To the Editor:
Effusive-constrictive pericarditis (ECP) is a rare form of pericardial syndrome, where cardiac constriction occurs in the presence of significant pericardial effusion.1 Patients present cardiac tamponade, although post-pericardiocentesis symptoms persist, thus revealing cardiac constriction which is resolved only after pericardiectomy.2 Although the condition was first described some years ago, only a few cases have been reported in the medical literature.3,4 We present a case of ECP in a patient with a history of mitral valve replacement.
A 55-year-old man with mitral valve replacement in 1998 and postpericardiotomy syndrome, characterized by fever and tiredness with minimal effort; following this treatment, the patient remained asymptomatic. In April 2004, he was seen for severe pericardial effusion and cardiac tamponade that required pericardiocentesis. Afterwards, he initially remained asymptomatic. He was readmitted in July 2004 and reported that he felt well after hospital discharge, but a few weeks later, began to feel tired after considerable exertion, and then with only moderate effort. At the time of readmission, the patient's blood pressure was 110/70 mm Hg; there was no paradoxical pulse, but the jugular vein was enlarged. Cardiac auscultation was rhythmic at 70 bpm and prosthetic sounds were normal. He presented slight hepatomegaly and edema with fovea in the lower extremities.
The electrocardiogram showed sinus rhythm. The echocardiogram disclosed a protodiastolic septal notch, restrictive transmitral flow, and respiratory variation in mitral E wave velocity. The artificial valve was functioning normally.
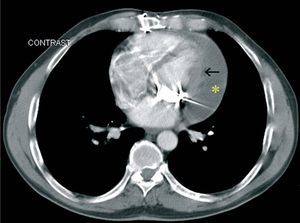
The chest computed tomography scan showed moderate, predominantly posterolateral, pericardial effusion with pericardial thickening (Figure 1).
Figure 1. Chest computed tomography: moderate, primarily posterolateral, pericardial effusion (asterisk), and pericardial thickening (arrow).
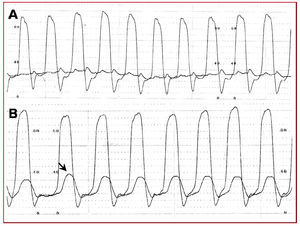
We suspected pericardial constriction and requested right and left catheterization. We also observed equalization of end-diastolic pressures in the right and left chambers. The diastolic pressure curve of the left ventricle showed the typical "square root" or "dip-plateau" morphology (Figure 2).
Figure 2. Catheterization. A: LV curve with diastolic dip-plateau and right atrial curve (equalized diastolic pressures). B: left (LV) and right (RV) ventricular pressure curve (equalized diastolic pressures). LV-RV pressure discordance during inspiration (arrow).
Based on a diagnosis of ECP (probably idiopathic), pericardiectomy was performed. The histologic study showed hyalinized fibrous tissue and lymphoplasmocytic infiltrate, consistent with a chronic inflammatory response. Clinical progress was favorable.
Whenever a patient presents right heart failure that is not explained by systolic dysfunction, valve disease, or right heart disease, ECP should be suspected. A differential diagnosis with cardiomyopathy is essential, since ECP presents relief of postpericardiectomy symptoms. Visualization of pericardial thickening or calcification on imaging studies is extremely helpful in the diagnosis.5
On echocardiography, ECP shows reciprocal respiratory changes between both ventricles.6,7 Cardiac catheterization reveals an increase and equalization of end-diastolic pressures, reciprocal postinspiratory changes6,7 (Figure 2, arrow), and left ventricular dip-plateau morphology.
Effusive-constrictive pericarditis simultaneously presents pericardial effusion with hemodynamic compromise and pericardial constriction. The diagnosis is established postpericardiocentesis, if the patient does not have complete symptomatic relief and manifests constriction,2 as in the case we present. The importance of the diagnosis lies in the need for resection of the visceral pericardium. Pericardiectomy is the treatment of choice in symptomatic patients.