A 75-year-old male smoker with diabetes and dyslipidemia was admitted to our hospital in January 2011 with anterior acute myocardial infarction. Emergency coronary angiography revealed severe atheromatous disease with thrombosis in the proximal and medial segment of the left anterior descending artery. The lesion was revascularized in a percutaneous procedure by balloon angioplasty and placement of 2 overlapping everolimus-eluting stents (Promus Element 2.75×24mm and 3.5×24mm, Boston Scientific Corporation; Natick, Massachusetts, United States) (Fig. 1). In addition, a severe lesion was detected by angiography in the medial segment of the right coronary artery and treated in a scheduled procedure 1 month later. In view of the characteristics (short nonostial de novo lesion in a native coronary artery with a good caliber and without significant calcification) and the satisfactory dilation achieved with balloon angioplasty, the patient was implanted with a bioresorbable everolimus-eluting vascular scaffold (Absorb BVS 3.0×18mm, Abbott Vascular; Santa Clara, California, United States) (Fig. 2).
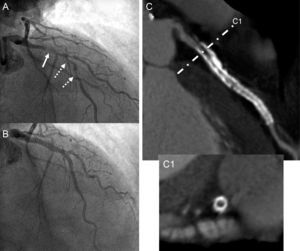
A: Intraluminal thrombus leading to deficient perfusion in the proximal segment of the left anterior descending artery (solid arrow) and severe atheromatous disease in the medial segment of the same artery (dashed arrows). B: Angiographic outcome at the site of primary angioplasty with placement of 2 overlapping drug-eluting metal stents. C: Noninvasive angiographic study by computed tomography at 2 years; a substantial metal artifact is observed (high white density) resulting from both stents. C1: Transversal section of the proximal segment of the left anterior descending artery showing significant intrastent neointimal hyperplasia in the study (low black density tissue).
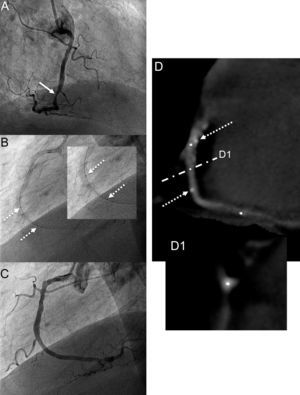
A: Severe atheromatous lesion of the medial segment of the right coronary artery (arrow). B: Placement of bioresorbable vascular scaffold; the 2 radiopaque markers at either end of the stent can be seen (dashed arrows). C: Angiographic outcome after placement of the bioresorbable vascular scaffold. D: Noninvasive angiographic assessment by computed tomography at 2 years, in which only the radiopaque markers can be seen (dashed arrows) in the medial segment of the right coronary artery. D1: Transversal segment of the artery at the same site, confirming the absence of intraluminal stent and tissue indicative of neointimal hyperplasia.
In March 2013, multislice coronary computed tomography was performed (Aquilion 64, Toshiba Corporation; Tokyo, Japan), showing the outcome of both percutaneous coronary interventions. In the case of the anterior descending artery, neointimal hyperplasia could be observed in the proximal stent and in the region of overlap, despite the metallic nature of the stents (Fig. 1). As expected, no metal artifact or neointimal hyperplasia was observed within the revascularized lesion with bioresorbable vascular scaffold, although the 2 platinum markers of the proximal and distal edges were evident (Fig. 2).
The advent of metal stents was a major advance in percutaneous coronary intervention procedures, as these significantly reduced acute occlusion and elastic retraction of the target lesions after simple balloon angioplasty. However, it was soon noted that the rate of restenosis, although lower, was still high, with neointimal hyperplasia developing to an even greater extent than after simple balloon angioplasty. Although drug-eluting stents have further improved the outcome of percutaneous coronary intervention, clinically relevant complications such as restenosis and late stent thrombosis are still observed.1 On the other hand, the presence of a metal structure inside the arterial lumen can induce a substantial inflammatory reaction that may lead to neoatherosclerosis and be at least a partial cause of severe long-term endothelial dysfunction in the target artery.2,3 In addition, the metal scaffolding limits subsequent enlargement of the artery and expansive remodeling.1
In view of the above, a novel and enticing concept is that bioresorbable vascular scaffolds may be able to provide the necessary support during the first few weeks to prevent acute occlusion and elastic retraction of the coronary artery while eluting an antiproliferative drug that reduces the risk of neointimal hyperplasia.
We believe that our case illustrates some of the advantages of these bioresorbable vascular scaffolds compared to metallic stents. The complete absence after 2 years of any endovascular structure (Fig. 2D) would minimize and even eliminate late events such as restenosis (Fig. 1C) or stent thrombosis. This in turn would make prolonged antiplatelet therapy unnecessary. Likewise, the absence of the scaffold would allow further interventions, both percutaneous and surgical, on the revascularized artery or secondary branches (note, for example, the caging of the diagonal branch in Fig. 1B compared to the transient caging of the acute marginal branch, Fig. 2C). Finally, metal stents are known to be responsible for a “blooming effect” in the images produced by coronary angiography or computed tomography that reveals a false thickening of the stent struts, leading to underestimation of the real diameter of the intrastent lumen. In the absence of any metal, noninvasive monitoring of the outcome by angiographic computed tomography or magnetic resonance imaging of arterial segments treated with bioresorbable vascular scaffolds could also be a valid and reliable alternative to invasive coronary angiography.