The STructured multidisciplinary outpatient clinic for Old and frail Post-discharge patients hospitalized for heart failure (STOP-HF Clinic) study was designed to reduce 30-day readmission rates and to facilitate the transition to primary care of vulnerable patients recently admitted for acutely decompensated heart failure (HF).1 The interventions performed in the STOP-HF Clinic study have recently been reported.1 In summary, this was a prospective study including 518 patients (age 82 years; Barthel score, 70; Charlson index, 5.6) and starting 4.9±2 days after discharge. The STOP-HF Clinic study is a 1-month intervention (up to 2-3 months in very specific cases) that included a number of actions ranging from health literacy, early reassessment, increased quality of medical management, with intravenous therapies if needed, and personalized transition of care. The efficacy of the STOP-HF Clinic was confirmed, examining its 30-day impact with the official readmission data registry of the Catalan Health Service (CatSalut), which provides medical care to 7.5 million people in Catalonia, Spain. We reported a ∼ 50% reduction in the all-cause 30-day readmission rate after an index hospitalization for HF, mainly driven by the reduction in HF-related readmissions.
Whether an early postdischarge intervention, such as the STOP-HF Clinic, may have an impact on subsequent readmissions in the following year remained to be determined. Accordingly, our aim was to assess the 1-year readmission rate of the STOP-HF Clinic cohort and to compare, as a natural experiment, the 1-year readmission rate of the STOP-HF referral area against that of a control group comprising the patients in the remainder of the CatSalut area. For this long-term analysis, the primary endpoint was HF-related rehospitalization at 1 year. We also addressed all-cause death and the composite endpoint of all-cause death or HF-related hospitalization in the on-site cohort. At 1-year, 151 (29.2%) patients were readmitted at least once for HF (with a total of 204 hospitalizations) and 128 (24.7%) died; the composite endpoint occurred in 216 patients (41.7%).
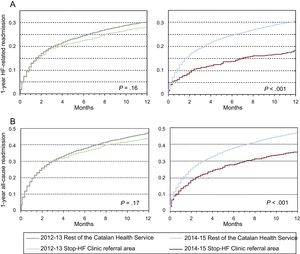
Readmission rates within the STOP-HF referral area (∼ 250 000 people) were compared with those of the CatSalut registry (∼ 7.5 million people) during 2 time periods: pre-STOP-HF (2012-2013) and post-STOP-HF (2014-2015). The 1-year HF-related readmission rates were significantly lower in the STOP-HF referral area than in the CatSalut registry in the 2014 to 2015 period (P<.001), whereas they were nonsignificantly different in the 2012 to 2013 period (Table). Indeed, in the 2014 to 2015, period a 36% reduction in 1-year HF-related hospitalizations in the STOP-HF referral area was observed, while rehospitalizations remained unchanged in the CatSalut registry. The Figure shows the probability actuarial curves of HF-related readmissions (Figure A) and all-cause readmissions (Figure B) after an index HF hospitalization within the CatSalut area and the STOP-HF referral area. Compared with the rest of the CatSalut area, the STOP-HF referral area showed a significant decline in HF readmissions during the 2014 to 2015 period, with the 2 curves following diverging paths starting before the first month and up to the 1-year follow-up (P <.001 using the Wilcoxon-Gehan test). All-cause 1-year readmissions showed a similar trend; of note, this was only driven by the reduction in HF-related readmissions, as non–HF-related readmissions remained similar in the 2 study periods (Table). This reduction in 1-year HF-related hospitalizations in the STOP-HF referral area was not related to an increase in mortality (31.3% vs 28.6%, P=.15).
CatSalut Population-based Data During the 2 Study Periods
| Index admission 2012-2013 period | |||
|---|---|---|---|
| STOP-HF referral area | Catalan Health Service | P | |
| Total index HF admissions | 1251 | 30995 | |
| All-cause 1-year readmissions | 522 (41.7) | 13272 (42.8) | .449 |
| HF-related | 293 (23.4) | 7754 (25.0) | .206 |
| Non–HF-related | 229 (18.3) | 5518 (17.8) | .410 |
| Index admission 2014-2015 period | |||
|---|---|---|---|
| STOP-HF referral area | Catalan Health Service | P | |
| Total index HF admissions | 1296 | 31383 | |
| All-cause 1-year readmissions | 416 (32.1) | 12925 (41.2) | <.001 |
| HF-related | 193 (14.9) | 7644 (24.4) | <.001 |
| Non–HF-related | 223 (17.2) | 5281 (16.8) | .681 |
Discharges with a primary diagnosis of chronic disease not involving the circulatory system and having no external cause, and readmissions due to a complication of the index admission.
HF, heart failure; HF-related, recurrence of heart failure; Non HF-related, nonrecurrence of heart failure.
Data are expressed as No. or No. (%).
Actuarial curves of the probability of 1-year readmission in the STOP-HF referral area vs the CatSalut area before STOP-HF (2012-2013) and with STOP-HF (2014-2015).
A: Heart failure-related readmission. B: All-cause readmission.
P values reflect comparisons between the study groups.
HF, heart failure; STOP-HF, STructured multidisciplinary outpatient clinic for Old and frail Post-discharge patients hospitalized for Heart Failure.
What is the most likely explanation for the long-term impact of such a short-term intervention? Three main mechanisms are proposed and discussed. First, when a prolonged strategy is not feasible–or cost-efficient–to be carried out over time, the number and the intensity of the actions included may play an essential role in the program's success. Considering an aging population such as ours, holistic management may be a key issue. Indeed, Saleh et al.2 analyzed elderly Medicare beneficiaries randomized to receive a 45-day intervention including 5 activities, and the 1-year readmission analysis revealed that control participants were more likely to be readmitted than intervention participants (58.2% vs 48.2%) with a favorable cost-benefit analysis. A recent example of the benefits of comprehensive and multidisciplinary interventions (a 1 year-long intervention) is the Integrated Management Units for Patients with HF (UMIPIC) program,3 which obtained a very significant reduction in 1-year HF readmissions when compared with the previous year. By contrast, time-limited but less broad interventions were unsuccessful in reducing mid- and long-term outcomes. Second, by acting during the most vulnerable phase, we may have been most effective. Indeed, the concept “hospitalization begets hospitalization” is currently well recognized. Thus, by reducing early-stage hospitalizations, we may be acting on subsequent hospitalizations, and this is of the utmost importance for patients’ quality of life and for the sustainability of the health care system. Finally, an integrated approach that facilitates the transition to primary care management with a written medical report and drug prescription information transferred to the primary care physician very likely prolongs adequate patient management, keeping the patient within the “radar” of the health care system.
In conclusion, in a real-life, prospective, all-comers study that enrolled old, frail and vulnerable patients, an early short-term strategy aiming to reduce 30-day readmission rates remained beneficial up to 1-year, largely driven by HF-related readmissions.
.