Disability refers to a decrease in functional status related to activities of daily living. The Barthel index is used to measure disability and has proved to be useful in assessing functional status in elderly patients after stroke.1 The relationship between disability and prognosis after acute coronary syndromes, however, has been little investigated to date.
The boundaries between frailty and disability are unclear: although both conditions can overlap, some authors argue that frailty should be considered a predisability state.2 Following this line of thought, we speculated that there is a continuum of progressive vulnerability from frailty to disability and that an index integrating frailty and disability would improve risk stratification after acute coronary syndrome. This hypothesis was tested in the present study.
The study group consisted of 342 hospitalized patients who had survived acute coronary syndrome. Before discharge they underwent a full geriatric assessment, which included frailty, disability (Barthel index) and comorbidities (Charlson index). Likewise, a large number of variables were included from clinical assessment, electrocardiograms, blood tests, and echocardiograms. Further details of the study are provided elsewhere.3,4 The primary endpoint was all-cause mortality at a median follow-up of 4.7 years.
By Cox regression analysis (backward method), the clinical predictive model included the following independent variables: age, Killip class ≥ 2, left ventricular ejection fraction, hemoglobin and Charlson index. All predictive analyses involving frailty and disability were adjusted for this clinical model. Frailty was evaluated with the Fried and Green scores, the latter being used for statistical adjustment since it was the strongest predictor in a previous study.3,4 The Barthel index was analyzed as a continuous and dichotomized variable, dividing the patient cohort into nondisabled (Barthel index > 90; n = 279) and disabled (Barthel index ≤ 90; n = 63) subgroups according to the predefined moderate disability cutoff.1
Of 342 patients hospitalized for acute coronary syndrome (mean age 77.5 ± 7.1 years, 21% ST-segment elevation acute myocardial infarction), a total of 156 patients died after discharge. The median Barthel index was 100 points [98.75-100]. Sixty-three (18%) patients showed at least moderate disability (Barthel index ≤ 90). The Barthel index was not significantly associated with mortality (per point, P = .13; Barthel ≤ 90 points; P = .09), after adjustment for the clinical model and the Green score. Frailty, however, was predictive: per point of the Green score, hazard ratio, 1.19; 95% confidence interval, 1.06-1.21; P = .0001; Green score ≥ 5 points, hazard ratio, 1.91; 95% confidence interval, 1.28-2.89; P = .002). The 5-point cutoff was chosen according to a previous study.3
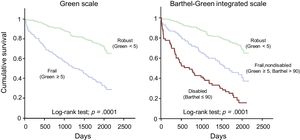
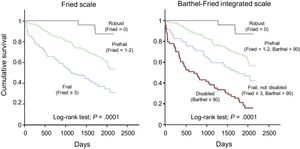
All disabled patients were also frail, while 100 out of 279 (36%) nondisabled patients were frail. Accordingly, we built a new scale integrating disability and frailty: disabled (Barthel ≤ 90, n = 63), frail nondisabled (Green ≥ 5, Barthel > 90, n = 100) and robust (Green < 5, Barthel > 90, n = 179). The mortality rate progressively decreased from disabled, to frail nondisabled, and robust categories: 81%, 56% and 27% (log-rank test; P = .0001, Figure 1). Likewise, mortality risk progressively decreased after adjustment for the clinical model (compared with the disabled subgroup; frail nondisabled: hazard ratio, 0.70; 95% confidence interval, 0.47-1.05; P = .08; robust: hazard ratio, 0.41; 95% confidence interval, 0.25-0.66; P = .0001). The integrated frailty/disability scale also performed well using the predefined categories of robust, prefrail and frail, in the Fried scale (Figure 2).5
This study proposes a simple geriatric scale, integrating frailty and disability, which has proven to be of prognostic value after acute coronary syndrome. The scale attempts to optimize patient classification according to age-related vulnerability.
There is little information about the Barthel index as a prognostic factor in acute coronary syndromes. In our population, only 18% of the patients had at least moderate disability (Barthel index ≤ 90 points). This might reflect the selection bias of patients admitted to a cardiology ward. The small number of disabled patients would explain the lack of predictive value of the Barthel index. However, the incorporation of the disabled subgroup into the frail classification provided a more comprehensive risk gradient. Disabled patients had the highest mortality risk, followed by frail and robust patients. Therefore, the main contribution of the integrated scale, unlike the simple frailty scale, is the distinction between high (disabled) and intermediate (frail but nondisabled) risk subgroups. Additionally, categorization of the nondisabled patients into frail and nonfrail subgroups was also useful for risk stratification. Our study confirms that disability and frailty can be considered in aggregate and result in a gradation in long-term outcomes after acute coronary syndrome. Conceivably, frailty scales other than Green's and Fried's, using alternative definitions of frailty, might also fit this mixed frailty/disability scale.
A major concern is to decide on the best management of these patients. Potentially, geriatric assessment might lead to a more personalized approach to the elderly patient with acute coronary syndrome. Further trials targeting elderly patients with geriatric conditions and acute coronary syndrome are warranted.6
FundingThis work was supported by grants from Spain's Ministry of Economy and Competitiveness through the Carlos III Health Institute: CIBER-CV 16/11/00420 and FIS 15/00837; FEDER; Health Research Fund, Madrid, Spain.
.