To the Editor,
The stress test, whether performed conventionally or with imaging techniques, is the most widely used method in clinical practice to demonstrate myocardial ischemia in patients with chest pain. A pharmacological stress test is usually indicated in patients who cannot do physical exercise. Although several drugs are currently available to induce ischemia, for many years dipyridamole has been the most widely used agent. This drug causes vasodilatation by inhibiting the reuptake of adenosine in the myocardium and dilatating the coronary arteries through the non-endothelium-dependent vascular smooth muscle A2 receptors. In patients with significant coronary stenosis, this form of vasodilatation causes flow redistribution ("coronary theft") and induces ischemia in the area of the diseased vessel. Ischemia is usually revealed by nuclear imaging, often with few electrocardiographic changes or with ST-segment depression.
ST-segment elevation is uncommon during conventional or pharmacological stress testing and indicates transmural ischemia in patients without previous myocardial infarction or necrosis Q waves. Transient ST-segment elevation tends to be a sign of coronary spasm. Coronary spasm is not expected following the administration of dipyridamole, given its role as a vasodilator. The mechanism by which ST-segment elevation can occur during dipyridamole stress testing remains unknown, although different hypotheses have been postulated: vasospasm,1 severe systemic arterial hypotension, and alterations in the coronary microcirculation.2
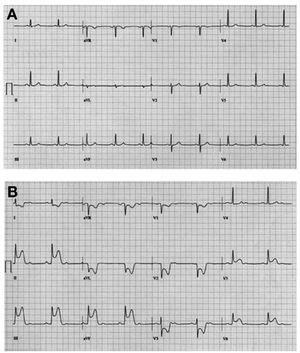
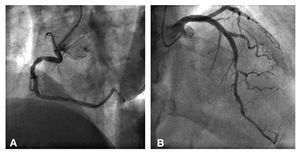
We report the case of a 71-year-old man, with hypertension and diabetes mellitus type 2 who was referred due to episodes of chest pain, that occurred during rest and evolved over 1 month. A pharmacological stress test with dipyridamole was performed because the patient was unable to make any physical effort due to degenerative joint disease. A dose of 0.57 mg/kg in 10 mL of physiological saline solution was intravenously administered over 4 minutes. Basal ECG (Figure 1A) showed sinus rhythm without alterations in the ST segment. Six minutes after beginning dipyridamole administration the patient presented chest pain. ECG showed ST-segment elevation in leads II, III, aVF, V5, and V6 (Figure 1B). Nitroglycerin and aminophylline were administered sublingually and the ECG normalized within 2 minutes. Blood pressure remained within the normal range. Coronary angiography showed nonsignificant atherosclerotic plaque in the proximal right coronary artery (Figure 2A) and 70% stenosis of the middle segment of the anterior descending coronary artery (Figure 2B). A drug-eluting stent was implanted in the descending anterior artery, with a good angiographic outcome.
Figure 1. A: basal ECG in sinus rhythm without ST-segment alterations. B: ECG 6 minutes after administration of dipyridamole. Consistent with signs of angina, there is a second-degree AV block and ST-segment elevation in leads II, III, aVF, and V5-V6.
Figure 2. Coronary angiography. A: nonsignificant lesion in the proximal right coronary artery. B: 70% stenosis in the middle segment of the anterior descending coronary artery.
This was an unusual case of ST-segment elevation with dipyridamole administration in a patient with resting angina associated with probable vasospasm. Some authors have suggested that coronary spasm is a rebound effect that occurs after dipyridamole has terminated its vasodilator activity3 and when there is multivessel disease,4 but not when there is a only one significant lesion. Coronary angiography showed a nonsignificant stenosis in the right coronary artery that may have acted as the substrate of the spasm, correlating with ST-segment elevation in the inferior leads.
In conclusion, we think that the possibility of coronary spasm as a rare adverse effect should be taken into account when performing pharmacological stress testing with dipyridamole. More studies are needed to determine the mechanism by which this vasodilator can induce vasospasm.