyzing answers to the question “How often are you exposed to tobacco smoke indoors? Consider only situations where other people are smoking”. The categories for the 2017 survey were “never or hardly ever”, “less than 1 hour a day”, “between 1 and 5hours a day”, and “more than 5hours a day”. For the 2020 survey, they were “never or hardly ever”, “every day”, “at least once a week (but not every day)”, and “less than once a week”. Individuals who answered anything except “never or hardly ever” were considered to have been exposed to SHS. Smokers were defined as people who were smoking at the time of the survey, former smokers as those who had quit, and never smokers as those who had never smoked. A mixed-effects multinomial logistic model with random area effects was used to improve the accuracy of the estimated prevalence of smoking and SHS exposure by sex, age, and place of residence. The dependent variables were the number of smokers, former smokers, or people exposed to SHS according to age, sex, and place of residence. Independent variables were factors associated with smoking and exposure to SHS, such as level of education, employment status, occupation, and income level. The model used is described in more detail elsewhere.14,15 The prevalence estimates for SHS exposure are provided in tables 1 and 2 of the supplementary data.
The RRs of developing ischemic heart disease (RR=1.27) or lung cancer (RR=1.16) in exposed vs unexposed individuals were obtained from the 2006 US Surgeon General's report on the Health Consequences of Involuntary Exposure to Tobacco Smoke.1 The risks of death due to ischemic heart disease or lung cancer in smokers and former smokers vs never smokers by sex and age were derived from 5 US cohorts.16 The risks used are shown in tables 3 and 4 of the supplementary data.
Observed mortality figures for adults aged ≥35 years, classified by sex, age, place of residence, and cause of death, for the years 2016 to 2021 were obtained from the Spanish National Statistics Institute. Information was collected on all individuals whose main cause of death was classified as ischemic heart disease (codes I20-25 of the International Classification of Diseases, 10th edition [ICD-10]) or tracheal, lung, and bronchial cancer (ICD-10 codes C33 and C34).17
Sensitivity analysisAttributable mortality was estimated using RRs applied in previous calculations for Spain.18,19 The burden of mortality attributable to chronic obstructive pulmonary disease (COPD; ICD-10 codes J40-44) and cerebrovascular disease (ICD-10 codes I60-69) was also assessed. The risks used in this case were taken from meta-analyses20,21 and are shown in table 3 of the supplementary data.
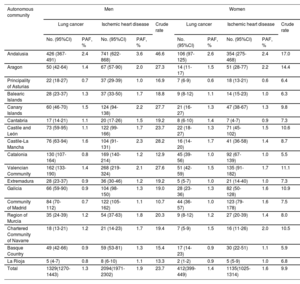
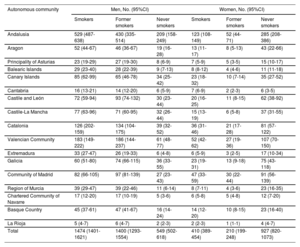
RESULTSBetween 2016 and 2021, exposure to SHS in Spain caused 4970 (95%CI, 4787-5387) deaths in adults aged ≥ 35 years. This corresponds to 1.6% of all observed deaths due to ischemic heart disease and lung cancer in that period. SHS was responsible for 3423 (95%CI, 3241-3742) deaths in men and 1547 (95%CI, 1434-1760) in women. In men, 2094 (95%CI, 1971-2302) deaths were due to ischemic heart disease (table 1), with 549 (95%CI, 502-618) occurring in never smokers, and 1400 (95%CI, 1293-1554) in former smokers. The respective figures for female never and former smokers were 927 (95%CI, 820-1073) and 210 (95%CI, 199-248) (table 2).
Mortality attributable to secondhand smoke with 95%CIs, population attributable fractions (PAFs), and crude mortality rates (per 100 000 inhabitants). The results are shown by sex, cause of death, and autonomous community
| Autonomous community | Men | Women | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lung cancer | Ischemic heart disease | Crude rate | Lung cancer | Ischemic heart disease | Crude rate | |||||
| No. (95%CI) | PAF, % | No. (95%CI) | PAF, % | No. (95%CI) | PAF, % | No. (95%CI) | PAF, % | |||
| Andalusia | 426 (367-491) | 2.4 | 741 (622-868) | 3.6 | 46.6 | 106 (97-125) | 2.6 | 354 (275-468) | 2.4 | 17.0 |
| Aragon | 50 (42-64) | 1.4 | 67 (57-90) | 2.0 | 27.3 | 14 (11-17) | 1.5 | 51 (28-77) | 2.2 | 14.4 |
| Principality of Asturias | 22 (18-27) | 0.7 | 37 (29-39) | 1.0 | 16.9 | 7 (6-9) | 0.6 | 18 (13-21) | 0.6 | 6.4 |
| Balearic Islands | 28 (23-37) | 1.3 | 37 (33-50) | 1.7 | 18.8 | 9 (8-12) | 1.1 | 14 (15-23) | 1.0 | 6.3 |
| Canary Islands | 60 (46-70) | 1.5 | 124 (94-138) | 2.2 | 27.7 | 21 (16-27) | 1.3 | 47 (38-67) | 1.3 | 9.8 |
| Cantabria | 17 (14-21) | 1.1 | 20 (17-26) | 1.5 | 19.2 | 8 (6-10) | 1.4 | 7 (4-7) | 0.9 | 7.3 |
| Castile and León | 73 (59-95) | 1.1 | 122 (99-166) | 1.7 | 23.7 | 22 (18-27) | 1.3 | 71 (45-102) | 1.5 | 10.6 |
| Castile-La Mancha | 76 (63-94) | 1.6 | 104 (91-131) | 2.3 | 28.2 | 16 (14-20) | 1.7 | 41 (36-58) | 1.4 | 8.7 |
| Catalonia | 130 (107-164) | 0.8 | 169 (140-214) | 1.2 | 12.9 | 45 (39-56) | 1.0 | 92 (67-139) | 1.0 | 5.5 |
| Valencian Community | 162 (133-190) | 1.4 | 268 (219-324) | 2.1 | 27.6 | 51 (42-59) | 1.5 | 135 (91-182) | 1.7 | 11.1 |
| Extremadura | 28 (23-37) | 0.9 | 36 (30-46) | 1.2 | 19.2 | 5 (5-7) | 1.0 | 21 (14-40) | 1.0 | 7.3 |
| Galicia | 66 (59-90) | 0.9 | 104 (98-150) | 1.3 | 19.0 | 28 (23-36) | 1.3 | 82 (50-128) | 1.6 | 10.9 |
| Community of Madrid | 84 (70-112) | 0.7 | 122 (105-162) | 1.1 | 10.7 | 44 (36-57) | 1.0 | 123 (79-178) | 1.6 | 7.5 |
| Region of Murcia | 35 (24-39) | 1.2 | 54 (37-63) | 1.8 | 20.3 | 9 (8-12) | 1.2 | 27 (20-39) | 1.4 | 8.0 |
| Chartered Community of Navarre | 18 (13-21) | 1.2 | 21 (14-23) | 1.7 | 19.4 | 7 (5-9) | 1.5 | 16 (11-26) | 2.0 | 10.5 |
| Basque Country | 49 (42-66) | 0.9 | 59 (53-81) | 1.3 | 15.4 | 17 (14-23) | 0.9 | 30 (22-51) | 1.1 | 5.9 |
| La Rioja | 5 (4-7) | 0.8 | 8 (6-10) | 1.1 | 13.3 | 2 (1-2) | 0.9 | 5 (5-9) | 1.0 | 6.8 |
| Total | 1329(1270-1443) | 1.3 | 2094(1971-2302) | 1.9 | 23.7 | 412(399-449) | 1.4 | 1135(1025-1314) | 1.6 | 9.9 |
95%CI, 95% confidence interval; PAF, attributable fraction.
Mortality attributable to secondhand smoke with 95%CIs. The results are shown by smoking status, sex, and autonomous community
| Autonomous community | Men, No. (95%CI) | Women, No. (95%CI) | ||||
|---|---|---|---|---|---|---|
| Smokers | Former smokers | Never smokers | Smokers | Former smokers | Never smokers | |
| Andalusia | 529 (487-638) | 430 (335-514) | 209 (158-249) | 123 (108-149) | 52 (44-71) | 285 (208-386) |
| Aragon | 52 (44-67) | 46 (36-67) | 19 (16-28) | 13 (11-17) | 8 (5-13) | 43 (22-66) |
| Principality of Asturias | 23 (19-29) | 27 (19-30) | 8 (6-9) | 7 (5-9) | 5 (3-5) | 15 (10-17) |
| Balearic Islands | 29 (23-40) | 28 (22-39) | 9 (7-13) | 8 (8-12) | 4 (4-6) | 11 (11-18) |
| Canary Islands | 85 (62-99) | 65 (46-78) | 34 (25-42) | 23 (18-32) | 10 (7-14) | 35 (27-52) |
| Cantabria | 16 (13-21) | 14 (12-20) | 6 (5-9) | 7 (6-9) | 2 (2-3) | 6 (3-5) |
| Castile and León | 72 (59-94) | 93 (74-132) | 30 (23-44) | 20 (16-25) | 11 (8-15) | 62 (38-92) |
| Castile-La Mancha | 77 (63-96) | 71 (60-95) | 32 (26-44) | 15 (13-19) | 6 (5-8) | 37 (31-55) |
| Catalonia | 126 (202-159) | 134 (104-175) | 39 (32-52) | 36 (31-46) | 21 (17-28) | 81 (57-122) |
| Valencian Community | 183 (149-222) | 186 (144-237) | 61 (48-77) | 52 (42-62) | 27 (19-36) | 107 (70-150) |
| Extremadura | 33 (27-47) | 26 (19-33) | 6 (4-8) | 6 (5-9) | 3 (2-5) | 17 (10-34) |
| Galicia | 60 (51-80) | 74 (66-115) | 36 (33-55) | 23 (19-31) | 13 (9-18) | 75 (43-118) |
| Community of Madrid | 82 (66-105) | 97 (81-139) | 27 (23-43) | 47 (33-59) | 30 (22-44) | 91 (56-139) |
| Region of Murcia | 39 (29-47) | 39 (22-46) | 11 (6-14) | 8 (7-11) | 4 (3-6) | 23 (16-35) |
| Chartered Community of Navarre | 17 (12-20) | 17 (10-19) | 5 (3-6) | 6 (5-8) | 5 (4-8) | 12 (7-20) |
| Basque Country | 45 (37-61) | 47 (41-67) | 16 (14-24) | 14 (12-20) | 10 (8-15) | 23 (16-40) |
| La Rioja | 5 (4-7) | 6 (4-7) | 2 (2-3) | 2 (2-3) | 1 (1-1) | 4 (4-7) |
| Total | 1474 (1401-1621) | 1400 (1293-1554) | 549 (502-618) | 410 (389-454) | 210 (199-248) | 927 (820-1073) |
The burden of mortality due to ischemic heart disease or lung cancer attributed to SHS exposure varied geographically, with the lowest rates observed in the Principality of Asturias (0.7% for men and 0.6% for women) and the highest in Andalusia (3.6% for men and 2.6% for women). Ischemic heart disease was the main cause of death in men and women, regardless of place of residence. Crude mortality rates in men ranged from 46.6 deaths per 100 000 inhabitants in Andalusia to 10.7 deaths per 100 000 inhabitants in the Community of Madrid (table 1). In women, the rate ranged from 17.0 deaths per 100 000 inhabitants in Andalusia to 5.5 deaths per 100 000 inhabitants in Catalonia. The highest rates, in all regions, were observed in never smokers, particularly in the subgroup of women (table 2).
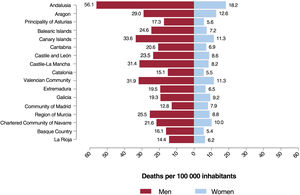
Age-standardized mortality rates for men ranged from 56.1 deaths per 100 000 inhabitants in Andalusia to 12.8 deaths per 100 000 inhabitants in the Community of Madrid. For women, they ranged from 18.2 deaths per 100 000 inhabitants in Andalusia to 5.4 deaths per 100 000 inhabitants in the Basque Country (figure 1 and table 1). Both crude and age-standardized rates differed between the two 3-year periods analyzed (table 5 of the supplementary data).
Application of the RRs used in other studies analyzing mortality attributable to SHS in Spain yielded a total of 6134 (95%CI, 5923-6624) deaths; this is 23.4% higher than the figure obtained in our analysis.
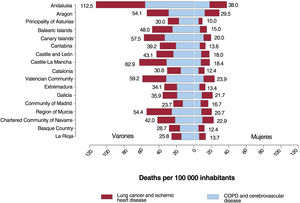
When COPD and cerebrovascular disease were included in the analysis, the number of deaths attributable to SHS exposure between 2016 and 2021 increased to 9579 (95%CI, 9290-10 240). The greatest increase was observed for Andalusia, with age-standardized mortality rates increasing from 56.1 to 112.5 deaths per 100 000 inhabitants for men and from 18.2 to 38.0 deaths per 100 000 inhabitants for women (figure 2).
DISCUSSIONBetween 2016 and 2021, exposure to SHS in Spain caused approximately 5000 deaths due to ischemic heart disease or lung cancer and more than 9000 deaths due to ischemic heart disease, lung cancer, COPD, or cerebrovascular disease. The burden of mortality attributable to SHS exposure varied regionally, with the highest rates observed in Andalusia.
Although mortality attributable to SHS has been previously studied in Spain, ours is the first study to estimate rates for each of the country's 17 autonomous communities. Our findings confirm the existence of regional variations, although consideration must be paid to differences in the number of inhabitants and age structure. Andalusia and Catalonia, for example, with 18% and 16% of the country's total population respectively, have the largest populations. SHS-attributable ischemic heart disease and lung cancer deaths, however, were much higher in Andalusia than in Catalonia (33% vs 9%). Regional variations in age structure should also be taken into account, as they, rather than differences in SHS exposure, might explain differences in mortality rates. Spain has an overall aging index of 129.1, but regional indices range from 90.3 in the Region of Murcia to 231.1 in the Principality of Asturias. Andalusia and Catalonia have some of the youngest populations, with indices of 107.8 and 120.1, respctively.22 Nonetheless, when mortality rates were standardized for age, Andalusia still had the highest number of SHS-attributable deaths in both men and women. The age-standardized mortality rate in Andalusia, at 56.1 deaths per 100 000 inhabitants, was 4-times that of the region with the lowest rate, the Community of Madrid, with 12.8 deaths per 100 000 inhabitants. These variations can largely be explained by regional differences in exposure to SHS. In Andalusia, for example, more than 25% of men and women aged <65 years reported being exposed to SHS. The corresponding rate in the Community of Madrid was around 10%. These differences are likely reflections of differences in lifestyle habits and compliance with smoking laws. Andalusia, for instance, has one of the highest smoking rates and number of bars per 100 000 inhabitants in Spain, while Madrid has one of the lowest smoking rates and the fewest bars per 100 000 inhabitants.23,24 We were unable to compare regional levels of compliance with smoking laws, as the surveys used did not specify site of exposure.
Supporting previous findings for Spain, mortality attributable to SHS was higher in men than women. This finding was expected as men also had higher SHS exposure and observed mortality rates. Observed mortality rates were higher in men for all the conditions analyzed except cerebrovascular disease, and the difference was particularly evident in the case of lung cancer and COPD.17 Smoking is the main risk factor for both these diseases, and it should be noted that women started smoking significantly later than men in Spain.23
Another notable finding is the significant impact of SHS exposure on death due to ischemic heart disease and lung cancer in women who had never smoked: 60% of all SHS-attributable deaths in women occurred in never smokers. The corresponding rate for men was just 16%. The disparate results are probably linked to differences in smoking habits, as in Spain, more women than men have never smoked.23
It is not easy to compare our results with findings from other countries. In the past 5 years, just 3 studies that are strictly comparable in terms of causes of death and age have been conducted in other countries (China,25 the United States,26 and Morocco27). The Moroccan study reported an SHS-attributable mortality rate of 0.63% for individuals aged ≥35 years. This is higher than the rate of 0.19% detected for Spain in 2021 (data not shown), possibly because of differences in SHS exposure rates, lifestyle habits, and time periods analyzed (the Moroccan study analyzed data for 2012).
StrengthsThis study has several strengths. Notably, it is the first to estimate regional differences in mortality attributable to SHS. This is a particular strength, as our findings can be used to help regional and national policymakers make evidence-based decisions on smoking restrictions. National smoking laws in Spain have remained unchanged since the last amendment in 2010. While there have been some regional changes, these have been inconsistent. The Canary Islands, for example, banned smoking on beaches, while in Catalonia, there is a plan to ban smoking on the terraces of bars and restaurants.
Our study is also the first to apply a small-area model to estimate the prevalence of SHS exposure by age and sex group. The use of small-area models in similar studies has helped generate more accurate estimates of smoking rates.14,15 The sensitivity analysis is another strength, as it enabled a more comprehensive examination of the methodological complexities associated with studies of this nature. Our estimates are the most conservative possible, as they are based only on causes of death with an established causal link to SHS exposure in the 2006 Surgeon General's Report (ischemic heart disease and lung cancer). While there is evidence suggesting a causal link between SHS exposure and COPD and cerebrovascular disease,28–30 these conditions were only included in our sensitivity analysis. Although the sensitivity analysis did not consider the effects of smoking, it is important to assess the impact of SHS exposure on mortality among smokers. While the risk posed by SHS is negligible compared with the risk of smoking itself, there is some evidence of additive or synergistic effects.31,32 A final strength of this study is that the death records were obtained from the Spanish National Death Registry, a high-quality dataset in which just 0.7% of deaths have an ill-defined or unknown cause (ICD-10 code R99).
LimitationsThis study also has some limitations. Notably, we were unable to conduct a more detailed analysis of the impact of SHS exposure on mortality due to the unavailability of annual data. The use of data from 2017 and 2020 to generate estimates for the periods 2016 to 2018 and 2019 to 2021, respectively, required the assumption that SHS exposure rates would not vary significantly within these periods. Because they were closer in time, prevalence data from 2017 rather than 2014 were used to estimate attributable mortality in 2016. Nonetheless, the rates were similar for both years. The use of self-reported survey data for the estimates may have resulted in an underestimation of actual SHS exposure33 and, accordingly, mortality attributable to exposure. Considering individuals with occasional exposure to SHS as unexposed might also have contributed to an underestimation of attributable mortality. It should be noted that the risk levels used in our calculations were from studies conducted outside Spain. The risks selected, however, represent the best possible evidence, as they were taken from meta-analyses and large cohort studies with long follow-up times. The true impact of exposure to SHS will necessarily be underestimated as we only studied adults. We did not, for instance, investigate the potential effects of exposure on sudden infant death syndrome. Finally, considering the time periods analyzed, our findings might have been influenced by the COVID-19 pandemic. According to official estimates for Spain, COVID-19 caused 60 358 confirmed and 14 481 suspected deaths in 2020.17 The impact of these deaths on our estimates is uncertain.
CONCLUSIONSSHS exposure causes approximately 2 avoidable deaths every day in Spain. Our findings, however, show that the effects vary regionally and indicate that both the central government and regional authorities should legislate accordingly to reduce exposure, particularly in areas with high rates of SHS-attributable mortality. Successful initiatives implemented in other places, such as California, should be analyzed. Banning smoking in public areas34 such as beaches and state parks,35 cars when children are present,36 and multidwelling units37 would strengthen protection against involuntary exposure to tobacco smoke and heighten awareness among the general public of the importance of reducing exposure to SHS, which is a significant risk factor for numerous life-threatening diseases, in particular ischemic heart disease.
- -
Exposure to SHS increases the risk of death due to ischemic heart disease and lung cancer. Three studies to date have estimated mortality attributable to SHS exposure in Spain, but none of them have analyzed regional differences.
- -
Between 2016 and 2020, exposure to SHS caused 4970 deaths in individuals aged ≥35 years in Spain; 3230 of the deaths were due to ischemic heart disease and 1740 to lung cancer. The burden of attributable mortality varied regionally. Andalusia had the highest rates for both men and women. The lowest rates were observed in the Community of Madrid for men and Catalonia for women.
This study was funded by the Instituto de Salud Carlos III (ISCIII) via project PI22/00727 and cofunded by the European Union. It also received funding through a SEPAR 2023 grant (Project 1426).
ETHICAL CONSIDERATIONSThis study was conducted in accordance with the principles for international medical research outlined in the Declaration of Helsinki. Ethical approval and informed consent were not necessary, as the study did not involve the participation of humans (or identifiable human material or data) or interventions involving humans. Sex and gender issues were taken into consideration in the study design and analysis.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence tools were used in the preparation of this manuscript.
AUTHORS’ CONTRIBUTIONSJ. Rey-Brandariz: conception, data acquisition, interpretation of results, editing and critical review of manuscript; C. Guerra-Tort: data analysis, interpretation of results, editing and critical review of manuscript; D.C. López-Medina and G. García: data acquisition, interpretation of results, and critical review of manuscript; A. Teijeiro, R. Casal-Fernández, and C. Candal-Pedreira: interpretation of results and critical review of manuscript; L. Varela-Lema and A. Ruano-Ravina: conception, interpretation of results, and critical review of manuscript; M. Pérez-Ríos: conceptualization, acquisition of funding, drafting and editing of manuscript. All authors have read and approved the final version of the manuscript.
CONFLICTS OF INTERESTThe authors declare that they have no conflicts of interest.