Individuals with long COVID may exhibit alterations in heart rate (HR), including an elevated resting HR (rest-HR) or diminished HR variability, among other abnormalities. These perturbations in HR dynamics are believed to be linked to underlying autonomic dysfunction and are associated with higher self-reported symptoms.1,2
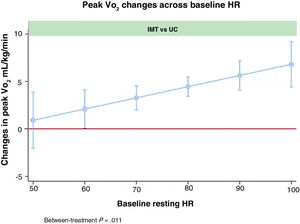
Under normal physiological conditions, the diaphragm plays a pivotal role in modulating HR variability and regulating sympathetic tone.3 Previous evidence has suggested that improved muscle function may have a beneficial effect on cardiovascular function and the re-establishment of sympathovagal balance facilitated by ergoreflex modulation.4 Given these considerations, we hypothesized that, in long COVID individuals with higher baseline sympathetic tone surrogates, improved respiratory muscle function through inspiratory muscle training (IMT) may further enhance tolerance to physical activity by regulating sympathetic activation and cardiovascular stress. In this post hoc substudy of the InsCOVID trial, we aimed to assess the influence of rest-HR on responsiveness to a 12-week IMT program in terms of peak oxygen consumption (peak VO2) among patients with long COVID.
The InsCOVID trial was a randomized clinical trial conducted at a single center with blinded assessors and 26 patients with long COVID. The trial investigated the impact of a 12-week home-based IMT vs usual care (UC) on peak VO2 in individuals with prolonged symptoms postsevere acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia hospitalization. The design and primary outcomes of the trial were registered at Clinical Trials (NCT05279430) and have been previously published.5,6 Informed consent was obtained from all participants, and the trial was approved by the local research ethics committee following the Declaration of Helsinki and national regulations.
The inclusion criteria for participant enrollment were: a) symptomatic adults previously admitted due to SARS-CoV-2 pneumonia; b) a minimum of 3 months since discharge; and c) provision of informed consent. The main exclusion criteria encompassed: a) the inability to undergo maximal baseline cardiopulmonary exercise testing (CPET); b) structural heart disease, valve heart disease or diastolic dysfunction estimated by 2-dimensional echocardiography; c) significant pulmonary disease; d) the presence of angina or ischemia during CPET; e) chronic kidney disease (glomerular filtration rate <60mL/min/1.73 m2); f) anemia (hemoglobin level of <12g/dL in women and <13g/dL in men); and g) treatment with negative chronotropic drugs or individuals with a pacemaker.
The IMT intervention commenced with an initial diaphragmatic breathing instruction using a threshold inspiratory muscle trainer. Subsequently, patients participated in a home-based training regimen involving 2 daily 20-minute sessions over 12 weeks at a resistance level set at 25% to 30% of their maximal inspiratory pressure. Weekly assessments by a physiotherapist allowed adjustments to be made to resistance settings.
Maximal functional capacity was evaluated using incremental and symptom-limited CPET on a bicycle ergometer. HR was assessed at rest and peak effort (peak-HR). The HR response during CPET was evaluated following the chronotropic index (CIx) formula=peak-HR-rest-HR/ [(220-age)-rest-HR)].
We used a linear mixed regression model to analyze between-treatment changes in peak VO2. Baseline age, sex, hemoglobin, body mass index (BMI), baseline maximal inspiratory pressure, and the baseline values of peak VO2 were included as covariates. All analyses were performed with STATA 17.0 (StataCorp LP, College Station, United States).
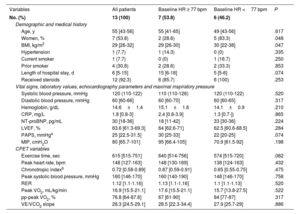
There were no significant differences across treatment arms at baseline in the InsCOVID trial.6 Baseline characteristics across median baseline rest-HR among patients assigned to the IMT arm are presented in table 1. The median age was 55 (43-56) years, with 46.2% of the participants being women. Overall, patients with a higher rest-HR were predominantly men and showed lower BMI, with no other significant differences.
Baseline characteristics of patients who receive d IMT stratified by median baseline heart rate.
| Variables | All patients | Baseline HR ≥ 77 bpm | Baseline HR <77 bpm | P |
|---|---|---|---|---|
| No. (%) | 13 (100) | 7 (53.8) | 6 (46.2) | |
| Demographic and medical history | ||||
| Age, y | 55 [43-56] | 55 [41-65] | 49 [43-56] | .617 |
| Women, % | 7 (53.8) | 2 (28.6) | 5 (83.3) | .048 |
| BMI, kg/m2 | 29 [26-32] | 29 [26-30] | 30 [22-38] | .047 |
| Hypertension | 1 (7.7) | 1 (14.3) | 0 (0) | .335 |
| Current smoker | 1 (7.7) | 0 (0) | 1 (16.7) | .250 |
| Prior smoker | 4 (30.8) | 2 (28.6) | 2 (33.3) | .853 |
| Length of hospital stay, d | 6 [5-15] | 15 [6-18] | 5 [5-6] | .074 |
| Received steroids | 12 (92.3) | 6 (85.7) | 6 (100) | .253 |
| Vital signs, laboratory values, echocardiography parameters and maximal inspiratory pressure | ||||
| Systolic blood pressure, mmHg | 120 (110-122) | 110 (110-126) | 120 (110-122) | .520 |
| Diastolic blood pressure, mmHg | 60 [60-66] | 60 [60-70] | 60 [60-65] | .317 |
| Hemoglobin, g/dL | 14.6±1.4 | 15.1±1.6 | 14.1±0.9 | .210 |
| CRP, mg/L | 1.8 [0.8-3] | 2.4 [0.8-3.9] | 1.3 [0.7-]) | .865 |
| NT-proBNP, pg/mL | 30 [18-36] | 18 [11-42] | 33 [30-36] | .224 |
| LVEF, % | 63.6 [61.3-69.3] | 64 [62.6-71] | 62.5 [60.6-68.5] | .284 |
| PAPS, mmHga | 25 [22.5-31.5] | 30 [25-33] | 22 [20-25] | .074 |
| MIP, cmH2O | 80 [65.7-101] | 95 [66.4-105] | 70.9 [61.5-92] | .198 |
| CPET variables | ||||
| Exercise time, sec | 615 [515-751] | 640 [514-756] | 574 [515-720] | .082 |
| Peak heart rate, bpm | 148 [127-163] | 148 [130-169] | 138 [124-163] | .432 |
| Chronotropic indexb | 0.72 [0.58-0.89] | 0.87 [0.59-0.91] | 0.65 [0.55-0.75] | .475 |
| Peak systolic blood pressure, mmHg | 160 [146-170] | 160 [140-190] | 148 [146-170] | .758 |
| RER | 1.12 [1.1-1.16] | 1.13 [1.1-1.16] | 1.1 [1.1-1.13] | .520 |
| Peak VO2, mL/kg/min | 16.9 [15.5-21.1] | 17.6 [15.5-21.1] | 15.7 [13.8-27.5] | .522 |
| pp-peak VO2, % | 76.8 [64-87.6] | 67 [61-90] | 84 [77-87] | .317 |
| VE/VCO2 slope | 28.3 [24.5-29.1] | 28.5 [22.3-34.4] | 27.9 [25.7-29] | .886 |
BMI, body mass index; bpm, beats-per-minute; CPET, cardiopulmonary exercise testing; CRP, C-reactive protein; HR, heart rate; LVEF, left ventricle ejection fraction; MIP, maximal inspiratory pressure; NT-proBNP, N-terminal pro-B-type natriuretic peptide; PASP, pulmonary artery systolic pressure; peak VO2, peak oxygen consumption; pp-peak VO2, percent of predicted peak oxygen consumption; RER, respiratory exchange ratio; VE/VCO2, ventilatory efficiency.
The data are expressed as No. (%), mean±standard deviation, or median [interquartile range]. Baseline variables were compared among treatment groups with unpaired Student t test, Mann-Whitney U test, or chi-square test as appropriate.
Compared with patients in the UC group, those assigned to the IMT group exhibited an enhanced increment in peak VO2 at 12 weeks if they had a higher rest-HR at baseline (P value for between-treatment comparison=.011), as illustrated in figure 1.
Regarding HR response to treatment, a statistically significant increase was observed in both peak-HR and CIx (Δ+11.42; 95% confidence interval [95%CI], 0.33-22.5; P=.044 and Δ+0.13, 95%CI, 0.01-0.26; P=.046, respectively) in the IMT group compared with the UC group. No significant differences in treatment were observed at 12 weeks for rest-HR in the IMT group compared with the UC group (Δ-3.85; 95%CI,-15.8 to 8.06; P=.509).
The main finding of this substudy is that baseline rest-HR was related to maximal aerobic capacity response to IMT. Furthermore, we found significant improvement in HR response to exercise. Overall, our results highlight the role of IMT as a simple and valuable treatment for improving aerobic capacity in long COVID patients, especially in those with higher rest-HR. Notably, patients showing higher rest-HR and greater functional capacity improvement were mostly men with lower BMI. The current findings contribute important insights to previous work6 as they clarify which patients stand to benefit most from IMT.
Despite the lack of clear understanding regarding the precise mechanisms through which IMT enhances exercise capacity in individuals with long COVID, we postulate that IMT, facilitated by cardiac and peripheral autonomic modulation, may enhance HR response to exercise as well as the muscle ergoreflex,3,4 thus improving short-term exercise tolerance.
The main limitation of this post hoc substudy is its small sample size, which increases the risk of type II error and reduces statistical power for detecting significant effects. Nevertheless, the findings of the study provide valuable insights and warrant further investigation into the underlying pathophysiological mechanisms through which IMT enhances exercise tolerance in patients with long COVID and its potential application in other cardiovascular disorders.
FUNDINGThis work was partially supported by a grant from Sociedad Española de Cardiología, Investigación Clínica en Cardiología, Grant SEC 2021.
ETHICAL CONSIDERATIONSInformed consent was obtained from all participants, and the local research ethics committee approved the trial in accordance with the principles outlined in the Declaration of Helsinki and national regulations. Possible sex/gender biases have been considered in the preparation of this article.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence tool was used.
AUTHORS’ CONTRIBUTIONSAll authors have read and approved the manuscript.
CONFLICTS OF INTERESTNone.