Cardiovascular disease (CVD) remains the leading cause of death in most countries; however, few specific political actions have been implemented to improve cardiovascular health at both national and international levels. We aimed to describe the methodology used for the development and initial rollout of Spain's Cardiovascular Health Strategy of the National Health System (ESCAV, Estrategia en Salud Cardiovascular del Sistema Nacional de Salud).
MethodsA multidisciplinary team comprising diverse stakeholders developed a national strategy to reduce the burden of CVD in Spain. The team used qualitative methodologies to identify and select priorities and design strategic map models.
ResultsThe strategy was structured around a matrix with 6 cross-cutting themes (citizen empowerment; health promotion, prevention, and early CVD detection; comprehensive management of acute and chronic CVD; health care coordination; equity; and knowledge management) and 4 longitudinal lines (ischemic heart disease, heart failure, arrhythmias, and valve disease). The framework was further supported by 3 overarching axes: continuity of care, patient safety, and leveraging of information systems. A total of 27 critical points were selected, leading to the definition of 99 strategic objectives (32 general and 67 specific) and 136 actions through iterative reviews and prioritization. Strategic maps were developed for the overall strategy and for each action line, incorporating 61 indicators to facilitate and monitor the development of the strategy.
ConclusionsESCAV represents one of the most ambitious initiatives aimed at transforming a nation's cardiovascular health. The methods and steps undertaken in this process could serve as a valuable reference for other countries seeking to establish similar initiatives. Furthermore, it may act as a catalyst to advance efforts toward establishing a European plan for cardiovascular health.
Keywords
Significant advances in the prevention and treatment of cardiovascular disease (CVD) have been achieved in recent years. However, CVD remains the leading cause of death and a major cause of morbidity in Europe and many other regions.1 Worse cardiovascular health,2,3 along with cardiovascular risk factors4,5 and CVD, leads to substantial health care costs and imposes a significant burden for patients, families and society in Spain and worldwide.6 This situation poses a major challenge for health care systems. Despite this, there are few national plans specifically designed to enhance cardiovascular health and mitigate the burden of CVD through a comprehensive approach. Unlike cancer,7 there is no specific European plan to combat CVD.
In response to these challenges, and with the aim of reducing the burden of CVD in Spanish society while promoting equity in cardiovascular health promotion, prevention, and care among its 17 regions, the Spanish Ministry of Health developed its first national Strategy on Cardiovascular Health of the National Health System (ESCAV, Estrategia en Salud Cardiovascular del Sistema Nacional de Salud), which was released in 2022. This manuscript aims to summarize the methodology for the development of the ESCAV, outline its main content, and describe the initial steps for its implementation. It is intended as a potential model for other countries or as a reference for the development of a European plan.
METHODSBackground. Spain's National Health SystemSpain has a decentralized administrative and political organization, comprising 17 autonomous regions and 2 autonomous cities (Ceuta and Melilla). These autonomous regions and cities (ARCs) are responsible for local public health services and the planning and management of local health care services. The Spanish National Health System (NHS) operates under a mixed competency model, where regional responsibilities are combined with the coordination functions of the Ministry of Health.
The Spanish Ministry of Health is responsible for the design and development of national health plans and strategies, as well as creating specific tools to promote cohesion in services provided across the NHS and to ensure regional equity in the quality of health care provision. The distinction between national plans and strategies lies in budget allocation: the former includes a specifically allocated budget from the Ministry of Health, while the latter does not. Notably, the central government annually transfers a designated budget for health care to the ARCs from the general state budget. This funding must cover the benefits of the Common Portfolio of Services defined by Spanish law and the actions approved by the Interterritorial Council.
Each strategy or plan is coordinated by the Ministry of Health and developed in collaboration with key stakeholders, including health authorities from ARCs, scientific societies, patient associations, and experts from academia. Proposals are submitted to the Interterritorial Council, an official forum comprising representatives from all regional health authorities. To move forward, these proposals must receive unanimous approval from all members to progress. Subsequently, regional health services adapt these strategies or plans to their local resources and needs, establishing their own priorities, implementation plans, timelines, and action plans.
The Cardiovascular Health Strategy: conception and designIn 2018, the Spanish Ministry of Health decided to update the previous CVD Strategy (the Strategy for Ischemic Heart Disease, approved in 2006 and last updated in 2009)8,9 and expand its scope to include other cardiovascular diseases. To achieve this, an ad hoc scientific advisory board was appointed, comprising four experts in CVD care, hospital management, primary care management, and primary care nursing. The advisory board recommended a paradigm shift, proposing a focus on cardiovascular health rather than exclusively targeting cardiovascular disease.
AimsThe general aim of the ESCAV was to improve the cardiovascular health of the Spanish population. The specific aims of the plan included:
- a)
Facilitating the adoption of healthy and sustainable lifestyles by creating healthier environments.
- b)
Promoting cardiovascular prevention to reduce the incidence and prevalence of CVD in Spain.
- c)
Enhancing cardiovascular care through the early detection of CVD and the multidisciplinary and coordinated care of acute and chronic CVD, including health recovery and restoration, prevention of disability, and improvement of the quality of life and well-being of patients and their families.
- d)
Implementing measures that have proven to be safe, effective, efficient, and sustainable.
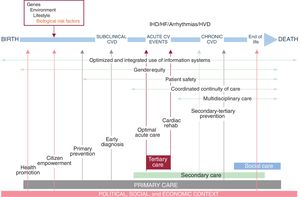
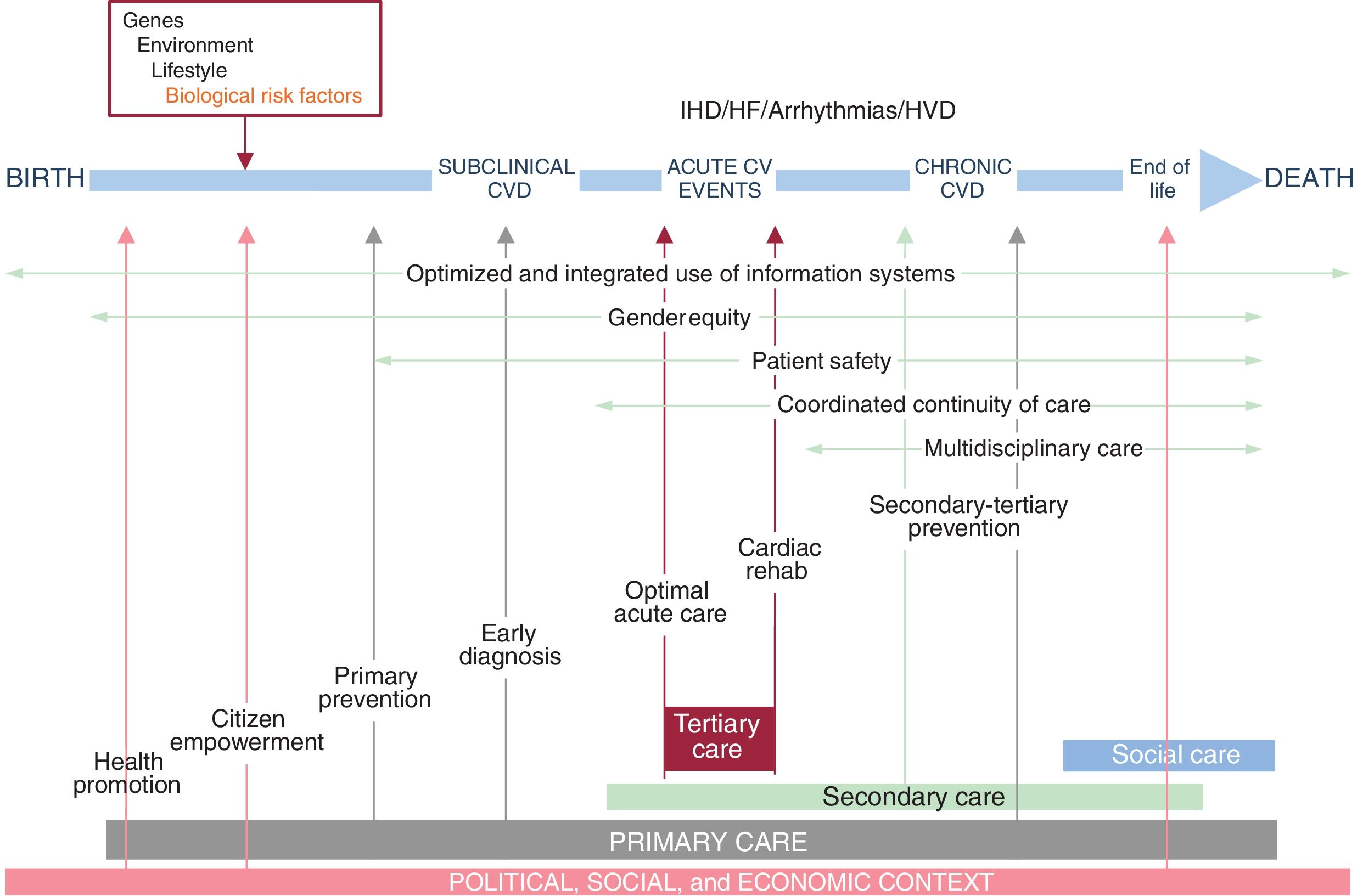
A comprehensive approach to cardiovascular health was adopted, emphasizing a person-centered perspective that addressed the key factors involved in maintaining or losing cardiovascular health, as well as the progression of disease trajectories. A theoretical framework was developed to illustrate individual trajectories from health to various forms of CVD, encompassing the main individual and social determinants, key stakeholders, settings, and opportunities for action (figure 1).
Central illustration. Conceptual person-centered framework of the trajectories from health to subclinical, clinical (acute or chronic) and end-stage cardiovascular disease (CVD), their determinants, settings, stakeholders, and opportunities for action. The model starts from childhood and includes the main factors involved in the maintenance or loss of health, including individual and social determinants of health, the different times and environments where these occur, the key stakeholders, and opportunities for action (ie, education of children and citizens on healthy lifestyles, cardiovascular health, changes for a healthier environment beyond the health system; early cardiovascular risk factors or subclinical disease detection in primary care; training of health care professionals and changing the health care system to improve the management of acute and chronic CVD from the beginning to the end of the process through a multidisciplinary approach to continuity in acute and chronic CVD care. CV, cardiovascular; HF, heart failure; IHD, ischemic heart disease; HVD, heart valve disease.
A Multidisciplinary Advisory Committee, composed of relevant stakeholders—patients, health care professionals (cardiologists, primary care physicians, public health specialists, other medical specialists, and nurses), managers, researchers, technology development experts, representatives of the Ministry of Health, and representatives from ARCs—was established to select and prioritize a number of action lines within the defined strategic framework. Committee members were appointed by ministry representatives and/or the strategy coordinators, based on technical expertise, experience, previous collaboration or their capacity to represent collective interests.
StructureA general framework for the structure of the document was subsequently proposed. Three overarching strategic axes were identified to guide for the entire strategy: continuity of care, patient safety, and the use of information systems to guide and monitor changes. In alignment with the specific aims of the strategy, 6 general cross-cutting themes were defined:
- a)
Health promotion, disease prevention, and early detection.
- b)
Citizen empowerment and participation.
- c)
Equity (with a special focus on gender equity).
- d)
Comprehensive management of individuals with acute CVD.
- e)
Comprehensive management of individuals with chronic CVD.
- f)
Knowledge management, research, and innovation.
Given the wide variety of CVDs, 4 specific clinical areas were prioritized based on their societal burden (ie, incidence, prevalence, mortality, clinical impact, or rising trends): ischemic heart disease, heart failure, arrhythmias/sudden death, and heart valve disease. These priorities were identified as the longitudinal lines of the strategy. To design the strategic framework of ESCAV, a matrix was developed to define the relationships between the cross-cutting themes and the longitudinal lines. This matrix served as a tool for selecting priorities and structuring the strategy.
Each decision level within the matrix was required to define its own objectives (ends or goals), strategies (why, what for), actions (what, how, who, when, where), outputs (expected immediate results), outcomes (expected mid- and long-term results), and indicators (measurement criteria). These considerations were designed to incorporate the perspectives of various stakeholders, including citizens, patients, caregivers, professionals, and decision-makers.
The model used for the development of the ESCAV was intentionally designed to allow for replication or expansion. This flexibility ensures its applicability to other cardiovascular syndromes not addressed in this edition or even to other health areas. Within this framework, the following steps for the development of the ESCAV were taken:
Development methodologyAfter definition of the general structure and clinical areas, a sequence of actions for completing the design of the ESCAV was developed:
Design and development of the core content of the strategyFor the development of the ESCAV and the collaborative model, 3 ad hoc committees were designed, each with distinct functions:
- a)
Multidisciplinary Advisory Committee, organized into specific interdisciplinary working groups to develop the content of the cross-cutting themes and longitudinal lines. Each working group had a coordinator.
- b)
Technical Committee, composed of representatives from relevant scientific societies, patient associations, and selected individual experts to validate the proposals made.
- c)
Institutional Committee, including representatives from all Spanish autonomous communities and relevant ministerial units for final approval and implementation commitments.
The main initial activities of the Multidisciplinary Advisory Committee included:
- -
Identification, confirmation, and prioritization of critical points. The Nominal Group Technique was used to select priorities for the initial identification of critical points within each line.10 Prioritization was conducted using an abbreviated version of the Hanlon Method, which evaluates factors such as the magnitude and relevance of the problem, the effectiveness of proposed interventions, and their feasibility.11,12
- -
Strategic goal setting and action definition. Each interdisciplinary group defined at least 1 specific strategic goal and provided an initial definition of actions for each critical point selected, ideally choosing evidence-based interventions with a significant impact on cardiovascular health outcomes.
The initial document was evaluated and reviewed in a structured manner through the following steps. Subsequently, a strategic map of the ESCAV with specific scorecards was developed and approved.
- -
The ESCAV draft was presented to the Technical and Institutional Committees for external review and initial approval. This process included a thorough analysis and discussion of all critical points.
- -
Feedback on the proposed critical points, strategic objectives, and actions was compiled and reviewed. Specific indicators were defined to monitor the progress and outcomes of each action.
- -
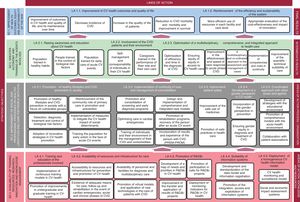
A preliminary strategic map encompassing the entire strategy was created. The map was designed based on Kaplan and Norton's model, incorporating the critical points, strategic objectives, and initial actions. It also defined four perspectives: two focused on results (customer satisfaction and the expected efficiency of products or services) and two on processes (excellence and continuous process improvement through the integration of knowledge and innovation).
- -
The Balanced Scorecard model13 was employed as a strategic tool to design the necessary processes to achieve the desired results while adhering to budget constraints, and to monitor the implementation and results of the ESCAV.
- -
Following several revisions and adjustments by the Technical and Institutional Committees, the final version was submitted to the Interterritorial Council of the NHS for approval.
Figure 1 summarizes the philosophy and key components of Spain's Cardiovascular Health Strategy of the NHS.
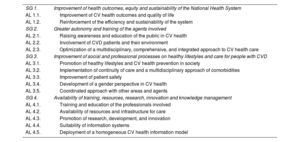
Overview of the strategy development workflowThe Multidisciplinary Advisory Committee consisted of 67 members from 16 disciplines, including patients (a complete list of members is available in the supplementary data). All members were briefed on the aims and workflow of the initiative. During the first meeting, the committee focused on identifying and prioritizing the critical points required to improve cardiovascular health and CVD care in Spain. This process initially resulted in the identification of 90 critical points. After iterative reviews, 27 critical points were established (table 1). For each critical point, specific objectives and specific actions were defined. The committee outlined four general strategic goals (SG) and 15 action lines (AL) (table 2). Following a waterfall structure (), 99 strategic objectives (32 general and 67 specific, ) and 136 actions were finally proposed. A strategic map for the entire Cardiovascular Health Strategy was developed (figure 2 shows an example), along with individual maps for each action line.14
Final critical points selected in the Spanish Cardiovascular Strategy on Cardiovascular Health (ESCAV)
| Critical points associated with strengthening the central strategic axes |
| Promote and strengthen continuity of care as a key element of high quality, efficient and safe health care for patients with CVD |
| Promote safe practices in the care of patients with CVD |
| Improve access to reliable information to comprehensively identify the status of CV health and CVD care in the Spanish population |
| Critical points associated with health promotion, disease prevention, and citizen empowerment in CV health |
| Promote CV health and CVD prevention among the population of Spain |
| Raise awareness about primary CVD prevention, focusing on lifestyle: tobacco use as a key target |
| Promote primary CVD prevention through the monitoring of biological risk factors |
| Increase the ability of health professionals and other professionals to promote CV health and CVD prevention |
| Encourage public empowerment to adopt healthy lifestyles |
| Critical points associated with knowledge management, research and innovation in CV health |
| Focus the training of health professionals on research and innovation for the improvement of CV health outcomes as far as possible throughout their training cycle |
| Carry out initiatives to equip citizens with self-care skills in CV health |
| Include patient-reported outcomes and experiences in institutional reports of patient outcomes |
| Identify research and innovation areas in CV health based on the needs and challenges of the NHS, considering health outcomes |
| Promote research projects and develop innovations addressing specific solutions to existing CV health needs, fostering collaboration and facilitating the transfer to a care approach |
| Promote epidemiological studies on differences in the prevalence of CVD influenced by gender or other inequities |
| Support initiatives regarding development models for virtual care and the improvement of outcomes in patients with CVD within the framework of the NHS's Digital Health Strategy |
| Critical points associated with equity and gender in CV health |
| Promote knowledge and self-care related to CV health among women |
| Train all NHS professionals in the specific aspects of CVD (diagnosis and treatment) in women and gender inequality in CV care |
| Address social inequalities in CV health in the Strategy's actions using an interdisciplinary approach |
| Critical points associated with the comprehensive management of persons with acute and chronic ischemic heart disease |
| Develop cardiac rehabilitation and secondary prevention programs in hospitals and primary care settings according to patient risk |
| Optimize the performance of acute coronary syndrome networks |
| Critical points associated with the comprehensive management of persons with acute and chronic HF |
| Improve the early detection and diagnosis of HF |
| Organize the care for HF patients through multidisciplinary HF units/programs, coordinated with the participation of all professionals involved at all levels of care |
| Develop specific regional networks to optimize the management of patients with cardiogenic shock |
| Critical points associated with the comprehensive management of persons with acute and chronic valve heart disease |
| Promote the early diagnosis of prevalent heart valve diseases |
| Optimize the choice of therapeutic options for patients with severe aortic stenosis through comprehensive multidisciplinary evaluation teams |
| Critical points associated with arrhythmias/sudden death |
| Improve the effectiveness of access to early cardiopulmonary resuscitation in patients with out-of-hospital cardiac arrest |
| Promote the early diagnosis of atrial fibrillation |
CVD, cardiovascular disease; CV, cardiovascular; HF, heart failure; NHS, National Health System.
Strategic goals and action lines (for the strategic map) in the Spanish Strategy on Cardiovascular Health (ESCAV)
| SG 1. | Improvement of health outcomes, equity and sustainability of the National Health System |
| AL 1.1. | Improvement of CV health outcomes and quality of life |
| AL 1.2. | Reinforcement of the efficiency and sustainability of the system |
| SG 2. | Greater autonomy and training of the agents involved |
| AL 2.1. | Raising awareness and education of the public in CV health |
| AL 2.2. | Involvement of CVD patients and their environment |
| AL 2.3. | Optimization of a multidisciplinary, comprehensive, and integrated approach to CV health care |
| SG 3. | Improvement of social and professional processes on healthy lifestyles and care for people with CVD |
| AL 3.1. | Promotion of healthy lifestyles and CV health prevention in society |
| AL 3.2. | Implementation of continuity of care and a multidisciplinary approach of comorbidities |
| AL 3.3. | Improvement of patient safety |
| AL 3.4. | Development of a gender perspective in CV health |
| AL 3.5. | Coordinated approach with other areas and agents |
| SG 4. | Availability of training, resources, research, innovation and knowledge management |
| AL 4.1. | Training and education of the professionals involved |
| AL 4.2. | Availability of resources and infrastructure for care |
| AL 4.3. | Promotion of research, development, and innovation |
| AL 4.4. | Suitability of information systems |
| AL 4.5. | Deployment of a homogeneous CV health information model |
AL, action line; CVD, cardiovascular disease; CV, cardiovascular; NHS, National Health System; SG, strategic goal.
Example of a strategic map of the Spanish Strategy on Cardiovascular Health of the National Health System. CV, cardiovascular; CVD, cardiovascular desease; HF, heart failure; IHD, ischemic heart disease; LA, line of action; NHS, National Health System; PREM, patient-reported experience measures; PROM, patient-reported outcome measures; R&D&i, research and development and innovation; SO, strategic objective; VHD, valvular heart disease.
To support the development of the ESCAV and the evaluation of interim and final outcomes, 61 indicators were proposed, each organized by action line and critical point. Among these, 16 indicators were considered as top priorities ().
DeploymentThe final version of the ESCAV was officially published on the Ministry of Health's website and presented at a formal meeting with representatives from the 17 ARCs. During this meeting, the representatives agreed on the general guidelines for implementation. As strategies do not have a specific allocated budget tied to a defined timeframe, flexible timelines were established to facilitate its execution.
Given the scope and complexity of the ESCAV, prioritization of strategic aims and actions was proposed by consensus among the working group coordinators and presented to the Institutional Committee. The first steps of the orderly deployment are presented in the results section.
RESULTSRolloutThe final version of the ESCAV was published on the Ministry of Health's website on 27 April 2022.14 No specific timeline was set for the rollout and full development, but a 5-year period is typically considered for the development of a national strategy, as each region retains the authority and competence to adapt and execute these actions according to their own priorities and resources. As a result, the pace of implementation varies across regions. The activation of the ESCAV was delayed due to competing priorities during and after the COVID-19 pandemic. The official presentation of the ESCAV took place on 29 March 2023.
Given the magnitude of the proposal, the involvement of different institutional and social levels, and its complementarity with other national strategies, a phased approach for implementation was approved. For 2024, the following lines were prioritized.
PreventionSpecific activities of the Ministry of Health's Promotion and Prevention Department have been aligned with the ESCAV proposals. These activities include: promoting physical activity to reduce sedentary lifestyles, encouraging healthy eating, and preventing alcohol consumption in health, educational, and regulatory environments,15 and the recently approved National Plan for Tobacco Prevention and Control 2024-2027.16
Promotion of interdisciplinary models of careThe following interdisciplinary models were proposed:
- -
National Plan on Out-of-Hospital Cardiac Resuscitation.
- -
Cardiogenic Shock Networks.
- -
Optimization of acute myocardial infarction networks to ensure comprehensive coverage of both ST-segment elevation myocardial infarctions (STEMIs) and non–ST-segment elevation myocardial infarctions (NSTEMIs).
Three specific actions focused on primary care were selected:
- -
Implementation of a check box in the EHR of primary care for cardiac auscultation for the early diagnosis of valvular heart disease and pulse taking for the early diagnosis of atrial fibrillation and earlier initiation of oral anticoagulation.
- -
Availability of natriuretic peptides in all primary care centers for the early diagnosis of heart failure.
A call for good practices related to the ESCAV was launched, inviting all autonomous communities to share ongoing local activities aligned with ESCAV recommendations. This initiative aimed to foster mutual learning and collaboration among regions.
Out of 30 submissions formally presented at the Ministry of Health in May 2024, 8 specific actions were selected, awarded, and subsequently published on the Ministry's website ().
DISCUSSIONCVD is the leading cause of death globally and a major contributor to morbidity, health care costs, and societal burden in all European countries.17,18 Despite its significant impact, CVD does not receive proportional priority in political planning or research funding. For instance, the European Union recently launched Europe's Beating Cancer Plan to address cancer prevention, treatment, and care, recognizing the growing challenges and opportunities in cancer care advancements.7 However, there is no equivalent European plan aimed at reducing the burden of CVD or enhancing cardiovascular health. This gap has been highlighted as an urgent priority by the European Society of Cardiology (ESC) in partnership with the European Alliance for Cardiovascular Health (EACH).19 To date, Spain appears to be the only country with a comprehensive plan to prevent and improve CVD care. A recent review of cardiovascular health plans in Europe identifies the Spanish Strategy as a leading example, alongside a funded CVD plan in Poland and initial efforts in Bulgaria (focused on a future CVD plan) and France (working on a White Paper).20 Given the major disparities in epidemiology, resources, care, and outcomes,21 there is an urgent need to invest in CVD prevention, care, and research at levels comparable to those dedicated to cancer prevention and care.22
After decades of positive epidemiological trends in CVD mortality, characterized by a steady decrease in CVD incidence and mortality, new societal changes are posing significant challenges to further progress. These include accelerated population aging, the growing prevalence of obesity5 and diabetes, social inequalities in cardiovascular risk factors, a rising number of patients living with chronic CVD due to better acute CVD care, and increasing rates of multimorbidity and dependence. Consequently, an increasing proportion of the population is living with disability and chronic CVD,23 resulting in a huge economic burden.24 This paradox stems from societal and health care advancements that have led to increased longevity and improved survival among individuals with CVD. As a result, there is a growing need for new actions to reduce the burden of CVD and enhance cardiovascular health across the population. These efforts must extend beyond the traditional focus on disease management and patient care to include a broader public health approach. Such an approach should address not only individuals with CVD but also the healthy population and the environmental factors that influence cardiovascular health.
Spain has released its first Cardiovascular Health Strategy, the most ambitious proposal ever developed to enhance the overall health of the Spanish population. This comprehensive strategy encompasses the promotion of cardiovascular health, primary prevention, early diagnosis, and the acute and chronic care of various cardiovascular syndromes (figure 1). Although Spain operates under a unified NHS, health care is delivered by 17 regional health care systems and 2 autonomous cities. This decentralized structure often results in regional differences that contribute to inequities in care. To address these disparities, the Spanish NHS Strategies were designed to promote equity and coherence in health care delivery across regions, aiming to minimize variations while allowing regional autonomy in planning, implementation, and service provision. The Ministry of Health has previously introduced several general strategies related to cardiovascular health in the NHS, including the Strategies on Diabetes,25 Stroke,26 Health Promotion and Prevention,27 Management of Chronicity,28 and the Strategy for Nutrition, Physical Activity and Obesity Prevention.29 These initiatives have served as a foundation for the Cardiovascular Health Strategy, which integrates and builds upon their principles.
Only one previous strategy had specifically focused on CVD: the Strategy on Ischemic Heart Disease, approved in 2006.30 Since then, no other dedicated strategy for CVD had been proposed. The new Cardiovascular Health Strategy represents a paradigm shift, moving from a focus on specific cardiovascular diseases to a broader emphasis on cardiovascular health. This expanded perspective includes the four most prevalent groups of CVDs and shifts attention beyond disease management to encompass the entire process of potential health loss. The strategy adopts a holistic approach, extending its scope from the health care system to society, from patients to citizens, and from health care professionals to all actors involved in health promotion and care.
This shift necessitates addressing the determinants of health, both individual and social, and implementing public health initiatives such as promoting sustainable living environments, population education campaigns, taxing unhealthy foods, and implementing measures to reduce tobacco and alcohol consumption. Additionally, the strategy emphasizes addressing factors contributing to worse health outcomes and inequities, such as socioeconomic conditions and access to education. While the central focus is on cardiovascular health, the strategy also identifies specific clinical areas requiring improvement, including: early diagnosis of heart failure and atrial fibrillation, optimization of regional networks for managing acute myocardial infarction,31 expansion to non–ST-segment elevation myocardial infarctions,32 cardiogenic shock,33 multidisciplinary management of chronic heart failure or aortic stenosis,34 increased cardiac rehabilitation and the development of a national plan for out-of hospital cardiac arrest.
The previous Strategy on Ischemic Heart Disease of Spain's NHS recommended the establishment of STEMI networks to achieve earlier and higher reperfusion rates in each Spanish region. The implementation of these networks progressed at varying speeds across regions, initially resulting in a regional disparity in STEMI mortality—higher in regions without established networks. However, this gap narrowed significantly after all regions implemented their respective STEMI networks.35 Other initiatives include the approval of the Spanish smoke-free law, regulations to reduce the availability of unhealthy foods in schools, and the more recent National Plan for Tobacco Prevention and Control 2024-2027. Given these precedents, it is reasonable to anticipate similarly positive outcomes from the new Cardiovascular Health Strategy. These results are expected to be particularly evident in terms of effectiveness and efficiency, especially when concrete actions with specific monitoring indicators are proposed.
Reducing regional inequalities is a fundamental objective of the ESCAV. Special emphasis has been placed on addressing gender inequities, as cardiovascular care has long been identified as a significant source of gender inequity in health care.36,37 Evidence of such inequities continues to be observed in Spain38,39 and other countries.40 Consequently, gender equity has been established as a cross-cutting theme throughout the ESCAV.
While the content of the strategy may apply to other countries or health care systems, the selection and prioritization of critical points, strategic aims, and actions need to be adapted to each context. The methods employed in the development of the strategy and the prioritization of its objectives may serve as a valuable resource for others seeking to create similar strategies or expand existing ones to address additional CVDs.
Although conceptually robust, implementing the ESCAV presents significant challenges. A wide range of indicators was selected to monitor its progress and assess the achievement of established objectives. However, the collection and measurement of these indicators remain far from routine practice and are often viewed as burdensome and complex. One major obstacle is the lack of automatic recording systems, which hinders efficient data collection. To address these challenges, improving registration and information systems is essential to enhance knowledge about cardiovascular health at the population level and CVD care within the health care system. This requires a framework to manage critical information: CVD care structures, processes, results, and quality indicators; standardizing data definitions; harmonizing data collection, integration, and sharing; considering all potential sources of information; and developing a systematic analysis plan for identifying needs and gaps while prioritizing improvement initiatives. These efforts are particularly critical given the ongoing transformations in data use regulations and artificial intelligence (AI) in Europe. Key regulatory frameworks, such as the General Data Protection Regulation (GDPR),41 European Data Space for Health (EEDS),42 and the proposed Artificial Intelligence Act (AIA),43 must be considered to ensure compliance and facilitate progress in cardiovascular health data management and analysis.
Despite potential skepticism regarding the ambition of the ESCAV to transform the national status of cardiovascular health—perceived by some as a naïve effort driven by voluntarism due to the lack of specific central funding—the success of the strategy will largely depend on its dissemination and the active involvement of key stakeholders. These include public institutions, scientific societies, and civil society. Encouragingly, early indicators of alignment with the ESCAV are evident in the growing number of activities and publications that reflect its principles and goals. Furthermore, the success of previous health strategies provides additional optimism, demonstrating the potential for meaningful impact through coordinated and sustained efforts.
CONCLUSIONSThe ESCAV represents one of the most ambitious initiatives ever undertaken to enhance cardiovascular health at the national level. The steps taken and the methodologies employed in the development of this strategy could serve as a reference for other countries and act as a catalyst for the creation of a comprehensive European plan for cardiovascular health.
FUNDINGAll expenses related to the development of ESCAV were covered by public funding from the Ministry of Health, Spain.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCEDuring the preparation of this work, generative artificial intelligence was used exclusively to improve English language. The output was supervised and approved by the corresponding author.
AUTHORS’ CONTRIBUTIONSH. Bueno, G. Seara, M. R. Azcutia, and M. J. Rodríguez-García were the scientific coordinators; S. Peláez and Y. Agra were the technical coordinators; and P. Aparicio Azcárraga was the technical leader during the drafting of the document of the ESCAV. C. A. Dueñas is the current technical coordinator of the rollout and development of the ESCAV and P. Gullón is the current technical leader of the rollout and development of the ESCAV. H. Bueno conceived the manuscript. H. Bueno and G. Seara drafted the manuscript, and all other authors critically reviewed its content contributing significantly to the final version.
CONFLICTS OF INTERESTNone of the authors have conflicts of interest directly related to this work. Outside of this work, H. Bueno receives research funding from the European Union (EU4H-2022-JA-03), Instituto de Salud Carlos III, Spain (FORTALECE program, PI21/01572), the Spanish Society of Cardiology, AstraZeneca, Boehringer Ingelheim, Janssen, and Novartis; and has previously received consulting and speaking fees from AstraZeneca, Novartis, Novo Nordisk and Organon. All other authors have nothing to declare.
The members of the ESCAV Multidisciplinary Advisory Committee are listed in appendix 1 of the supplementary data.