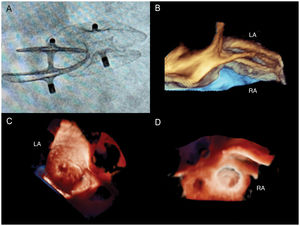
A 49-year-old woman presented at our clinic with a history of recurrent ischemic strokes. She had no known cardiovascular risk factors. Despite treatment with aspirin after the first episode in 2013, she was admitted again in 2017 with an acute infarction in the right middle cerebral artery territory, suggestive of an embolic etiology. No association was found with thrombophilia, autoimmune disorders, or vascular involvement. The electrocardiogram was normal, and a search for rhythm disorders with a prolonged Holter was unsuccessful. A transesophageal echocardiogram was performed, showing a prominent atrial septal aneurysm with 2 defects, one of them retroaortic (size 9mm) and the other posterior (size 4mm), with continuous left-to-right shunt. She underwent successful transcatheter closure with 2 overlapping devices, a 25mm patent foramen ovale occluder in the posterior orifice and an 11-mm atrial septal defect occluder in the anterior defect (figure 1A). Two months after intervention, a follow-up transesophageal echocardiogram with 3-dimensional echocardiographic transillumination rendering was performed. There was no residual shunt through the interatrial septum with color Doppler, and no images suggestive of thrombus on the devices. In figure 1B with 3-dimensional zoom mode, the atrial septal aneurysm is clearly trapped between both disks of the atrial septal defect device. In figure 1C Image acquired with MultiVue tool to achieve a perpendicular plane, 3-dimensional transillumination rendering and multiplanar reformatting show the overlapping devices seen from the left atrium (LA), and in figure 1D the view is from the right atrium (RA).
.
To Daniel Sanchez García, clinical applications echocardiography specialist (Philips, Spain).