The efficacy of implantable cardioverter-defibrillators in preventing sudden death has been amply demonstrated.1 However, inappropriate discharge (ID) remains a therapeutic complication with negative consequences for prognosis and quality of life. Undoubtedly, IDs use up health care resources but no studies have attempted to quantify this cost. We present an analysis of the economic cost of ID-related medical attention in our center.
Between 2003 and 2011, we implanted cardioverter-defibrillators in 227 patients. Antitachycardia pacing therapy was programmed with 2 or 3 zones and overdrive pacing therapy. In the follow-up, the electrophysiologist analyzed each arrhythmic event. ID were defined as those applied in situations other than ventricular tachycardia or ventricular fibrillation, as well as in ventricular tachycardia/ventricular fibrillation appearing after inappropriate pacing in supraventricular or sinus tachycardia. Dubious cases were resolved by consensus. Prolonged episodes, which the device considers as more than one, were considered a single clinical episode.
Analysis was based on clinical episodes. We considered costs directly related with the medical attention received for each episode (extra visits to the clinic, emergency room visits, hospitalization, interventions, and length of in-hospital stay). We also determined the possible effect of IDs on the useful life of devices, taking into account that ID episodes can present as multiple shocks when a shock does not revert the cause that triggered it. The items and associated costs were obtained from the relevant regional government of Catalonia decree (SLT/42/2012).2
Median follow-up was 2.5 years (0 days to 8.5 years), and 27 patients (11.9%) presented with an ID. In total, 42 clinical ID episodes were recorded. Incidence was 0.08 episodes per patent/year. The most frequent cause was nonventricular tachycardia (66.7%). Overdetection of T waves caused 16.7% of episodes and electrical noise detection, 11.9%. In 19% of episodes, more than 5 shocks were received.
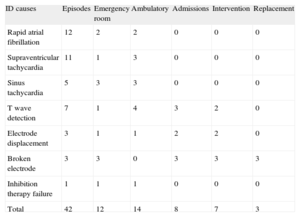
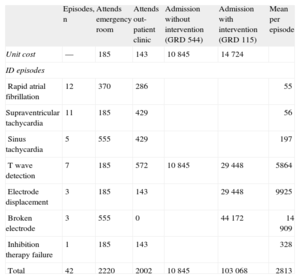
Tables 1 and 2 show resources used in the 42 episodes and their estimated economic cost, grouped as a function of ID cause. Twenty episodes led to medical examinations in the emergency room or outpatient clinics. Another 20 episodes were diagnosed in subsequent routine check-ups. These were single shock episodes, mostly for nonventricular tachycardia. The 2 remaining episodes occurred in patients hospitalized for another cause and the attention they received was not included as a cost. Eight episodes led to hospitalization. Hospitalizations were classified as a function of the diagnosis-related groups (DRG). Seven DRG 115 patients (implantation or replacement of generator or defibrillator electrode) and 1 DRG 544 patient (heart failure with major complications) were hospitalized. The DRG was the criterion used to determine the cost of hospitalization. Mean in-hospital stay was 4.4 days. Seven patients underwent reinterventions with ID, due to broken electrode (3), electrode displacement (2) and T wave overdetection (2). Total expense attributable to these incidents for all 42 episodes was €118 135.
Use of Hospital Resources as a Function of Causes of Inappropriate Discharge
| ID causes | Episodes | Emergency room | Ambulatory | Admissions | Intervention | Replacement |
| Rapid atrial fibrillation | 12 | 2 | 2 | 0 | 0 | 0 |
| Supraventricular tachycardia | 11 | 1 | 3 | 0 | 0 | 0 |
| Sinus tachycardia | 5 | 3 | 3 | 0 | 0 | 0 |
| T wave detection | 7 | 1 | 4 | 3 | 2 | 0 |
| Electrode displacement | 3 | 1 | 1 | 2 | 2 | 0 |
| Broken electrode | 3 | 3 | 0 | 3 | 3 | 3 |
| Inhibition therapy failure | 1 | 1 | 1 | 0 | 0 | 0 |
| Total | 42 | 12 | 14 | 8 | 7 | 3 |
ID, inappropriate discharge.
Distribution of Health Care Costs as a Function of Causes of Inappropriate Discharge
| Episodes, n | Attends emergency room | Attends out-patient clinic | Admission without intervention (GRD 544) | Admission with intervention (GRD 115) | Mean per episode | |
| Unit cost | — | 185 | 143 | 10 845 | 14 724 | |
| ID episodes | ||||||
| Rapid atrial fibrillation | 12 | 370 | 286 | 55 | ||
| Supraventricular tachycardia | 11 | 185 | 429 | 56 | ||
| Sinus tachycardia | 5 | 555 | 429 | 197 | ||
| T wave detection | 7 | 185 | 572 | 10 845 | 29 448 | 5864 |
| Electrode displacement | 3 | 185 | 143 | 29 448 | 9925 | |
| Broken electrode | 3 | 555 | 0 | 44 172 | 14 909 | |
| Inhibition therapy failure | 1 | 185 | 143 | 328 | ||
| Total | 42 | 2220 | 2002 | 10 845 | 103 068 | 2813 |
DRG, diagnosis-related groups; ID, inappropriate discharge.
Unless otherwise indicated, values express €.
Forty-nine devices were indicated for replacement due to low battery levels, 12 in the ID group and 37 in the non-ID group. Mean device life was 4.2 (2.2) years and 5.2 (1.6) years, respectively (P=.03). Mean device cost of the 227 implantations was €20 810 per unit. The 19.2% reduction in device life represents a mean cost of €3996 per device with ID.
We must remember that the economic value of the resources used was determined by our context at the time of the study, and this may differ in other situations. Furthermore, our calculation was based on the use of specific health care resources but we did not consider costs associated with the undoubtedly unfavorable effects of shocks—particularly inappropriate shocks—on psychosocial factors, quality of life, and overall mortality.
Our study found the economic cost of ID-related medical attention is distributed unequally; 42.8% of episodes were treated without using any of the resources studied and 96.4% of total costs were related to the 8 in-hospital episodes. We must distinguish between the cost of ID episode-related medical attention as such, and the cost of treating the cause. The first is low, since half of the episodes did not generate extra visits and were diagnosed at subsequent routine check-ups; moreover, diagnosis and therapeutic decision-making took place at a single visit. We put the cost of this at a mean €100 per episode. Treatment of ID-causes gives rise to costs that differ greatly as a function of these causes. Most are treated by reprogramming and/or adjusting medication, at no additional cost. However, 19% of episodes required hospitalization and reintervention, with high costs attributable more to the complication causing the ID than to ID itself (mean €14 239). Moreover, ID shortens the useful life of devices, at an estimated mean cost of some €4000 per device with ID.
FUNDINGStudy financed by Medtronic.