Heart failure (HF) is a public health issue due to its increasingly high incidence and prevalence, high morbidity and mortality, and the significant associated resource use.1 Although there are several initiatives in Spain that aim to implement HF-specific care models, information is lacking on the distribution and complexity of these patients and, therefore, their classification according to their theoretical care needs. One of the systems used for this purpose is known as the Kaiser pyramid, developed in the United States.2 This allows classification of patients into risk categories and the intensity of recommended health interventions. The base of the pyramid represents healthy individuals and those that are acutely unwell. In the middle segments are those with a chronic disease for whom health care efforts should be directed at disease management. The top level represents complex chronic patients, for whom health care efforts should focus on individual case management.2
The aim of this study was to classify the entire population with a diagnosis of HF in the Valencian Community in Spain according to the Kaiser pyramid categories.
This was a cross-sectional descriptive study of patients with a diagnosis of HF in the Valencian Community in 2015, selected from a population of 4 709 115 patients with a health card and registered with a named physician. HF was defined using the following codes from the International Classification of Diseases 9th Revision, Clinical Modification: 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93 and 428.XX.3
The study population was classified according to the 9 health statuses, with up to 6 levels of severity per health status, of the clinical risk groups (CRGs), which are a tool for dividing the population according to disease burden.3 These 9 health statuses were grouped into the 4 Kaiser complexity levels: a) healthy or with acute illness: health statuses 1 and 2 of the CRGs; b) low-complexity chronic disease: health statuses 3, 4 and 5 (severity levels 1, 2 and 3) of the CRGs; c) moderately-complex chronic disease: health statuses 5 (severity levels 4 and 5), 6 (severity levels 1 to 4), 7 (severity levels 1 and 2), 8 (severity levels 1 and 2) and 9 (severity levels 1 and 2) of the CRGs, and d) highly-complex chronic disease: health statuses 5 (severity level 6), 6 (severity levels 5 and 6), 7 (severity levels 3 to 6), 8 (severity levels 3 to 5) and 9 (severity levels 3 to 6) of the CRGs. Further details on each of the CRG categories are provided in the supplementary material. The information was obtained from the Alumbra information platform of the Valencian Community Consellería de Sanitat Universal i Salut Pública (Department of Universal Health and Public Health).
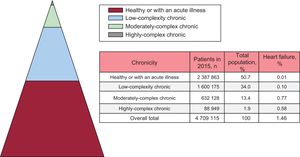
The distribution of the total population by Kaiser pyramid category showed that 50.7%, 34.0%, 13.4% and 1.9% were healthy or had acute illness, had low-complexity chronic disease, moderately-complex chronic disease, and highly-complex chronic disease, respectively (Figure 1).
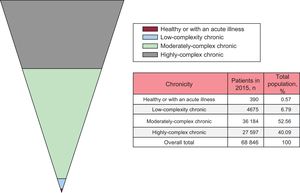
For HF, the prevalence for the 2015 period was 1.46% (68 846 patients). The distribution of patients with a diagnosis of HF by Kaiser pyramid category is shown in Figure 2. Unlike the observations in the general population, the distribution took the form of an inverted pyramid: most patients with HF had at least moderately-complex disease (52.56%), which was severe in 27 597 patients (40.09%).
The findings presented here highlight that most patients with HF have high care needs due to their complexity. According to the Kaiser pyramid postulates, patients with high-complexity illness need personalized health care management with the dual aim of: a) improving clinical prognosis and patient satisfaction, and b) reducing the use of health care resources.
The results presented here, in combination with the future prospects of an increase in HF prevalence, should serve as a warning call for health care systems to turn their attention to a reorganization that allows delivery of equal care that is appropriate for patients’ complexity level. In Spain, HF-specific care pathways have been developed and implemented, although unfortunately with uneven geographical distribution at the national level.1,4,5
In our opinion, the use of systems that can be adapted according to CRG could be a simple starting method when selecting the type of intervention in HF. However, it should be noted that this categorization is somewhat generic. Further tools will likely be needed to describe in more detail the health care needs of patients with more complex needs.
FUNDINGThis study was partly funded by grants from the Instituto del CIBER Cardiovascular 16/11/00420 FEDER and PIE15/00013.