To assess sex differences and the management of clinical problems in patients with atrial fibrillation through the use of care indicators.
MethodsOver a 5-month period, the study included all consecutive patients attended in the cardiology outpatient clinics of 2 tertiary hospitals with an atrial fibrillation episode or a clinical process due to atrial fibrillation.
ResultsA total of 533 patients were included (56.5% women; mean age, 70.5 ± 12.2 years), of whom 24.3% were younger than 65 years. Women had significantly more clinical problems and a higher stroke risk: CHADS2 (congestive heart failure, hypertension, age, diabetes, stroke [doubled]) (1.8 ± 1.2 vs 1.5 ± 1.1; P = .001) and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥ 75 [doubled], diabetes, stroke [doubled]-vascular disease and sex category [female]) (3.7 ± 1.4 vs 2.2 ± 1.4; P = .0001). Referrals to the cardiology department were appropriate in 94% of the patients, the referral source was primary care or other hospital services in 53.8%, and echocardiography was performed or recommended in 93.4%. Treatment (antiarrhythmics and anticoagulants) was administered according to guideline recommendations. In the previous 3 months, the Rosendaal index was 48.4 ± 37.4.
ConclusionsOne in every 4 patients seeking care for problems associated with atrial fibrillation are young; women have more clinical problems and seek care more frequently than men. Patients are correctly referred to the cardiology department and most are not referred from the emergency department. Echocardiography and antiarrhythmic and anticoagulant therapy were provided according to the recommendations of clinical practice guidelines. Vitamin K antagonists for anticoagulation therapy are underused.
Keywords
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice. In Spain, AF has a prevalence of 4.4% in the general population older than 40 years. The European clinical practice guidelines (CPGs) on AF emphasize the relationship between different risk factors and the onset of AF and the need to optimize the management of AF by controlling the rhythm or rate in each individual patient. They also recommend echocardiography and the optimal prevention of embolism using CHADS2 (congestive heart failure, hypertension, age, diabetes, stroke [doubled]and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥ 75 [doubled], diabetes, stroke [doubled]-vascular disease and sex category [female]) criteria and antiplatelet or anticoagulant drugs. The classic drugs of this type are vitamin K antagonists (VKA) or the direct anticoagulants (DAs) dabigatran, rivaroxaban, and apixaban.2
Many studies have highlighted the discrepancy between the routine treatment of patients with AF and the recommendations of the CPGs, an example being the underuse of recommended anticoagulation therapy. Previous studies have investigated this discrepancy3–6 in relation to previous guidelines, and the Spanish Society of Cardiology has undertaken a critical review of these guidelines.7
Currently, care indicators are available (derived from the recommendations of the CPGs) that can be used to assess the management of patients with AF. In 2010, we found significant sex differences in the characteristics of patients with AF treated in our outpatient cardiology department. The aim of this study was to determine the real-world treatment of AF in our setting 4 years later, assess sex differences, and evaluate how the CPG have influenced treatment in daily clinical practice.6
METHODSThe study was organized by the cardiology departments of 2 tertiary hospitals (A and B) in collaboration with the Research Agency of the Spanish Society of Cardiology. Care indicators were used to assess patient management in outpatient cardiology departments either due to an AF episode prompting a visit to the emergency room or due to a medical problem caused by AF. Patients could not be part of any other study conducted by the Research Agency of the Spanish Society of Cardiology. The study prospectively included all patients consecutively seen in cardiology departments because of an AF episode or a clinical problem caused by the arrhythmia. We excluded all patients with AF who visited the cardiology departments for a regular check-up and showed no clinical changes. Given that 70% of patients with AF sought medical attention for acute arrhythmia symptoms, or complications of the arrhythmia or the treatment (93% in recent-onset episodes), the study focused on clinical problems. A clinical problem was defined as any event resulting from a change of rhythm in AF: first detected AF, recurrence, fast rhythms, and slow rhythms. We included only 1 episode per patient and excluded any second episodes, if produced. Patients were included according to the recommendations of the ethics committees of both hospitals; the database excluded any information that could lead to patient identification. A patient was considered to have AF when the arrhythmia was confirmed by the electrocardiographic recording performed in the cardiology department, or when AF was documented in the record provided by the patient or the hospital report. All the cardiologists who worked in outpatient departments participated in the study; patients were recruited using a competitive enrolment strategy.
Data collection without any pharmacological intervention entailed the Spanish Agency for Medicines and Health Products classifying the registry as a Post-Authorization Study using designs other than prospective follow-up (EPA-OD) with the SEC-ACO-2013-01 code.
Main ObjectiveTo analyze the clinical characteristics of patients with AF, the management of antiarrhythmic treatment, and treatment to prevent embolic events and readmissions, and to evaluate sex differences.
Secondary ObjectivesTo determine the epidemiological characteristics and possible sex differences in AF patients visiting cardiology outpatient departments. To identify the risk factors for embolism in patients with AF and analyze the prevalence of each factor. To identify the prescribed treatment and adherence to the CPGs, particularly with regard to prescription of anticoagulant and antiarrhythmic drugs.
Online Data Collection FormPatients were included via an online data collection form designed with the assistance of the Spanish Society of Cardiology. The form collected all clinical data, their source, the approach in the emergency department to AF patients, and the treatment received by the patient prior to arrival at the cardiology department. International normalized ratio (INR) values 3 months prior to the hospital visit were collected from patients taking VKAs to calculate the time in therapeutic range (TTR) using the Rosendaal method, measuring the days within the therapeutic range and dividing by the total number of days that the patient was taking anticoagulants. Rhythm on ECG was documented at the time of the hospital visit and the AF was classified according to clinical patterns established by the CPGs. Ischemia was defined as a depressed ST segment or a deeply inverted T wave on electrocardiogram with ischemic characteristics accompanied by typical clinical characteristics. Prior AF episodes or hospital admissions were documented when confirmed by the relevant clinical report. Data were recorded on the physician's use of echocardiography at the clinic in patients with AF, therapeutic recommendations, and referral at patient discharge.
Care IndicatorsOutpatient care for patients with AF involves various aspects that should be assessed to improve the quality of care: a) referral source and the opinion of the treating cardiologist on the appropriateness of the referral (yes/no); we considered a referral to be appropriate when the patient actually had a clinical problem (regardless of whether the patient attended the emergency department or not) that led to treatment of the AF episode by a cardiologist; we considered a referral to be inappropriate when the patient was referred for a clinical problem that was later ruled out and the cardiologist did not change his or her approach to the AF episode; b) the performance of echocardiography in patients with AF; c) the treatment received by the patient in the cardiology department, and d) the use of treatments for embolism prevention, anticoagulation therapy with VKAs assessed by TTR, and the reasons given by cardiologists for not using these treatments.
Sample Size and Study DurationIn 2013, over 50 000 patients were seen in outpatient cardiology clinics of the 2 hospitals, of whom 24 958 were first visits from primary care, the emergency departments of both hospitals, or referrals from other specialties: In total, 14 183 patients attended hospital A and 10 775 patients attended hospital B. The prevalence of AF was 21% in patients attending our cardiology departments, of whom 23.7% had de novo AF and an unknown percentage of the remainder had decompensated AF. We estimated that 5% of all our patients could be included in the registry.6 A sufficiently large number of patients had to be included to ensure the robustness of the statistical analysis. The sample had an alpha risk < 0.5 and an accuracy of 5% for calculating the size of the sample. Assuming 5% of patients would be lost, it was estimated that the number of patients included in our 2010 study would have to be tripled. Beginning on March 1, 2014, more than 500 patients were included over a 3-month period.
Statistical AnalysisQuantitative variables with a normal distribution are expressed as mean ± standard deviation; the Student t test was used for their analysis. The chi-square test or, if needed, Fisher's exact test was used to compare qualitative variables by sex or type of AF. A P value of < .05 was used as a cutoff for statistical significance. The data were analyzed using SPSS version 15.0 (SPSS, Inc.; Chicago, Illinois, United States).
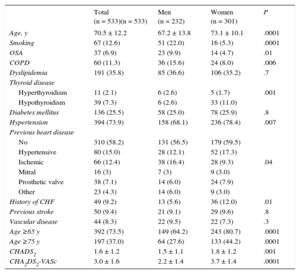
RESULTSFrom February 1, 2014 to June 30, 2014, 14 cardiologists from both hospitals included 533 patients in the registry. Further inclusion was suspended because the target of including more than 500 patients had been achieved. All patients underwent electrocardiogram in the cardiology department or were referred from the emergency department, where AF was documented (CPG class I/level B). During this 5-month period, 12 381 patients attended cardiology departments, of whom 4.3% were included. Mean age was 70.5 ± 12.2 (20-93) years, 16 patients (3%) were younger than 40 years, 114 (21.3%) were aged 40 to 65 years, and there were more women than men (301 [56.5%] women vs 232 men [43.5%]). There were significant differences between sexes in clinical characteristics; age, smoking, presence of obstructive sleep apnea, chronic obstructive pulmonary disease, thyroid disease (predominantly hypothyroidism), and hypertension. The prevalence of heart failure was higher in women, and significant differences between sexes were observed in previous heart disease (Table 1).
Clinical Characteristics of the Population by Sex
| Total (n = 533)(n = 533) | Men (n = 232) | Women (n = 301) | P | |
|---|---|---|---|---|
| Age, y | 70.5 ± 12.2 | 67.2 ± 13.8 | 73.1 ± 10.1 | .0001 |
| Smoking | 67 (12.6) | 51 (22.0) | 16 (5.3) | .0001 |
| OSA | 37 (6.9) | 23 (9.9) | 14 (4.7) | .01 |
| COPD | 60 (11.3) | 36 (15.6) | 24 (8.0) | .006 |
| Dyslipidemia | 191 (35.8) | 85 (36.6) | 106 (35.2) | .7 |
| Thyroid disease | .001 | |||
| Hyperthyroidism | 11 (2.1) | 6 (2.6) | 5 (1.7) | |
| Hypothyroidism | 39 (7.3) | 6 (2.6) | 33 (11.0) | |
| Diabetes mellitus | 136 (25.5) | 58 (25.0) | 78 (25.9) | .8 |
| Hypertension | 394 (73.9) | 158 (68.1) | 236 (78.4) | .007 |
| Previous heart disease | .04 | |||
| No | 310 (58.2) | 131 (56.5) | 179 (59.5) | |
| Hypertensive | 80 (15.0) | 28 (12.1) | 52 (17.3) | |
| Ischemic | 66 (12.4) | 38 (16.4) | 28 (9.3) | |
| Mitral | 16 (3) | 7 (3) | 9 (3.0) | |
| Prosthetic valve | 38 (7.1) | 14 (6.0) | 24 (7.9) | |
| Other | 23 (4.3) | 14 (6.0) | 9 (3.0) | |
| History of CHF | 49 (9.2) | 13 (5.6) | 36 (12.0) | .01 |
| Previous stroke | 50 (9.4) | 21 (9.1) | 29 (9.6) | .8 |
| Vascular disease | 44 (8.3) | 22 (9.5) | 22 (7.3) | .3 |
| Age ≥65 y | 392 (73.5) | 149 (64.2) | 243 (80.7) | .0001 |
| Age ≥75 y | 197 (37.0) | 64 (27.6) | 133 (44.2) | .0001 |
| CHADS2 | 1.6 ± 1.2 | 1.5 ± 1.1 | 1.8 ± 1.2 | .001 |
| CHA2DS2-VASc | 3.0 ± 1.6 | 2.2 ± 1.4 | 3.7 ± 1.4 | .0001 |
CHADS2, congestive heart failure, hypertension, age, diabetes, stroke (doubled); CHA2DS2-VASc, congestive heart failure, hypertension, age ≥ 75 (doubled), diabetes, stroke (doubled)-vascular disease and sex category (female); CHF, chronic heart failure; COPD, chronic obstructive pulmonary disease; OSA, obstructive sleep apnea.
Data are expressed as No. (%) or mean ± standard deviation.
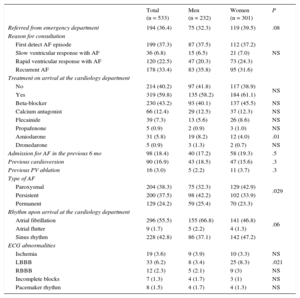
There were no differences between sexes in clinical characteristics upon arrival at the cardiology department, except for the type of AF prompting the visit: there was a higher rate of persistent AF in men and of paroxysmal AF in women (P = .029). Some type of AF rhythm control was administered to 80 patients (14.9%), with no differences between sexes, except that amiodarone was used more often in men than in women (8.2% vs 4.0%; P < .01); 296 (55.6%) patients had prescription drugs to slow the rate, mostly beta-blockers; 214 (40.2%) patients were prescribed no specific treatment for the arrhythmia (Table 2).
Population Characteristics Upon Arrival at the Cardiology Department
| Total (n = 533) | Men (n = 232) | Women (n = 301) | P | |
|---|---|---|---|---|
| Referred from emergency department | 194 (36.4) | 75 (32.3) | 119 (39.5) | .08 |
| Reason for consultation | NS | |||
| First detect AF episode | 199 (37.3) | 87 (37.5) | 112 (37.2) | |
| Slow ventricular response with AF | 36 (6.8) | 15 (6.5) | 21 (7.0) | |
| Rapid ventricular response with AF | 120 (22.5) | 47 (20.3) | 73 (24.3) | |
| Recurrent AF | 178 (33.4) | 83 (35.8) | 95 (31.6) | |
| Treatment on arrival at the cardiology department | ||||
| No | 214 (40.2) | 97 (41.8) | 117 (38.9) | NS |
| Yes | 319 (59.8) | 135 (58.2) | 184 (61.1) | |
| Beta-blocker | 230 (43.2) | 93 (40.1) | 137 (45.5) | NS |
| Calcium antagonist | 66 (12.4) | 29 (12.5) | 37 (12.3) | NS |
| Flecainide | 39 (7.3) | 13 (5.6) | 26 (8.6) | NS |
| Propafenone | 5 (0.9) | 2 (0.9) | 3 (1.0) | NS |
| Amiodarone | 31 (5.8) | 19 (8.2) | 12 (4.0) | .01 |
| Dronedarone | 5 (0.9) | 3 (1.3) | 2 (0.7) | NS |
| Admission for AF in the previous 6 mo | 98 (18.4) | 40 (17.2) | 58 (19.3) | .5 |
| Previous cardioversion | 90 (16.9) | 43 (18.5) | 47 (15.6) | .3 |
| Previous PV ablation | 16 (3.0) | 5 (2.2) | 11 (3.7) | .3 |
| Type of AF | .029 | |||
| Paroxysmal | 204 (38.3) | 75 (32.3) | 129 (42.9) | |
| Persistent | 200 (37.5) | 98 (42.2) | 102 (33.9) | |
| Permanent | 129 (24.2) | 59 (25.4) | 70 (23.3) | |
| Rhythm upon arrival at the cardiology department | .06 | |||
| Atrial fibrillation | 296 (55.5) | 155 (66.8) | 141 (46.8) | |
| Atrial flutter | 9 (1.7) | 5 (2.2) | 4 (1.3) | |
| Sinus rhythm | 228 (42.8) | 86 (37.1) | 142 (47.2) | |
| ECG abnormalities | ||||
| Ischemia | 19 (3.6) | 9 (3.9) | 10 (3.3) | NS |
| LBBB | 33 (6.2) | 8 (3.4) | 25 (8.3) | .021 |
| RBBB | 12 (2.3) | 5 (2.1) | 9 (3) | NS |
| Incomplete blocks | 7 (1.3) | 4 (1.7) | 3 (1) | NS |
| Pacemaker rhythm | 8 (1.5) | 4 (1.7) | 4 (1.3) | NS |
AF, atrial fibrillation; ECG, electrocardiogram; LBBB, left bundle branch block; NS, nonsignificant difference; PV, pulmonary vein; RBBB, right bundle branch block.
Values are expressed as n (%).
Of the 533 patients, 194 (36.4%) were referred from the emergency departments they had visited for AF, and 287 (53.8%) were referred from their primary care physician or other hospital departments, but all had been referred to a cardiologists for symptoms of AF, and 52 (9.7%) patients had been referred for problems associated with AF detected during a routine check-up. Of the 481 patients referred to a cardiologist for specific clinical problems arising from AF, the cardiologists considered that the referral was appropriate in 452 (93.7%). The CPGs recommend that patients with symptomatic AF or AF-related complications (class IIa/level C) should be referred to a cardiologist.
The most frequent clinical cause prompting the visit was similar in both sexes (Table 2). Of the 194 patients (36.4%) referred from emergency departments, 100 had attended for a first AF episode, 8 for AF with slow ventricular response, 25 for AF with rapid ventricular response, and 61 for recurrent AF. There were no differences between sexes. Of the 287 patients referred from primary care, 37 (12.9%) were referred due to poor INR control and arrhythmias.
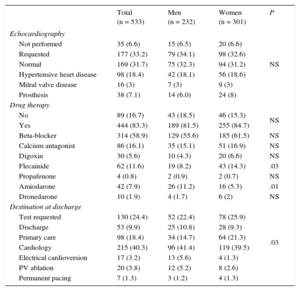
Echocardiography in Patients With Atrial FibrillationEchocardiography was performed in 321 patients (60.2%); this procedure was requested in 177 (33.2%) and was not performed or requested in 35 (6.6%) patients due to their having undergone echocardiography within the last 12 months. That is, echocardiography was performed in 93.4% of patients, as recommended by the CPGs (class IB in patients with severe symptoms, suspected or documented heart disease or risk factors, and class IIa/level C in patients with documented or suspected AF). No differences were found between sexes in the 321 echocardiography procedures performed in the cardiology department (Table 3).
Care Provided in the Cardiology Department
| Total (n = 533) | Men (n = 232) | Women (n = 301) | P | |
|---|---|---|---|---|
| Echocardiography | NS | |||
| Not performed | 35 (6.6) | 15 (6.5) | 20 (6.6) | |
| Requested | 177 (33.2) | 79 (34.1) | 98 (32.6) | |
| Normal | 169 (31.7) | 75 (32.3) | 94 (31.2) | |
| Hypertensive heart disease | 98 (18.4) | 42 (18.1) | 56 (18.6) | |
| Mitral valve disease | 16 (3) | 7 (3) | 9 (3) | |
| Prosthesis | 38 (7.1) | 14 (6.0) | 24 (8) | |
| Drug therapy | ||||
| No | 89 (16.7) | 43 (18.5) | 46 (15.3) | NS |
| Yes | 444 (83.3) | 189 (81.5) | 255 (84.7) | |
| Beta-blocker | 314 (58.9) | 129 (55.6) | 185 (61.5) | NS |
| Calcium antagonist | 86 (16.1) | 35 (15.1) | 51 (16.9) | NS |
| Digoxin | 30 (5.6) | 10 (4.3) | 20 (6.6) | NS |
| Flecainide | 62 (11.6) | 19 (8.2) | 43 (14.3) | .03 |
| Propafenone | 4 (0.8) | 2 (0.9) | 2 (0.7) | NS |
| Amiodarone | 42 (7.9) | 26 (11.2) | 16 (5.3) | .01 |
| Dronedarone | 10 (1.9) | 4 (1.7) | 6 (2) | NS |
| Destination at discharge | .03 | |||
| Test requested | 130 (24.4) | 52 (22.4) | 78 (25.9) | |
| Discharge | 53 (9.9) | 25 (10.8) | 28 (9.3) | |
| Primary care | 98 (18.4) | 34 (14.7) | 64 (21.3) | |
| Cardiology | 215 (40.3) | 96 (41.4) | 119 (39.5) | |
| Electrical cardioversion | 17 (3.2) | 13 (5.6) | 4 (1.3) | |
| PV ablation | 20 (3.8) | 12 (5.2) | 8 (2.6) | |
| Permanent pacing | 7 (1.3) | 3 (1.2) | 4 (1.3) |
NS, nonsignificant; PV, pulmonary vein.
Values are expressed as n (%).
After assessment in the cardiology department, specific treatment for AF was deemed unnecessary in 89 patients (16.7%), most of whom were patients with a first AF episode that had already resolved or patients whose medication had been withdrawn because of a slow heart rate. Specific treatment was prescribed in 444 patients (83.3%). The number of patients using antiarrhythmic drugs increased from 80 to 118; the most-used drug was flecainide followed by amiodarone. Similarly, the 296 patients who were already receiving rate-slowing drugs increased to 430; beta-blockers were the drugs most often used and digoxin was prescribed in 30 patients. These drugs are recommend in the CPGs (class I/level B).
Once the patients had been seen in the cardiology department, the most frequent recommendations were for a new appointment in the cardiology department (with or without new diagnostic tests) for AF control in 215 (40.3%) patients, a new test and appointment after receiving the test results in 130 (24.4%), pulmonary vein ablation in 20 (3.8%), electrical cardioversion (ECV) in 17 (3.2%), permanent pacing in 7 (1.3%), follow-up in primary care in 98 (18.4%), and discharge in 53 (9.9%) (Table 3). The CPGs recommend that elective ECV be considered to start a long-term rhythm control strategy in patients with AF (class IIa/level B).
Embolism Prevention and Reasons For Not Using ItOral anticoagulants had been used prior to the episode prompting the visit by 273 patients (51.2%), and had been prescribed in 79 (14.8%) because of this episode. Thus, when they visited the cardiology department, 352 patients (66%) were receiving anticoagulant therapy; 304 (57%) with VKAs and 48 (9%) with DAs. In the previous 3 months, TTR, as measured with the Rosendaal index, was 48.4 ± 37.4 in patients on anticoagulation therapy with VKAs.
The number of patients prescribed anticoagulant therapy increased to 425 (79.8%).
Of these, 339 were prescribed VKAs: 90 (16.9%) received warfarin, and 249 (46.7%) received acenocoumarol, 20 of whom also received acetylsalicylic acid.
The remaining 84 patients (15.8%) were prescribed ADs: 50 (9.4%) received dabigatran, 26 (4.9%) received rivaroxaban, 8 (1.5%) received apixaban, 5 of whom also received aspirin. Finally, left atrial appendage closure was recommended in 2 patients. We analyzed prescription of anticoagulation therapy in patients with nonvalvular AF (n = 479), excluding 16 patients with mitral valve disease and 38 with prosthetic heart valves. There was a linear increase in prescription of anticoagulant therapy with VKAs and DAs according to the risk of embolism (Figure).
Percentage of patients with nonvalvular atrial fibrillation (n = 479) receiving anticoagulation therapy with vitamin K antagonists or direct anticoagulants according to the CHADS2 (congestive heart failure, hypertension, age, diabetes, stroke [doubled]) and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥ 75 [doubled], diabetes, stroke [doubled]-vascular disease and sex category [female]) scores.
Of the 108 patients (20.2%) not receiving anticoagulation therapy, 72 received aspirin, whereas only 36 patients received no treatment for embolism prevention. The use of aspirin for embolism prevention is a CPG class I/level B recommendation only for patients with CHADS2 = 0 and CHA2DS2-VASc = 0 and patients with CHA2DS2-VASc = 1. The reasons given by cardiologists for not prescribing anticoagulant drugs to these 108 patients were the low risk of embolism in 49 (9.1%), a first AF episode in 24 (4.5%), the patient's preference in 16 (3.0%), a history of bleeding in 11 (2.1%), a high risk of falls in 5 (0.9%), and the physician's preference in 3 (0.6%). The CPGs recommend (class I/level A) antithrombotic therapy to prevent thromboembolism in all patients with AF, except those at low risk (isolated AF, age less than 65 years, or contraindications).
DISCUSSIONSeveral findings of this registry were striking. Regarding clinical characteristics, there was a high percentage of young patients with AF, and significant clinical differences were found between sexes. The following aspects should be emphasized: the poor control of anticoagulation with VKA drugs in the study population; the low use of DAs in anticoagulant therapy prescribed by cardiologists; and, regarding the care indicators, the high adherence to the recommendations of the CPG in the management of AF patients. If patients attending cardiology departments for follow-up of AF had been included in the study, the results would have been applicable to the whole population of patients with nonvalvular AF treated in cardiology departments. However, the characteristics of these patients were analyzed in 2010 and the cardiologists did not modify treatment and consequently we decided to center the analysis on patients with clinical problems associated with AF.
As observed in 2010, although the mean age of the population was 70 years, a significant proportion of patients were very young; in 2010, 20.7% were younger than 65 years, in 2014 the figure increased to 24.3%, but currently 3% are younger than 40 years.6 Regarding sex, the prevalence of AF in the 2010 study was similar to that in 2014 (49.5% and 50.5%) and was also the same in men (4.4% [3.6% to 5.2%]) and women (4.5% [3.6% to 5.3%]) in population studies.1,6 However, the present study found significant sex differences, which were similar to those in the entire population with AF assessed in 2010. Thus, more women seek medical attention for AF than men (56.5% vs 43.5%). This finding is also in line with observations in Spanish emergency departments. In our registry, women were older and, except for patients with a history of ischemic heart disease, other heart diseases were more prevalent in women than in men. This finding is one of the reasons why the CHADS2 and CHA2DS2-VASc scores were clearly worse in women than in men. Future studies should assess if there is a relationship between sex and the occurrence of clinical problems in patients with AF, because this question cannot be answered by the findings of this registry. No explanation could be found for sex differences in the type of AF (P = .029) or in the literature addressing this issue.
Strikingly, an enormous number of patients were referred for a diagnosis of AF but received no treatment: only 59.8% of these patients were treated to control the rhythm or rate and only 66% were given anticoagulant therapy. Thus, increased efforts must be made when patients are diagnosed with AF, especially in the prescription of anticoagulants. After patient assessment in the cardiology department, sex differences were found in referral from cardiology to primary care (14.7% men and 21.0% women), with no observable reason for this finding.
Source of Patients and Appropriateness of ReferralsMore than 53% of patients with clinical problems were referred from primary care or other hospital departments, and more than a third were referred from the emergency department. Once the referral was assessed according to predefined criteria, 94% of patients were considered to have been appropriately referred in the opinion of the treating cardiologist. Thus, this care indicator performed beyond expectations and does not need improvement.
EchocardiographyEchocardiography is recommended in the CPGs. More than 94% of patients underwent the technique and only 35 (6.5%) patients were not considered to require an echocardiogram after assessment. Notably, 321 of these patients underwent the technique in the same consultation, which demonstrates the high percentage of patients attended using a strategy known as one-stop consultations. Therefore, there was full compliance with this care indicator.
Treatment Received in the Cardiology DepartmentAs recommended by CPGs, beta-blockers are the drugs most commonly used to slow heart rate.2 However, ECV was recommended in only 17 (3.2%) of the study patients and pulmonary vein ablation in only 20 (3.8%); more patients should undergo these procedures, as recommended by the CPGs. Importantly, many of the patients were already receiving anticoagulants and could have been recommended to undergo ECV (class I if there are symptoms or hemodynamic instability, and class IIa to begin a long-term rhythm control strategy2). There was no apparent reason for sex differences in indications for ECV. The low use of ECV should be put in context, among which could be poorly controlled anticoagulation therapy, but it is difficult to find a single explanation. Similar findings8,9 have been described in Spanish emergency department registries, in which the proportion of patients with AF who underwent ECV was only 6%, and in European registries, in which the proportion was only slightly higher (9.7%). This proportion is also similar to that described in clinical trials of DAs. The RE-LY trial reported that 9.14% of patients had received DAs,10 the ROCKET trial reported 1%,11 and the ARISTOTLE trial reported 4%.12 Furthermore, recent studies have shown that the use of DAs in patients undergoing ECV is safe and effective, which should certainly encourage their use and contribute to an increase in indications for ECV in the future.13,14
Although it may appear that there was little use of pulmonary vein ablation, no explanation can be offered for the difference found between sexes. In the present study, the use of this procedure was comparable to that of European registries (4.4%) and Spanish registries, which reported 2201 pulmonary vein ablation procedures in 2013. Currently, few suitable patients undergo this technique, and there is much room for improvement in these figures.9,15 Clearly, the fact that 24.3% of our patients were younger than 65 years should serve to increase indications for this technique in the future.
Embolism Prevention and Reasons For Not Using ItThis section presents 4 relevant findings. Firstly, among the 339 patients with a recommendation for VKA use, acenocoumarol was used much more frequently than warfarin: 249 (46.7%) vs 90 (16.9%) patients. To our knowledge, there is no reason for not using warfarin; furthermore, no clinical trial has demonstrated the efficacy of acenocoumarol in these patients. However, acenocoumarol is widely used throughout Spain.
Secondly, the TTR of 48.4% ± 37% in the 3 previous months is not a good indicator. Given that anticoagulation therapy is not monitored in cardiology departments, it is a care indicator that cannot be optimized in that setting; however, its use should be optimized in those departments where it is administered. However, our TTR data are similar to those of an American study reporting a TTR of 53.7% in a population of 138 319 patients. However, this figure is far lower than the 63.8% reported in the CALIFA study, which included 1056 Spanish patients, or the mean TTR of 66% in Spanish patients included in the RE-LY trial.16–18 Action should be taken in collaboration with primary care and hematology services to increase the TTR in order to optimize anticoagulation therapy. Similarly, if it becomes clear that the TTR cannot be optimized, VKAs should be replaced by DAs.
Thirdly, in 2014 the approach of cardiologists in the same departments was compared with that in 2010. We found that the percentage of patients receiving anticoagulation therapy had increased (from 60.0% to 79.8%); a justification was found for the 20.2% of the patients not recommended this treatment.6 This improvement may have been influenced by the CPGs and by the important clinical information obtained in clinical trials published in this field, which has increasingly convinced cardiologists of the need to use embolism prevention strategies in patients with AF. Regarding the levels of risk on the CHADS2 and CHA2DS2-VASc scales, the use of VKAs and DAs significantly increased in relation to the increased risk of embolism, which differed from that observed in 2010. The analysis of anticoagulation therapy in patients with nonvalvular AF showed that, as in 2010, 60% of patients with CHADS2 score = 0 and CHA2DS2-VASc score = 0-1 received anticoagulation therapy, which is not indicated in such patients according to the CPGs. A possible explanation for this approach is that most of these patients had been recently diagnosed and would be treated for electrical or pharmacological cardioversion; however, since only 14.9% received an antiarrhythmic agent and only 3.4% were referred for ECV, and thus this explanation is incorrect. The Val-FAAP study found that 48.9% of patients with a CHADS2 score= 0 received anticoagulation therapy.19 The reasons for not prescribing anticoagulation therapy to 20.2% of the patients with AF were similar to those described in other studies. The AFABE study showed that 24% of patients did not receive anticoagulation therapy. The most common reasons reported were the lack of indications based on the CHADS2 score (5.1%), cognitive impairment (3.6%), and the risk of bleeding (2.9%).20 The present study observed a significant reduction in the use of aspirin (18.1%) compared with its use in 2010 (37.1%). In another study, aspirin was prescribed in 25 of the 425 patients who had indications for oral anticoagulation therapy and in 72 of the 108 patients without an indication.6 The Val-FAAP study, which was also conducted in 2010, showed that at that time aspirin use ranged from 31.9% of AF patients with a CHADS2 score = 0 to 19.3% of AF patients with a CHADS2 score ≥ 2.19
Finally, only 15.7% of patients receiving anticoagulation therapy received DAs due to poor INR control. This aspect is clearly novel, because these drugs were not used in 2010. Poor INR control was the underlying reason for the increased use of DAs from 9% to 15.7% in patients attending the cardiology department. However, this increase is very low and is far from optimal. Administrative issues and therapeutic inertia were the 2 main reasons given by cardiologists to explain this problem, despite a high percentage of patients with poor INR control (TTR, 48.4% ± 37%). The enormous administrative problems can be broken down into 2 issues: firstly, the inability of the cardiologists to access patient data on INR control, although this information was available in this study and therefore cannot be used to explain the nonprescription of DAs. Secondly, physicians in Spain cannot follow the recommendations of the CPGs that highlight the superiority of DAs over VKAs, but can only follow the criteria recommended by the Spanish Agency for Medicines and Health Products, which prohibits the use of these drugs in patients with de novo AF and limits their use almost exclusively to patients with poor INR control.
Attention should be drawn to therapeutic inertia because, given the observed TTR, there has been a marked improvement in adherence by cardiologists to the recommendations of the CPGs. It is very likely that the strategy of using DAs will strongly increase in the future.
LimitationsThe study was affected by selection bias because the patients were referred from other departments in our hospitals. The diagnostic criteria are also another possible source of bias, given that they may have led to patient exclusion due to diagnostic errors. The data collected from each patient may have suffered bias, which may have led to errors in their interpretation. The study could have been optimized by the inclusion of the symptoms reported by the patients. It would have been useful to have compared the results obtained in 2014 with those before the publication of the CPGs, using a statistical design with the same population as in 2010. However, this was not done and different populations were studied, thus preventing such an analysis. The HAS-BLED (hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly [> 65 years], drugs/alcohol concomitantly) scale was not used to analyze the risk of bleeding, which would have completed the assessment of the patients with AF. Poor practice was shown by the finding that nearly 60% of patients with no indication for anticoagulation therapy received this treatment; this is an outstanding issue that needs to be addressed and resolved.
CONCLUSIONSOne in 4 patients seeking medical attention for AF are young, the prevalence of clinical problems is higher in women, and more women with AF than men with AF seek medical care. More than 70% of the problems are de novo AF or recurrent AF. More than 94% of patients are appropriately referred to the cardiology department, and more than 53% of patients are referred by their primary care physician or by other hospital departments. Although the number of ECVs and pulmonary vein ablation procedures should be increased, echocardiography and antiarrhythmic and anticoagulant therapy continue to be used as recommended by the CPGs. There is underuse of VKAs as anticoagulation therapy.
FUNDINGThis study was funded by the Research Agency of the Spanish Society of Cardiology.
CONFLICTS OF INTERESTNone declared.


![Percentage of patients with nonvalvular atrial fibrillation (n = 479) receiving anticoagulation therapy with vitamin K antagonists or direct anticoagulants according to the CHADS2 (congestive heart failure, hypertension, age, diabetes, stroke [doubled]) and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥ 75 [doubled], diabetes, stroke [doubled]-vascular disease and sex category [female]) scores. Percentage of patients with nonvalvular atrial fibrillation (n = 479) receiving anticoagulation therapy with vitamin K antagonists or direct anticoagulants according to the CHADS2 (congestive heart failure, hypertension, age, diabetes, stroke [doubled]) and CHA2DS2-VASc (congestive heart failure, hypertension, age ≥ 75 [doubled], diabetes, stroke [doubled]-vascular disease and sex category [female]) scores.](https://static.elsevier.es/multimedia/18855857/0000006900000004/v1_201604051616/S1885585715003928/v1_201604051616/en/main.assets/thumbnail/gr1.jpeg?xkr=eyJpdiI6IlcxL3BYWDVsMXk4K2FlMjNEMkhKMmc9PSIsInZhbHVlIjoiZ0U5MFR4eW01Vi80MktVTERWMGJiUTBTYy9BT0JSUWVSaTZBb0dyb0ZKND0iLCJtYWMiOiIzMzU1OTUxYWQyYmI5Yjc4MzQwM2YzM2NmNjRmZjU2NzRkZjliNTdhYTc1NTYxNDZjODg4MTNlZjEwZGVkZmUwIiwidGFnIjoiIn0=)