Vitamin K antagonists (VKAs) have been shown to be effective in the prevention of thromboembolic complications in distinct clinical situations, including atrial fibrillation. However, VKAs are not exactly equivalent. Genetic polymorphisms are affected differently according to the type of VKA. The CYP2C9 isoenzyme would appear to be more important for warfarin clearance than for acenocoumarol or phenprocoumon clearance.1 Although warfarin is the most widely used VKA, in some countries, acenocoumarol or phenprocoumon are used.2
In Spain, the most widely used VKA is acenocoumarol. However, most of the available evidence on the efficacy and safety of VKAs is derived from warfarin. The results obtained with this VKA have in general been extrapolated to the other VKAs.
PAULA is a cross-sectional study whose objective was to determine the degree of anticoagulation control in the preceding 12 months in patients with nonvalvular atrial fibrillation who received anticoagulation therapy with a VKA in the primary health care setting in Spain. The degree of anticoagulation control was determined by time in therapeutic range, using both a direct method (poor control < 60%) and the Rosendaal method (poor control < 65%).3
The objective of the present analysis was to determine whether there were differences in the clinical profile, anticoagulation control, and thromboembolic/bleeding events according to type of VKA. A total of 1524 patients were included. Of these, 79 (5.2%) were taking warfarin (1127 international normalized ratio [INR] assessments; 14.4±0.12 assessments/patient) and the rest were taking acenocoumarol (94.8%). Warfarin use varied according to autonomous community: Catalonia (n=201), 16.92%; Andalusia (n=263), 9.89%; Galicia (n=150), 6.67%; Balearic Islands (n=33), 6.06%; Chartered Community of Navarre (n=24), 4.17%; Principality of Asturias (n=54), 3.70%; Canary Islands (n=56), 3.57%; Aragon (n=63), 1.59%; Region of Murcia (n=53), 1.89%; Valencian Community (n=123). 0.81%; and Cantabria (n=11), Castile-La Mancha (n=72), Castile and León (n=58), Extremadura (n=70), Community of Madrid (n=206), and the Basque Country (n=87), < 0.5%.
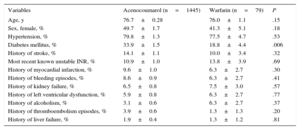
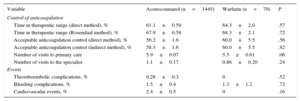
Except for a larger proportion of patients with diabetes mellitus among those treated with acenocoumarol, the remaining clinical characteristics were similar for both groups (Table 1). The degree of anticoagulation control was similar for both types of VKA. The number of visits both to the primary care physician and to the specialist for anticoagulation control was similar for both VKAs. Likewise, there were no differences in terms of the incidence of thromboembolic, bleeding, or cardiovascular events (Table 2).
Baseline Characteristics of the Patients in the PAULA Study
| Variables | Acenocoumarol (n=1445) | Warfarin (n=79) | P |
|---|---|---|---|
| Age, y | 76.7±0.28 | 76.0±1.1 | .15 |
| Sex, female, % | 49.7±1.7 | 41.3±5.1 | .18 |
| Hypertension, % | 79.8±1.3 | 77.5±4.7 | .53 |
| Diabetes mellitus, % | 33.9±1.5 | 18.8±4.4 | .006 |
| History of stroke, % | 14.1±1.1 | 10.0±3.4 | .32 |
| Most recent known unstable INR, % | 10.9±1.0 | 13.8±3.9 | .69 |
| History of myocardial infarction, % | 9.6±1.0 | 6.3±2.7 | .30 |
| History of bleeding episodes, % | 8.6±0.9 | 6.3±2.7 | .41 |
| History of kidney failure, % | 6.5±0.8 | 7.5±3.0 | .57 |
| History of left ventricular dysfunction, % | 5.9±0.8 | 6.3±2.7 | .77 |
| History of alcoholism, % | 3.1±0.6 | 6.3±2.7 | .37 |
| History of thromboembolism episodes, % | 3.9±0.6 | 1.3±1.3 | .20 |
| History of liver failure, % | 1.9±0.4 | 1.3±1.2 | .81 |
INR: international normalized ratio.
Control of Anticoagulation and Events in the PAULA Study
| Variable | Acenocoumarol (n=1445) | Warfarin (n=79) | P |
|---|---|---|---|
| Control of anticoagulation | |||
| Time in therapeutic range (direct method), % | 61.1±0.59 | 64.3±2.0 | .57 |
| Time in therapeutic range (Rosendaal method), % | 67.9±0.58 | 68.3±2.1 | .72 |
| Acceptable anticoagulation control (direct method), % | 56.2±1.6 | 60.0±5.5 | .56 |
| Acceptable anticoagulation control (indirect method), % | 58.3±1.6 | 60.0±5.5 | .82 |
| Number of visits to primary care | 5.9±0.07 | 5.5±0.61 | .06 |
| Number of visits to the specialist | 1.1±0.17 | 0.86±0.20 | .24 |
| Events | |||
| Thromboembolic complications, % | 0.28±0.3 | 0 | .52 |
| Bleeding complications, % | 1.5±0.4 | 1.3±1.2 | .72 |
| Cardiovascular events, % | 2.4±0.5 | 0 | .16 |
The data from this analysis indicate that, in Spain, there are no significant differences in the clinical characteristics (except for diabetes mellitus), anticoagulation control, or thromboembolic/bleeding complications according to the type of VKA used. This information is relevant as there are few publications that compare the 2 treatments.4–6
Two previous studies have compared the degree of anticoagulation control for the 2 drugs. The first, conducted in Spain but limited to a single hospital (120 patients treated with acenocoumarol and 120 with warfarin), reported that although there was a higher risk of INR ≥ 6, there were no differences in the percentage of visits in which INR was within the therapeutic range.4 In another study, conducted 20 years ago in a single center in Italy, anticoagulation control appeared to be better with warfarin.5
In terms of efficacy and safety, no randomized trials have compared these 2 alternatives. Data are, however, available from the EINSTEIN-DVT (NCT00440193), an open-label study that randomized patients with acute symptomatic deep vein thrombosis to rivaroxaban or enoxaparin followed by a VKA, which could be either warfarin or acenocoumarol, for 3, 6, or 12 months. The efficacy results were independent of the type of VKA,6 indicating that the efficacy of the 2 VKAs could be similar.
Although the design of our study does not allow determination of the reason for prescribing warfarin or why these differences in prescription vary according to autonomous community, given the difference in half-life of the VKA, the physicians may have switched to warfarin because of inadequate INR control with acenocoumarol. However, our data show that INR control is similar with acenocoumarol and warfarin.
The main limitation of this study is the small sample size with warfarin, thereby reducing the statistical power of the comparisons. However, this situation reflects what occurs in clinical practice in Spain, where warfarin use is very limited.
The data show that warfarin use is limited (5.2%), but with noteworthy differences between autonomous communities. The data also show that there are no differences in anticoagulation control and cardiovascular events. These findings would seem to support the usual practice of extrapolating to acenocoumarol results obtained with warfarin in large clinical trials of nonvalvular atrial fibrillation.
CONFLICTS OF INTERESTThe study was sponsored by Bayer Hispania S.L. The sponsor had no influence on study conduct or data collection and interpretation.