Sudden cardiac death (SCD) in young, healthy people is an issue of medical and social concern.1 Echocardiography has become an important diagnostic tool in this setting, as it can detect certain preventable causes of SCD. A study of 2688 Spanish athletes (67% male; mean±standard deviation age, 21±10 years) found that 4 athletes had risk factors for SCD and 3 had a heart condition requiring specific treatment or follow-up.2 The aim of this study was to establish the percentile distribution of 6 echocardiographic measurements that could serve as reference values for assessing and monitoring competing athletes.
We studied 2574 consecutive athletes (81% male, 89.2% white) from different clubs in La Rioja, Spain who had undergone cardiological examination between September 2013 and June 2017. While 20 different sports were represented, 85.5% of the athletes were from just 4 sports: soccer (61.2%), basketball (17.3%), handball (4.1%), and athletics (2.6%). They had been training for an average of 6 years (range, 4-7 years). Forty-two athletes (2.1%) were excluded because they had a heart condition. All athletes underwent a full cardiological examination consisting of structured history taking, physical examination, a resting electrocardiogram, and a 2-dimensional echocardiogram3 (Vivid S5; General Electric Vingmed, USA). Body mass index and body surface area (BSA), calculated as body weight (kg)0.425×height (cm)0.725)×0.007184, were also measured. Percentile curves (P3 to P97) adjusted for age and sex were created using the lambda-mu-sigma (LMS) method in LMSchartmaker Pro, version 2.54 (Harlow Printing Limited, Tyne & Wear, UK). The coefficient of determination (R2) was used to assess goodness-of-fit based on the inverse logarithm of BSA and cardiac structure measurements adjusted for sex.
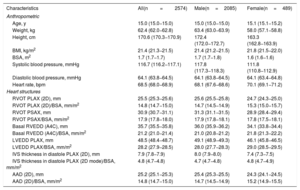
The athletes’ general characteristics and echocardiographic measurements are shown in table 1.
Athletes’ Characteristics.
| Characteristics | All(n=2574) | Male(n=2085) | Female(n=489) |
|---|---|---|---|
| Anthropometric | |||
| Age, y | 15.0 (15.0−15.0) | 15.0 (15.0−15.0) | 15.1 (15.1−15.2) |
| Weight, kg | 62.4 (62.0−62.8) | 63.4 (63.0−63.9) | 58.0 (57.1−58.8) |
| Height, cm | 170.6 (170.3−170.9) | 172.4 (172.0−172.7) | 163.3 (162.8−163.9) |
| BMI, kg/m2 | 21.4 (21.3−21.5) | 21.4 (21.2−21.5) | 21.8 (21.5−22.0) |
| BSA, m2 | 1.7 (1.7−1.7) | 1.7 (1.7−1.8) | 1.6 (1.6−1.6) |
| Systolic blood pressure, mmHg | 116.7 (116.2−117.1) | 117.8 (117.3−118.3) | 111.8 (110.8−112.9) |
| Diastolic blood pressure, mmHg | 64.1 (63.8−64.5) | 64.1 (63.8−64.5) | 64.1 (63.4−64.8) |
| Heart rate, bpm | 68.5 (68.0−68.9) | 68.1 (67.6−68.6) | 70.1 (69.1−71.2) |
| Heart structures | |||
| RVOT PLAX (2D), mm | 25.5 (25.3−25.6) | 25.6 (25.5−25.8) | 24.7 (24.3−25.0) |
| RVOT PLAX (2D)/BSA, mm/m2 | 14.8 (14.7−15.0) | 14.7 (14.5−14.9) | 15.3 (15.0−15.7) |
| RVOT PSAX, mm | 30.9 (30.7−31.1) | 31.3 (31.1−31.5) | 28.9 (28.4−29.4) |
| RVOT PSAX/BSA, mm/m2 | 17.9 (17.8−18.0) | 17.9 (17.8−18.1) | 17.8 (17.5−18.1) |
| Basal RVEDD (A4C), mm | 35.7 (35.5−35.8) | 36.0 (35.9−36.2) | 34.1 (33.8−34.4) |
| Basal RVEDD (A4C)/BSA, mm/m2 | 21.2 (21.0−21.4) | 21.0 (20.8−21.2) | 21.8 (21.3−22.2) |
| LVEDD PLAX, mm | 48.5 (48.4−48.7) | 49.1 (48.9−49.3) | 46.1 (45.8−46.5) |
| LVEDD PLAX/BSA, mm/m2 | 28.2 (27.9−28.5) | 28.0 (27.7−28.3) | 29.0 (28.5−29.5) |
| IVS thickness in diastole PLAX (2D), mm | 7.9 (7.8−7.9) | 8.0 (7.9−8.0) | 7.4 (7.3−7.5) |
| IVS thickness in diastole PLAX (2D mode)/BSA, mm/m2 | 4.8 (4.7−4.8) | 4.7 (4.7−4.8) | 4.8 (4.7−4.9) |
| AAD (2D), mm | 25.2 (25.1−25.3) | 25.4 (25.3−25.5) | 24.3 (24.1−24.5) |
| AAD (2D)/BSA, mm/m2 | 14.8 (14.7−15.0) | 14.7 (14.5−14.9) | 15.2 (14.9−15.5) |
2D, 2-dimensional; A4C, apical 4-chamber view; AAD, ascending aorta diameter; BMI, body mass index; BSA, body surface area; LVEDD, left ventricular end-diastolic diameter; IVS, interventricular septum; PLAX, parasternal long-axis view; PSAX, parasternal short-axis view; RVEDD, right ventricular end-diastolic diameter; RVOT, right ventricular outflow tract;
The AAD was measured in the tubular portion of the aorta.
IVS thickness in diastole was measured in PLAX.
Values presented as mean (95% confidence interval).
We observed a linear increase in percentiles (P3-P97) according to BSA for the 6 echocardiographic measurements analyzed (table 2). The association between BSA and all 6 measurements was linear (R2=0.11-0.31) but was strongest for left ventricular end-diastolic diameter (R2=0.29-0.31, P<.05).
Box-Cox power transformation values (L), median (M), coefficient of variation (S), and percentile distribution of echocardiographic measures according to body surface area (BSA) for both sexes
| BSA | L | S | p3 | p10 | p25 | p50 (M) | p75 | p90 | p97 | |
|---|---|---|---|---|---|---|---|---|---|---|
| RVOT PLAX, mm | 1.2-1.4 | 1.01 | 0.11 | 19.13 | 20.32 | 21.68 | 23.23 | 25.03 | 27.12 | 29.61 |
| 1.4-1.6 | 0.03 | 0.10 | 19.79 | 21.20 | 22.70 | 24.31 | 26.03 | 27.86 | 29.83 | |
| 1.6-1.8 | 0.94 | 0.10 | 20.35 | 21.98 | 23.60 | 25.24 | 26.88 | 28.53 | 30.19 | |
| 1.8-2.0 | 1.50 | 0.09 | 21.25 | 23.04 | 24.77 | 26.43 | 28.05 | 29.63 | 31.16 | |
| 2.0-2.2 | 1.78 | 0.09 | 22.10 | 23.96 | 25.72 | 27.38 | 28.97 | 30.50 | 31.97 | |
| > 2.2 | 1.98 | 0.08 | 23.43 | 25.33 | 27.10 | 28.76 | 30.33 | 31.82 | 33.25 | |
| RVOT PSAX, mm | 1.2-1.4 | -0.23 | 27.57 | 0.14 | 21.12 | 23.04 | 25.18 | 27.57 | 30.25 | 33.25 |
| 1.4-1.6 | 0.60 | 29.21 | 0.12 | 22.35 | 24.55 | 26.84 | 29.21 | 31.65 | 34.18 | |
| 1.6-1.8 | 1.43 | 30.84 | 0.11 | 23.70 | 26.17 | 28.55 | 30.84 | 33.06 | 35.22 | |
| 1.8-2.0 | 2.26 | 32.48 | 0.10 | 25.26 | 27.93 | 30.31 | 32.48 | 34.47 | 36.33 | |
| 2.0-2.2 | 3.10 | 34.11 | 0.08 | 27.14 | 29.85 | 32.13 | 34.11 | 35.88 | 37.48 | |
| > 2.2 | 3.93 | 35.74 | 0.07 | 29.42 | 31.95 | 34.00 | 35.74 | 37.27 | 38.63 | |
| Basal RVEDD (A4C), mm | 1.2-1.4 | 0.64 | 0.10 | 25.78 | 27.67 | 29.60 | 31.59 | 33.61 | 35.69 | 37.80 |
| 1.4-1.6 | 0.77 | 0.09 | 28.24 | 30.11 | 32.01 | 33.93 | 35.88 | 37.85 | 39.85 | |
| 1.6-1.8 | 1.19 | 0.08 | 30.09 | 31.96 | 33.81 | 35.64 | 37.46 | 39.26 | 41.04 | |
| 1.8-2.0 | 1.90 | 0.07 | 31.36 | 33.37 | 35.27 | 37.09 | 38.82 | 40.49 | 42.10 | |
| 2.0-2.2 | 2.40 | 0.07 | 31.95 | 34.04 | 35.95 | 37.74 | 39.41 | 40.99 | 42.49 | |
| > 2.2 | 2.57 | 0.08 | 32.71 | 34.85 | 36.81 | 38.61 | 40.29 | 41.87 | 43.36 | |
| RVEDD PLAX, mm | 1.2-1.4 | 0.58 | 0.07 | 37.35 | 39.09 | 40.95 | 42.96 | 45.13 | 47.49 | 50.04 |
| 1.4-1.6 | 0.03 | 0.07 | 40.38 | 42.23 | 44.18 | 46.21 | 48.34 | 50.58 | 52.92 | |
| 1.6-1.8 | 0.90 | 0.06 | 42.53 | 44.52 | 46.52 | 48.53 | 50.55 | 52.57 | 54.61 | |
| 1.8-2.0 | 2.80 | 0.06 | 44.12 | 46.48 | 48.64 | 50.64 | 52.51 | 54.27 | 55.93 | |
| 2.0-2.2 | 4.72 | 0.05 | 45.52 | 48.29 | 50.57 | 52.53 | 54.24 | 55.78 | 57.17 | |
| > 2.2 | 6.53 | 0.05 | 46.62 | 49.85 | 52.22 | 54.12 | 55.70 | 57.07 | 58.28 | |
| Myocardial wall thickness, mm | 1.2-1.4 | 0.34 | 0.11 | 5.49 | 5.90 | 6.35 | 6.84 | 7.39 | 7.99 | 8.66 |
| 1.4-1.6 | 0.32 | 0.15 | 5.82 | 6.25 | 6.73 | 7.25 | 7.83 | 8.47 | 9.18 | |
| 1.6-1.8 | 0.30 | 0.15 | 6.14 | 6.59 | 7.09 | 7.64 | 8.25 | 8.93 | 9.67 | |
| 1.8-2.0 | 0.31 | 0.12 | 6.41 | 6.88 | 7.40 | 7.98 | 8.61 | 9.31 | 10.10 | |
| 2.0-2.2 | 0.31 | 0.12 | 6.61 | 7.10 | 7.63 | 8.23 | 8.88 | 9.61 | 10.41 | |
| > 2.2 | 0.33 | 0.13 | 6.78 | 7.29 | 7.84 | 8.45 | 9.12 | 9.87 | 10.69 | |
| Ascending aorta diameter, mm | 1.2-1.4 | 1.80 | 0.10 | 19.45 | 20.50 | 21.71 | 23.16 | 24.91 | 27.09 | 29.90 |
| 1.4-1.6 | 1.04 | 0.07 | 20.20 | 21.32 | 22.56 | 23.97 | 25.57 | 27.40 | 29.52 | |
| 1.6-1.8 | 0.51 | 0.09 | 21.15 | 22.31 | 23.58 | 24.95 | 26.45 | 28.08 | 29.88 | |
| 1.8-2.0 | 0.21 | 0.08 | 21.95 | 23.18 | 24.49 | 25.89 | 27.39 | 29.00 | 30.72 | |
| 2.0-2.2 | 0.03 | 0.08 | 22.52 | 23.86 | 25.28 | 26.77 | 28.35 | 30.02 | 31.79 | |
| > 2.2 | 0.38 | 0.09 | 22.98 | 24.47 | 26.02 | 27.63 | 29.29 | 31.02 | 32.81 |
A4C, apical 4-chamber view; BSA, body surface area; LVEDD, left ventricular end-diastolic diameter; p, percentile; PLAX, parasternal long-axis view; PSAX, parasternal short-axis view; RVEDD, right ventricular end-diastolic diameter; RVOT, right ventricle outflow tract.
Our findings could contribute to the detection of potentially serious cardiac abnormalities in young athletes and identify athletes requiring cardiology follow-up or treatment. Our findings are similar to those of a study of competing child and adolescent athletes, but we analyzed a larger sample and more right ventricle echocardiographic measurements.4 As expected, the absolute chamber dimensions observed in our study are lower than those reported for elite athletes.5 Once adjusted for BSA, however, they are similar.
Generally speaking, the increase observed in cardiac dimensions according to BSA is consistent with the available evidence. However, discrepancies between our findings and others may partly be due to differences in type of sport, training characteristics, years of training, age, race, and sex. In addition, echocardiographic measurements, like all measurements, are prone to interobserver and intraobserver variability, and technical difficulties associated with echocardiographic image acquisition have been reported by various research centers.
One of the main limitations of our study is the absence of a control group (noncompeting adolescents) with which to compare our results. Our findings are, however, similar to those reported by several studies that did not use a control group either.6 Because of the cross-sectional nature of our study, we are unable to establish a causal link between our findings and numerous aspects, such as type of training, sporting history, and “possible” adaptations of the heart to training. Information on hours spent training every week might have allowed us to detect differences in heart chamber structures and diameters between athletes participating in different types of sport (eg, sport involving resistance and/or strength training or individual vs group sports). Finally, we did not stratify our results by sex, as female athletes accounted for just 20% of the study population.
In conclusion, this report of LMS values and percentile curves indexed to BSA should facilitate comparisons with similar populations to ours. A recent study found that 3 out of 4 white athletes who had died of SCD had arrhythmogenic cardiomyopathy on autopsy, highlighting the importance of echocardiographic screening as a diagnostic tool for incipient cardiomyopathy.6 Studies of this type are very important for determining whether enlarged cardiac structures are physiological (due to larger body size) or the result of adaptation to training and therefore potentially pathological. Our findings are noteworthy because they include 3 right ventricle measurements. The echocardiographic measurements presented for a large sample of young adolescent athletes could be useful for the detection of heart changes and cardiology follow-up.
FundingM Izquierdo is a recipient of a grant (PI17/01814) from the Spanish Ministry of Economy, Industry and Competitiveness (Instituto de Salud Carlos III, European Regional Development Fund). R Ramírez-Vélez is a recipient of a postdoctoral fellowship grant (420/2019) from Universidad Pública de Navarra.