Heart failure becomes more common with age and is the leading cause of hospitalization among people older than 75 years.1 The first month after hospitalization for heart failure is a critical period, with findings showing a 9.7% readmission rate for circulatory system diseases and a 10.4% mortality rate during readmission.2 The prognosis of older patients with heart failure is influenced by a range of variables, including the underlying cause of the failure, functional class, comorbidities, and, with particular relevance, certain geriatric syndromes.3 Few population-based studies have analyzed hospital readmissions for circulatory system diseases or in-hospital mortality among people older than 75 years in the first month after hospitalization for HF.
We conducted a retrospective observational study of all patients aged 75 years or older with a primary diagnosis of heart failure who were discharged from an acute care Spanish public hospital between 2016 and 2018. Diagnoses were determined through International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, and all patients were registered in the Spanish Minimum Data Set (MDS), which contains details of all hospital admissions within the Spanish national health system. We analyzed 30-day readmissions for circulatory diseases (ICD-10-CM, Chapter 9: Diseases of the Circulatory System) and mortality during these readmissions.
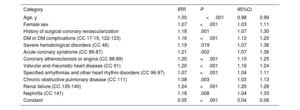
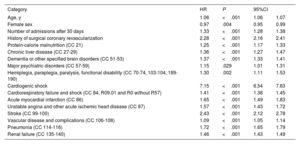
Data entries were analyzed for 178 523 patients (59.2% women) with a mean±standard deviation age of 85.1±5.5 years. The most common comorbidities were renal failure (40.9%), diabetes (34.3%), hypertension (32.9%), and valvular and rheumatic heart disease (31.4%). The crude 30-day readmission rate for circulatory system diseases was 9.6%, corresponding to a mean of 1.05 readmissions per patient. Predictors of readmission on multivariable analysis are shown in table 1. Overall, 34.5% of the patients died during readmission. When we included deaths occurring during readmission and the index episode, the 30-day mortality rate was 14.8%. The adjusted model for 30-day in-hospital mortality showed little discriminative ability (Harrell c index=0.66). The main predictors of in-hospital mortality are shown in table 2.
Predictors of readmission in the 30 days after hospitalization for heart failure in patients older than 75 years
| Category | IRR | P | 95%CI | |
|---|---|---|---|---|
| Age, y | 1.00 | <.001 | 0.98 | 0.99 |
| Female sex | 1.07 | <.001 | 1.03 | 1.11 |
| History of surgical coronary revascularization | 1.18 | .001 | 1.07 | 1.30 |
| DM or DM complications (CC 17-19, 122-123) | 1.16 | <.001 | 1.12 | 1.20 |
| Severe hematological disorders (CC 46) | 1.19 | .019 | 1.07 | 1.36 |
| Acute coronary syndrome (CC 86-87) | 1.21 | .002 | 1.07 | 1.36 |
| Coronary atherosclerosis or angina (CC 88-89) | 1.20 | <.001 | 1.15 | 1.25 |
| Valvular and rheumatic heart disease (CC 91) | 1.20 | <.001 | 1.16 | 1.24 |
| Specified arrhythmias and other heart rhythm disorders (CC 96-97) | 1.07 | <.001 | 1.04 | 1.11 |
| Chronic obstructive pulmonary disease (CC 111) | 1.08 | .003 | 1.03 | 1.13 |
| Renal failure (CC 135-140) | 1.24 | <.001 | 1.20 | 1.28 |
| Nephritis (CC 141) | 1.18 | .008 | 1.04 | 1.33 |
| Constant | 0.05 | <.001 | 0.04 | 0.06 |
CC, condition category; DM, diabetes mellitus; IRR, incidence rate ratio.
Predictors of mortality in the 30 days after hospitalization for heart failure in patients older than 75 years
| Category | HR | P | 95%CI | |
|---|---|---|---|---|
| Age, y | 1.06 | <.001 | 1.06 | 1.07 |
| Female sex | 0.97 | .004 | 0.95 | 0.99 |
| Number of admissions after 30 days | 1.33 | <.001 | 1.28 | 1.38 |
| History of surgical coronary revascularization | 2.28 | <.001 | 2.16 | 2.41 |
| Protein-calorie malnutrition (CC 21) | 1.25 | <.001 | 1.17 | 1.33 |
| Chronic liver disease (CC 27-29) | 1.36 | <.001 | 1.27 | 1.47 |
| Dementia or other specified brain disorders (CC 51-53) | 1.37 | <.001 | 1.33 | 1.41 |
| Major psychiatric disorders (CC 57-59) | 1.15 | .029 | 1.01 | 1.31 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 70-74, 103-104, 189-190) | 1.30 | .002 | 1.11 | 1.53 |
| Cardiogenic shock | 7.15 | <.001 | 6.54 | 7.83 |
| Cardiorespiratory failure and shock (CC 84, R09.01 and R0 without R57) | 1.41 | <.001 | 1.38 | 1.45 |
| Acute myocardial infarction (CC 86) | 1.65 | <.001 | 1.49 | 1.83 |
| Unstable angina and other acute ischemic heart disease (CC 87) | 1.57 | <.001 | 1.43 | 1.72 |
| Stroke (CC 99-100) | 2.43 | <.001 | 2.12 | 2.78 |
| Vascular disease and complications (CC 106-108) | 1.09 | <.001 | 1.05 | 1.14 |
| Pneumonia (CC 114-116) | 1.72 | <.001 | 1.65 | 1.79 |
| Renal failure (CC 135-140) | 1.46 | <.001 | 1.43 | 1.49 |
CC, condition category; HR, hazard ratio.
The main conclusions that can be drawn from this study are that older patients with heart failure have a) a high frequency of cardiovascular and noncardiovascular comorbidities that increase the short-term risk of events, b) a high 30-day readmission rate for diseases of the circulatory system (9.6%) and c) a high crude 30-day mortality rate (14.8%).
Older patients with heart failure are particularly vulnerable in the month following discharge from hospital, with findings showing a particularly high risk of readmission in the first week. The time required for maximum risk to decline by 50% is 38 days for readmission and 11 days for mortality.4 Increased mortality risk appears to be associated with admission-related factors, such as comorbidities and geriatric syndromes, while increased readmission risk seems to be more closely linked to indirect factors, such as social support, cognition, medication, and above all, poor care transition.5 Age was not a significant predictor of readmission in our series. The main predictors of mortality were acute cardiovascular events during the index admission, such as cardiogenic shock and stroke, and the number of readmissions in the first month.
The STOP-HF study has shown that close follow-up in the first month after hospitalization for heart failure reduces early readmissions in frail older patients.6 Although we cannot draw conclusions on this possibility based on our study design, the inclusion of older patients in multidisciplinary heart failure care programs may help improve the poor outcomes evident in the real-world population-based data analyzed.
Our study has some limitations inherent to the use of administrative data from the MDS database. In our analysis of 30-day mortality rates, we may have missed some deaths that occurred at home or outside the public hospital setting, but we expect there will have been few cases. In addition, these limitations will have been offset by the strengths of the MDS, which is a widely validated, exhaustive database containing codes for multiple clinical conditions and details of all public hospital admissions in Spain.
FundingNo funding.
Authors’ ContributionsStudy design and manuscript preparation: A. Esteban-Fernández, M. Anguita-Sánchez, J.L. Bernal. Data checks and statistical analysis: N. Rosillo, N. del Prado, J.L. Bernal. Manuscript review, revision, and approval: all authors.
Conflicts of InterestThe authors declare that they have no conflicts of interest in relation to this study.