Normal fetal heart rate ranges between 100 and 180 beats per minute. Fetal arrhythmias occur in 1% to 2% of pregnancies. The most common fetal arrhythmias are atrial extrasystoles, followed by supraventricular tachycardias (SVT), which are classified as sustained (present for more than 50% of the echocardiographic examination) or intermittent nonsustained (less than 50% of the examination). Sustained SVT is a major cause of nonimmune fetal hydrops, prematurity, and perinatal morbimortality. Treatment depends on gestational age, duration of the SVT, the degree of fetal involvement, maternal health status, and the possible risks of treatment for the mother and fetus. The goal of treatment is to restore sinus rhythm (SR) or to reduce the heart rate for long enough to resolve or prevent ventricular dysfunction.
Between July 2003 and November 2014, 6100 pregnant women at our center were referred for fetal echocardiography. Examinations were performed using the combined M-mode and pulsed Doppler approach.1 Arrhythmias were detected in 2.7% of pregnancies (165 fetuses). The women gave informed consent, and electrocardiograms and blood drug concentrations were obtained from all study participants. Electrocardiograms and echocardiograms were obtained from all newborns.
The following arrhythmias were detected:
- •
Atrial extrasystoles in 137 (83%) of fetuses, with no development of other arrhythmias.
- •
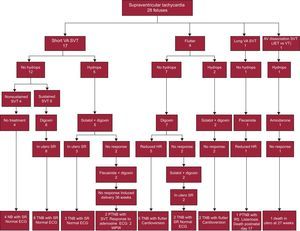
Supraventricular tachycardia in 28 (17%) of fetuses (Figure 1):
- -
Tachycardia with a short ventriculoatrial (VA) interval was detected in 17 fetuses: a) 4 had nonsustained tachycardia without hydrops and received no treatment; b) sustained tachycardia without hydrops was detected in 8 fetuses, and maternal oral digoxin therapy restored SR in all cases, and c) the remaining 5 fetuses had tachycardia with hydrops. Tachycardia was successfully reverted in 3 of these fetuses by combined maternal therapy with digoxin and sotalol. In the 2 fetuses that failed to respond, sotalol was replaced with flecainide. After continued failure to respond, a decision was made to induce delivery at 36 weeks gestation. Postnatal diagnosis confirmed Wolff–Parkinson–White syndrome, which was treated with adenosine (Figure 1).
- -
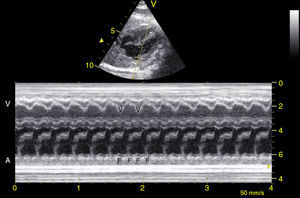
Atrial flutter was detected in 9 fetuses (Figure 2): a) 7 did not have hydrops, and maternal digoxin therapy reduced heart rate sufficiently to allow delivery at term in 5 of them; b) the other 2 fetuses failed to respond to digoxin alone, and sotalol therapy was added, restoring SR in both fetuses. The 2 fetuses with hydrops did not respond to combined maternal therapy with digoxin and sotalol, and delivery was induced at 36 weeks gestation. The 7 newborns with atrial flutter underwent electric cardioversion.
- -
One fetus had long VA interval tachycardia (190 beats per minute) with no hydrops. Maternal flecainide therapy was given and the neonate was born with sinus tachycardia and congenital listeriosis.
- -
Tachycardia with atrioventricular dissociation was detected in 1 fetus at 25 weeks gestation with hydrops and ventricular dysfunction. The suspected diagnosis was junctional ectopic tachycardia or ventricular tachycardia. Amiodarone therapy was given, but the fetus died in utero.
Figure 1.Type, treatment, and outcome of fetal tachycardias. AV, atrioventricular; ECG, electrocardiogram; HR, heart rate; JET, junctional ectopic tachycardia; NB, newborn; PTNB, preterm newborn; SR, sinus rhythm; SVT, supraventricular tachycardia; TNB, term newborn; VA, ventriculoatrial; VT, ventricular tachycardia; WPW, Wolff–Parkinson–White syndrome.
(0.39MB). - -
The incidence of irregular fetal heart rhythm is unknown. M-mode and pulsed Doppler echocardiography is the method of choice for determining the atrioventricular relation in the fetus and inferring the electrophysiological mechanism.2
The most common heart rhythm irregularities are premature atrial contractions, which are benign and which are often related to maternal stimuli, do not require treatment, and resolve spontaneously. Between 1% and 3% of cases progress to SVT, but this did not occur in any of the fetuses in our series. Sustained tachycardias, generally > 220 beats per minute, can lead to fetal hydrops, with mortality above 50%. There are no randomized studies on which drug to use, and current procedures are therefore based on descriptive series.3
In most centers, the treatment of choice for fetal arrhythmia is digoxin monotherapy, except in cases of fetal hydrops, in which the placental edema requires combination with another drug. The most commonly used are flecainide, sotalol, and amiodarone, but there is no evidence to direct the choice of one over another. In our study, we followed a uniform protocol of combined digoxin and sotalol, which has a reported complete or partial response rate of 85%.4
For sustained fetal tachycardia without fetal hydrops, pregnant women were given oral digoxin at 1mg/d for the first 48hours, followed by 0.25mg/d (dose concentrations of 0.7-2 ng/mL). If digoxin monotherapy did not induce a response by day 7, solatol therapy was added at 80mg every 12hours for 3 days and was increased to 160mg every 12hours if there was still no response. In cases with hydrops, combined digoxin and solatol therapy was given from treatment outset. In 2 patients, sotalol had to be substituted with flecainide, but there was no response. Sinus rhythm was achieved in 85% (11 of 13) of the fetuses in our series that received treatment for short VA tachycardia. A similar treatment was used for atrial flutter; the goal was to achieve partial atrioventricular node block, prevent 1:1 conduction, or ensure conversion to SR, and was achieved in 77% of fetuses (7 of 9). The efficacy of sotalol in these cases supports its use as a first-line treatment for this condition.5 Our treatment regimen restored SR or controlled heart rate in 85% (23 of 27) of fetuses with confirmed SVT.
In the single case of long VA tachycardia, heart rate was reduced with flecainide therapy. Postnatal examination revealed sinus tachycardia. These tachycardias are difficult to distinguish in utero, except for the frequency variability in sinus tachycardia. Ventricular tachycardia is very rare, and is treated with propanalol or amiodarone; in the single possible case in our series, amiodarone therapy was used, without success.
In conclusion, the most common fetal arrhythmia is atrial extrasystole, which is benign and does not require treatment. The most frequent tachyarrhythmias are short VA tachycardia and atrial flutter, which can usually be controlled with appropriate treatment.