To the Editor,
Cor triatriatum dexter (CTD) is a very rare defect in which the right atrium is divided into 2 chambers by a membrane. It has an estimated incidence of around 0.025% of all congenital heart diseases. We present 2 cases of CTD in adults diagnosed in our echocardiography laboratory; there were no clinical consequences in either case.
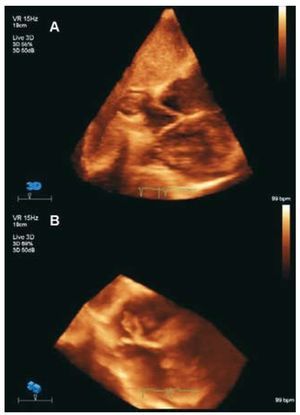
The first case was a 76-year-old woman referred for transthoracic echocardiography due to dyspnea. Severe aortic stenosis was diagnosed; furthermore, a partition in the right atrium was shown, with insertion into the interatrial septum and its base, dividing it into 2 compartments communicating through fenestrations in the partition, without interfering with filling flow. The diagnosis of CTD (Figure 1) was confirmed by 3D echocardiography.
Figure 1.A: membrane dividing the right atrium visualized by 3D-echocardiography in the subcostal view. B: flow of contrast medium from the posterior chamber to the anterior.
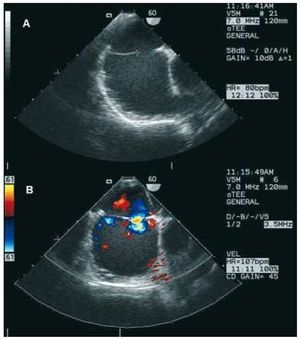
The second case concerns a 68-year-old women with a medical history of hypertension. Echocardiography showed a membrane running from the lateral side of the right atrium (contiguous with the mouth of the inferior vena cava) up to the interatrial septum. In view of these findings, a transesophageal study (Figure 2) was conducted and CTD was confirmed. The membrane began in the interatrial septum, contiguous with the mouth of the coronary sinus, and ran along the lateral side of the right atrium, leaving a 15-mm defect (with accelerated color Doppler flow at that level, although without obstructing the flow) and forming an entry chamber into which the venae cavae opened and another chamber from the membrane to the tricuspid valve.
Figure 2.A: the membrane visualized by transesophageal echocardiography. B: flow of contrast medium between the 2 chambers through the fenestration.
In the fourth week of embryonic development, the common atrium is separated from the venous sinus by a valve with 2 leaflets (the venous sinus valve). During embryonic development, the left leaflet of the venous sinus valve is incorporated into the interatrial septum and forms part of the septum secundum. The right leaflet is reabsorbed around the 12th week of gestation, leaving 2 structures: the Eustachian valve at the junction of the inferior vena cava and the coronary valve at the mouth of the coronary sinus. To a greater or lesser extent, the persistence of the right leaflet of the venous sinus valve causes a wide range of defects, including a prominent Eustachian valve, the Chiari network, and CTD.1
CTD is frequently associated with right-side defects caused by abnormal fetal circulation. Among these, the most frequent are stenosis or atresia of the pulmonary valve, tricuspid valve abnormalities and atrial septal defect.2
Clinical signs depend on the degree of obstruction,1 and there may be an absence of symptoms. Furthermore, it can lead to trapped catheters, supraventricular arrhythmias, or embolisms.
CTD can be diagnosed by echocardiography2,3 and magnetic resonance imaging, although caution is needed since a prominent Eustachian valve can simulate the defect. Either of these imaging techniques can show the right atrium divided into 2 chambers: a posterior chamber into which the venae cavae drain, and an anterior one that contains the atrial appendage.
Asymptomatic patients should not be treated, unless referred to heart surgery for other reasons. In symptomatic patients with significant obstruction, the treatment of choice is surgical resection, although percutaneous correction of the membrane has been proposed as an alternative to surgical treatment.4