We present the case of a 4-month-old male infant (6.4kg) referred to our center from another hospital with incessant tachycardia with poor clinical tolerance. On admission, ECG showed a regular tachycardia at 190 bpm, with narrow QRS, clearly visible P waves, which were negative in the inferior leads, an AV ratio of 1:1, and an RP interval longer than the PR interval, all of which suggested a permanent junctional reciprocating tachycardia or Coumel tachycardia (Figure 1). Echocardiography showed severe left ventricular failure with a shortening fraction of 14%. He was therefore admitted to the neonatal intensive care unit.
The tachycardia could not be controlled despite electrical cardioversion and antiarrhythmic drugs (esmolol, amiodarone), with immediate recurrence. Over the following hours, he deteriorated clinically and developed cardiogenic shock; adequate cardiac output could not be achieved despite inotropic drugs. Therefore, extracorporeal membrane oxygenation (ECMO) was started for hemodynamic support via the right carotid artery and jugular vein.
The following day the patient underwent an electrophysiological study with ECMO support. The electrode catheters were introduced via the right femoral vein. Standard stimulation maneuvers were performed, confirming the diagnosis and the presence of a midseptal concealed accessory pathway with slow conduction.
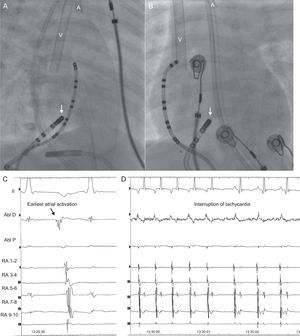
Initially, ablation was aimed at the point of earliest retrograde atrial activation, using a radiofrequency catheter with a 4-mm point/tip (Marinr 5 Fr, Medtronic Inc; Minneapolis, USA). Although this had transient success, the temperature (55°C) repeatedly limited application, reaching very low power (4 W), and the arrhythmia recurred within a few seconds. Even with small movements of the catheter, higher power could not be achieved. On the assumption that there was low flow in the right atrium, due to the ECMO removing blood from the right atrium, a 6-mm cryoablation catheter was introduced (7 Fr, Freezor Xtra, Medtronic Inc; Minneapolis, USA). During the cryomapping (-35°C), the tachycardia was interrupted by a retrograde block in the accessory pathway, which did not affect atrioventricular conduction (Figure 2A, Figure 2B, Figure 2C, Figure 2D). Therefore, cryoablation (–80°C) was applied for 240seconds. The patient progressed well after the procedure, ECMO and the vasoactive drugs were weaned, and he was finally discharged at 3 weeks. The ejection fraction was completely normalized at 3 months and, to date, there have been no recurrences.
Right anterior oblique (A) and posteroanterior (B) radiological projections showing the position of the cryoablation catheter in the midseptal region (arrow), where the earliest atrial activation was recorded (C). During cryomapping of this point, the tachycardia was terminated (D). Note the venous (V) and arterial (A) cannulae on the fluoroscopy images.
Permanent junctional reciprocating tachycardia is an uncommon form of supraventricular tachycardia, mediated by an accessory pathway with slow conduction, which is usually located in the posteroseptal region. It typically presents in the first few decades of life, particularly in infants and, due to the slow conduction properties of the accessory pathway, it is often incessant, which can lead to tachycardiomyopathy in up to 18% of patients. However, inotropic drugs and hemodynamic support are rarely needed.1 In this case, the patient's unfavorable clinical progression to refractory cardiogenic shock necessitated ECMO.
Although antiarrhythmic drugs are the first-line treatment for these arrhythmias, most patients need ablation to avoid recurrence in the long-term. In experienced centers, ablation can have high success rates and a low risk of complications even in infants.1,2
Radiofrequency is the most commonly used energy source for catheter ablation. To ensure that the lesion created is permanent, sufficient power must be effectively delivered to the tissue. However, when applied to areas of low flow (such as inside the coronary sinus), there is insufficient cooling of the catheter tip. The tip heats up rapidly and reaches the temperature limit, and adequate power cannot be reached. In this case, the removal of blood by the ECMO venous cannula caused low flow in the right atrium, which limited the power delivery with conventional radiofrequency. Irrigated-tip catheters are the most frequently used solution for this problem.3 However, there are few experimental or clinical data on the effects of applying irrigated-tip catheters to the developing myocardium, such as that of children.4
In this case, cryoablation was used as an alternative energy source to get around this limitation. Cryoablation also has an excellent safety profile, which has made it the treatment of choice for perinodular tissue in many centers performing ablation in pediatric patients. However, we must remember that the currently available catheters are stiff and relatively large, so their use in small children is limited.5
This case demonstrates a new advantage of cryoablation: the creation of an effective lesion is independent of the surrounding flow, which is important in patients requiring external hemodynamic support (ECMO).
CONFLICTS OF INTERESTF. Atienza is an advisor at Medtronic.