In recent years, due to the therapeutic advances and the introduction of the “infarct code” for primary angioplasty, patient mortality in the acute phase of acute coronary syndrome (ACS) has decreased considerably.1 However, the high rate of further ischemic events after discharge shows the need for optimizing secondary prevention measures in these patients. Among the objectives, it is fundamental to reduce levels of low-density lipoprotein cholesterol (LDL-C) (to < 70mg/dL, as recommended in the 2016 European guidelines on dyslipidemia,2 or even < 55mg/dL according to the most recent guidelines from 20193). Because of the efficacy of the available lipid-lowering drugs (high-potency statins, ezetimibe, and proprotein convertase subtilisin/kexin type 9 inhibitors [PCSK9i]), this is also now feasible.
However, recent studies continue to show that dyslipidemia control, despite improvement in recent years, remains very poor. Specifically, after an ACS, several studies in US populations have shown that the percentage of patients who received high-intensity statins in 2007-2009 was very low: 21% at discharge and just 14% at 1 year,4 and that this proportion increased slightly in 2011 (24.8% at discharge) and in 2014 (57.5%).5 More than a third of the patients had LDL-C> 70mg/dL.4 These data, as well as the release of PCSK9i, prompted the Spanish Society of Cardiology (SEC) to publish a position document on the subject in 2016.6 The aim of our study was to analyze the attainment of lipid targets in the first year of follow-up after an ACS in Spain following the publication of this document.6
We selected 20 cardiology departments from secondary or tertiary hospitals (10 of each) in Spain. All the departments had catheterization laboratories and infarct code programs, and 40% had cardiac rehabilitation units. Patient follow-up and, therefore, treatment monitoring, was done either by cardiology or by primary care; 80% of the hospitals did not have established protocols. A cutoff target LDL-C < 70mg/dL was used, as this was the recommended target in the 2016 guidelines.2
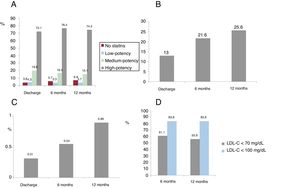
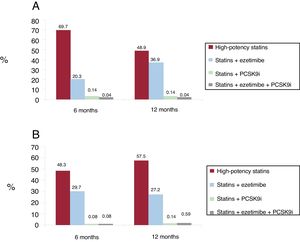
The study included 6364 patients (mean, 355 per hospital [range, 54-2254]),with a mean age of 73.3±10.6 years; 61.5% were men and 37.3% had diabetes. Figure 1 shows the lipid-lowering therapy used (figure 1A-C). At the time of discharge, 72.1% of patients received high-dose potent steroids (rosuvastatin 20 mg or atorvastatin 80 mg) and 24.1% received low- or medium-intensity statins, while just 3.8% received no statins (figure 1A). Thirteen percent received ezetimibe (figure 1B) and only 0.31% received PCSK9i (figure 1C). At 12 months, the percentage of patients receiving ezetimibe increased to 25.6%. Less than 1% of patients received PCSK9i. With these treatments, 61.1% of patients had LDL-C < 70mg/dL at 6 months and 55.9% at 12 months (figure 1D). Figure 2 shows the percentage of patients with LDL-C> 70 (figure 2A) or> 100mg/dL (figure 2B) and the different lipid-lowering treatments they were receiving. At 6 months, 30.3% of patients with LDL-C> 70mg/dL were not on high-potency statins, 79.9% were not on ezetimibe and only 0.14% were on PCSK9i; at 12 months, 51.5% of patients with LDL-C> 70mg/dL were not on high-potency statins, 63.1% were not on ezetimibe and only 0.04% were on PCSKi (figure 2A).
Lipid-lowering treatment received at discharge and at 6 and 12 months after acute coronary syndrome (ACS) in our study (A: statins; B: ezetimibe; C: PCSK9 inhibitors), and proportion of patients with low-density lipoprotein cholesterol (LDL-C) < 70mg/dL and < 100mg/dL at 6 and 12 months (D).
These study results, obtained in 2018, show improvements in the use of lipid-lowering drugs and LDL-C control after ACS. Only 20% to 25% of patients did not receive high-intensity statins in the first 12 months after ACS. The use of ezetimibe increased to 25% of patients at 12 months. This translated to close to 40% of patients having an LDL-C> 70mg/dL. Although it may not be possible to extrapolate these results nationally to all patients, they do indicate improved control of this problem. However, they also indicate that there remains much to be done, since a) up to 40% of patients did not meet the target LDL-C of < 70mg/dL (and this would increase substantially if we applied the current recommendations of LDL-C < 55mg/dL3); b) there is underuse of the available treatments, both the combination of statin+ezetimibe and particularly of PCSKi, whose use was minimal, and c) in 40% of patients with LDL-C higher than target levels, treatment was even further from the recommendations (figure 2). Better adherence to the scientific societies’ guidelines2,3,6 for these patients remains one of our greatest unmet challenges.
FUNDINGThis study was performed thanks to an unconditional grant from the Spanish Society of Cardiology.