We have read the article published by Redondo-Diéguez et al1 with interest. Our reading of this article has prompted us to offer a few comments.
In 2010, we published the results of the GYSCA Registry,2 analyzing the relevance of hospital type (tertiary care or secondary care) in the approach to Non–ST-segment elevation acute coronary syndrome (NSTEACS) and its prognosis. Data from this registry, including those referring to patients with no significant lesions (SL), have been presented at scientific meetings.
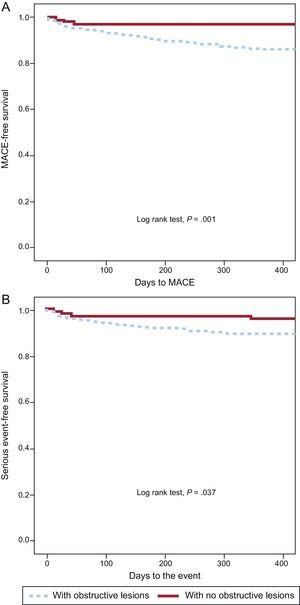
The GYSCA study was a prospective registry of 1133 consecutive patients admitted to 15 Spanish hospitals for NSTEACS. The prevalence of coronary angiographies without SL was 14.8%. At discharge, these patients received fewer treatments for secondary prevention. The incidence of major cardiac events was lower (2.5% vs 14%; P<.001) (Figure 1A). There were no cardiac-related deaths in this group of patients. With respect to the events evaluated in the study by Redondo-Diéguez et al1 (death or readmission due to acute coronary syndrome), the incidence in the GYSCA registry was 4.1% vs 11.2% (P=.042) (Figure 1B). This follow-up (1 year) was shorter than that in the study by Redondo-Diéguez et al1 (4.8 years), although, importantly, GYSCA was a prospective study with minimal losses to follow-up.
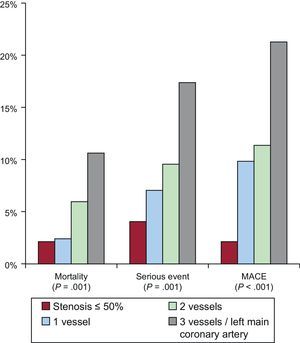
We also analyzed prognostic differences according to the extent of coronary artery disease. The mortality rate was very similar in patients with no SL and in those with single-vessel disease (Figure 2).
We consider that the prognosis of patients with no SL should focus on coronary events and cardiac death, since overall mortality does not faithfully reflect the contribution of coronary artery disease to prognosis. Our study showed a better outcome in this population, a finding that coincides with that of Cortell et al,3 who observed that rates of death and myocardial infarction at 3 years were lower among patients with non-ST-segment elevation myocardial infarction without SL (6% vs 27%; P=.0001). Other studies have also demonstrated a favorable prognosis in the absence of SL, but there is a lack of agreement on the benign nature of the condition, as most authors report a small percentage of recurrent events, especially if there are irregularities in the coronary angiogram.
The frequency of NSTEACS without SL ranges from 8.6% to 14%. These differences may depend on the characteristics of the study populations (NSTEACS with or without biomarker elevation) and on the definition of insignificant lesions (normal coronary arteries or stenosis ≤ 50%).
Moreover, the pathophysiological mechanism of the ischemic event does not always involve rupture of an atheromatous plaque. The difficulty lies in correct determination of the cause, which will enable treatment optimization. The prognosis of those patients with arteriosclerotic disease who undergo spontaneous reperfusion is probably similar to that of individuals with “culprit” lesions. The absence of obstruction could be mistaken for the absence of disease and result in fewer measures being taken for secondary prevention, thus exposing the patient to a higher risk of event occurrence. In fact, in the study by Redondo-Diéguez et al1 and the GYSCA2 registry, the administration of treatments with a class I indication for secondary prevention was less widespread among individuals with no SL.
In view of the above, it is essential to establish a correct etiological diagnosis. This can be based on techniques such as intravascular ultrasound, optical coherence tomography, or coronary computed tomography angiography, which aid in the identification of arteriosclerosis, or magnetic resonance, which reveals areas of subendocardial fibrosis corresponding to necrosis.
With the application of these techniques, acute coronary syndrome without SL should now be less of an enigma. However, their use is limited by their lack of universal availability, their cost, and the added workload. Consequently, many Spanish patients are discharged from hospital without an accurate diagnosis and-even worse-without proper treatment to minimize the risk of new ischemic events.