The diagnostic value of myocardial ischemia tests is influenced by the pretest probability of coronary artery disease, which is essentially determined by the clinical characteristics of chest pain and the age and sex of the patient. It has been suggested that subclinical atherosclerotic carotid artery disease detected by ultrasound might be associated with an increased risk of heart disease. The 2013 ESC guidelines on the management of stable coronary artery disease recommends the use of carotid ultrasound to evaluate the presence of plaque and measure carotid intima-media thickness (CIMT) in patients with suspected coronary disease but without demonstrated atherosclerotic disease (recommendation IIa with level of evidence C).1 The recommendation is based on expert consensus opinion but is not supported by evidence from specific studies. We wished to investigate whether an increase in CIMT with or without the presence of plaque on a carotid ultrasound performed before an exercise echocardiogram is associated with a positive result.
We studied patients with chest pain referred from the cardiology department of our hospital for exercise echocardiography. Patients with a history of coronary disease or segmental wall-motion abnormalities in the baseline echocardiogram were excluded. CIMT measurements were taken for both carotid arteries over a 1-cm segment in the posterior wall, 1cm from the bulbs. Mean CIMT values have been shown to provide a better indication of atherosclerotic burden in hypertensive patients,2 and a CIMT of over 0.9mm is considered to be a marker of target organ damage.
The exercise echocardiogram was considered to be positive if it induced wall-motion abnormalities in at least 2 contiguous segments.
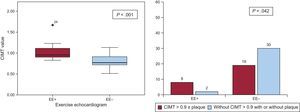
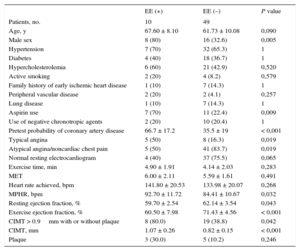
Fifty-nine patients (mean age, 62.7 years; 59% women) with no history of heart disease were studied. Their characteristics are summarized in the Table. The probability of coronary artery disease based on the manifestations of chest pain and the age and sex of the population was 40% (95%CI, 35.1-46.5). Twenty-seven patients (45%), 16 (59%) of whom were men, had carotid artery disease (CIMT > 0.9mm with or without plaque). The exercise echocardiogram was positive in 10 patients (16%), 8 of whom were men (80%). No complications were observed during the tests. A positive exercise echocardiogram was significantly associated with carotid artery disease (Figure).
Characteristics of Patients According to Exercise Echocardiogram Result
| EE (+) | EE (–) | P value | |
|---|---|---|---|
| Patients, no. | 10 | 49 | |
| Age, y | 67.60 ± 8.10 | 61.73 ± 10.08 | 0,090 |
| Male sex | 8 (80) | 16 (32.6) | 0,005 |
| Hypertension | 7 (70) | 32 (65.3) | 1 |
| Diabetes | 4 (40) | 18 (36.7) | 1 |
| Hypercholesterolemia | 6 (60) | 21 (42.9) | 0,520 |
| Active smoking | 2 (20) | 4 (8.2) | 0,579 |
| Family history of early ischemic heart disease | 1 (10) | 7 (14.3) | 1 |
| Peripheral vascular disease | 2 (20) | 2 (4.1) | 0,257 |
| Lung disease | 1 (10) | 7 (14.3) | 1 |
| Aspirin use | 7 (70) | 11 (22.4) | 0,009 |
| Use of negative chronotropic agents | 2 (20) | 10 (20.4) | 1 |
| Pretest probability of coronary artery disease | 66.7 ± 17.2 | 35.5 ± 19 | < 0,001 |
| Typical angina | 5 (50) | 8 (16.3) | 0,019 |
| Atypical angina/noncardiac chest pain | 5 (50) | 41 (83.7) | 0,019 |
| Normal resting electrocardiogram | 4 (40) | 37 (75.5) | 0,065 |
| Exercise time, min | 4.90 ± 1.91 | 4.14 ± 2.03 | 0,283 |
| MET | 6.00 ± 2.11 | 5.59 ± 1.61 | 0,491 |
| Heart rate achieved, bpm | 141.80 ± 20.53 | 133.98 ± 20.07 | 0,268 |
| MPHR, bpm | 92.70 ± 11.72 | 84.41 ± 10.67 | 0,032 |
| Resting ejection fraction, % | 59.70 ± 2.54 | 62.14 ± 3.54 | 0,043 |
| Exercise ejection fraction, % | 60.50 ± 7.98 | 71.43 ± 4.56 | < 0,001 |
| CIMT > 0.9mm with or without plaque | 8 (80.0) | 19 (38.8) | 0,042 |
| CIMT, mm | 1.07 ± 0.26 | 0.82 ± 0.15 | < 0,001 |
| Plaque | 3 (30.0) | 5 (10.2) | 0,246 |
EE, exercise echocardiogram; CIMT, carotid intima-media thickness; MPHR, maximum predicted heart rate.
Data expressed as No. (%) or mean ± SD unless specified otherwise.
The odds ratio for an association between a CIMT of over 0.9mm (with or without plaque) and a positive exercise echocardiogram was 6.3 (95%CI, 1.2-33.3). The following factors were also associated with a positive result: a higher pretest probability of coronary artery disease, the presence of typical angina, baseline ejection fraction (> 55% in all cases), prior use of aspirin, and male sex.
Ours is the first study to specifically analyze the ability of CIMT to predict a positive exercise echocardiogram. An association between carotid disease and coronary artery disease has previously been described. While the study in question did not detect an association between carotid disease and exercise echocardiography, the presence of carotid plaque appeared to increase the predictive power of the stress test for diagnosing coronary artery disease.3 The main limitation of our study is the few patients analyzed and the small number of positive exercise echocardiograms. The sample, however, was large enough to test the hypothesis with sufficient statistical power. Larger studies are needed to further investigate the variables identified as independent predictors of a positive echocardiogram. The results of our study support the recommendations in the 2013 ESC guidelines.1 While it is known that a positive ischemia test is not synonymous with obstruction of the main epicardial coronary arteries, a negative exercise echocardiogram is associated with good prognosis (1-year mortality of < 1%),4 and a positive echocardiogram is associated with worse prognosis, even in patients without angiographically significant coronary artery disease.5
The findings of a recent study suggest that exercise electrocardiography had little prognostic value in patients with a low pretest probability of coronary artery disease,6 and standard risk scales have also been claimed to have low predictive power.
In conclusion, CIMT measurement offers additional information, and by modifying the pretest probability of coronary artery disease, it may help to guide decision-making. Finally, detection of carotid disease should encourage clinicians to implement more active cardiovascular disease prevention measures.