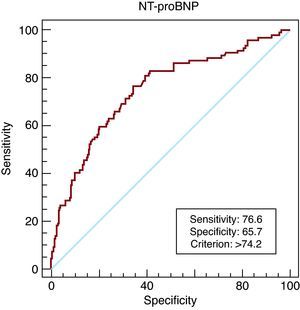
Electrocardiography (ECG) is the most widely used method for diagnosing left ventricular hypertrophy (LVH) in hypertensive patients. We assessed the value of N-terminal pro-brain natriuretic peptide (NT-proBNP) determination compared with ECG for detecting LVH in 336 consecutive hypertensive patients with preserved systolic function. We found a significant correlation between NT-proBNP levels and left ventricular mass adjusted for body surface area (r=.41; P<.001). The area under the receiver operating characteristic curve was 0.75 (95% CI, 0.7-0.8). A cut-off of 74.2 pg/mL had a greater sensitivity than ECG (76.6% vs 25.5%; P<.001) and a higher negative predictive value (87.8% vs 76.6%; P<.001) in the identification of LVH. NT-proBNP determination may be a useful tool for LVH screening in hypertensive patients.
Keywords
The presence of left ventricular hypertrophy (LVH) in patients with hypertension is an important predictor of cardiovascular events; hence, it is recommended to investigate LVH when evaluating the risk status of these patients.1 In clinical practice, electrocardiography (ECG) is the most commonly used procedure for this purpose, despite its low sensitivity. Echocardiography is a more accurate examination, but it requires more time, is more expensive, and is not always available because of technical reasons. The cost-benefit of routine echocardiographic study in the hypertensive population has been widely debated in the literature.2
In recent years, considerable interest has been focused on the relationship between plasma concentrations of B-type natriuretic peptide and N-terminal pro-brain natriuretic peptide (NT-proBNP) and the presence of structural heart disease.3 The use of plasma concentrations of this hormone for the diagnosis of LVH in the general population and in hypertensive patients has provided contradictory results due to the great heterogeneity of the patients analyzed.4, 5, 6, 7
The aim of this study is to compare the accuracy of plasma NT-proBNP concentrations with respect to ECG in screening for LVH in hypertensive patients, in order to better select patients who are candidates for echocardiographic examination.
METHODSWe consecutively analyzed all hypertensive patients older than 18 years referred to our hypertension unit between 2008 and 2010. A clinical history was taken in all patients, and all underwent a physical examination, ECG study, echocardiographic study with calculation of the left ventricular mass indexed by body surface area (LVMbs), and laboratory testing, including plasma NT-proBNP determination.
The echocardiographic diagnosis of LVH was based on the recommendations of the American and European echocardiography societies1, 8 (LVMbs ≥125 g/m2 in men and ≥110 g/m2 in women or interventricular septal thickness >13 mm in men and >12 mm in women), and the diagnosis by ECG was defined according to the classic criteria of Cornell and/or Sokolow-Lyon. Patients who presented atrial fibrillation, significant valve disease, or decreased left ventricular function (<50%) were excluded.
Statistical analysisQuantitative variables are described as the mean and standard deviation, and the Student t test was used for their comparisons. Categorical variables are expressed as the frequency and percentage, and comparisons were done with the chi-square test. The correlation analysis between the NT-proBNP value and the LVMbs was carried out with the Spearman test, since the variables did not follow a normal distribution. To determine the diagnostic reliability of NT-proBNP, the receiver operating characteristic (ROC) curve was calculated and the cut-off point that maximized sensitivity and specificity was selected. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the cut-off point and of ECG study in the diagnosis of LVH were determined. The validity indexes between the two tests were compared with the McNemar test for paired data. The statistical programs used were SPSS 17.0® and MedCalc 11.4®.
RESULTSIn total, 336 patients with hypertension and a mean age of 56.1 years were included. The clinical characteristics of the study population are shown in Table 1. Among the total, 28% (94 individuals) were found to have LVH on echocardiography. This group of patients had a slightly higher mean age, a greater number of established cardiovascular events in their clinical history, and a significantly higher NT-proBNP plasma concentration compared to patients without LVH (295.7 vs 92.9pg/mL; P<.001). Ambulatory blood pressure monitoring (ABPM) showed no differences in blood pressure values between the two populations. A significant correlation was observed between plasma NT-proBNP values and the LVMbs (r=0.41; P<.001). No correlation was found between NT-proBNP and the systolic or diastolic blood pressure values on ABPM.
Table 1. Clinical and Analytic Characteristics of the Populations Studied According to the Presence or Absence of Left Ventricular Hypertrophy.
| Total (n=336) | LVH (n=94) | No LVH (n=242) | P | |
| Age, years | 56.1 ± 13 | 59.9 ± 12.5 | 54.4 ± 13.1 | .001 |
| Women | 127 (37.8) | 31 (33) | 96 (39.7) | .256 |
| Diabetes mellitus | 66 (19.6) | 27 (28.7) | 39 (16.1) | <.01 |
| Smokers | 84 (25.1) | 24 (25.45) | 60 (24.8) | .568 |
| Ischemic heart disease | 17 (5.1) | 7 (7.4) | 10 (4.1) | .166 |
| Stroke | 17 (5.1) | 9 (9.6) | 8 (3.3) | .019 |
| BMI | 30.4 ± 5.1 | 31.2 ± 4.7 | 30.1 ± 5.2 | .09 |
| SBP at visit, mmHg | 153 ± 22 | 161 ± 25 | 151 ± 21 | .001 |
| DBP at visit, mmHg | 88 ± 13 | 87 ± 16 | 89 ± 12 | .318 |
| SBP 24-h mean (ABPM), mmHg | 130 ± 15 | 131 ± 17 | 130 ± 15 | .616 |
| DBP 24-h mean (ABPM), mmHg | 77 ± 11 | 78 ± 11 | 77 ± 11 | .275 |
| Fasting glucose, mg/dL | 113 ± 31 | 116 ± 30 | 112 ± 31 | .257 |
| LDLc, mg/dL | 123 ± 37 | 119 ± 34 | 124 ± 37 | .265 |
| Glomerular filtration, mL/min/1.73 m2 | 85 ± 21 | 79 ± 22 | 87 ± 21 | <.005 |
| Albumin/24 h, mg | 81 ± 306 | 167 ± 501 | 48 ± 172 | <.05 |
| LVH on ECG | 38 (11.2) | 24 (25.5) | 14 (5.8) | <.001 |
| NT-proBNP, pg/dL | 147 ± 258.6 | 295.7 ± 411.6 | 92.9 ± 126.7 | <.001 |
ABPM, ambulatory blood pressure monitoring; BMI, body mass index; DBP, diastolic blood pressure; ECG, electrocardiography; LDLc, low-density lipoprotein cholesterol; LVH, left ventricular hypertrophy; NT-proBNP, N-terminal pro-brain natriuretic peptide; SBP, systolic blood pressure.
Values are expressed as the n (%) or mean ± standard deviation.
Analysis of the usefulness of plasma NT-proBNP concentration in the diagnosis of LVH yielded an area under the ROC curve of 0.75 (95% confidence interval [CI] 0.7-0.8; P<.001) (Figure 1). A cut-off of 74.2 pg/mL had a sensitivity of 76.6%, specificity of 65.7%, PPV of 46.5%, and NPV of 87.8% for identifying LVH in our population. In contrast, ECG study yielded a significantly lower sensitivity and NPV, and only 25.5% of the patients who showed LVH on echocardiography were identified by this technique (Table 2). When the NT-proBNP cut-off was reduced to 20 pg/mL, sensitivity increased to 95.7% (95% CI, 89.5%-98.8%), with a specificity of 17.8% (95% CI 13.2%-23.2%), PPV of 31.1% (95% CI, 25.8%-36.8%), and NPV of 91.5% (95% CI, 79.4%-97.7%).
Figure 1. Receiver operating characteristic curve of plasma N-terminal pro-brain natriuretic peptide concentration for the diagnosis of left ventricular hypertrophy. NT-proBNP, N-terminal pro-brain natriuretic peptide.
Table 2. Indexes of Diagnostic Validity for Electrocardiography and N-Terminal pro-Brain Natriuretic Peptide in Left Ventricular Hypertrophy.
| Electrocardiography% (95% CI) | NT-proBNP (>74.2 pg/dL)% (95% CI) | P a | |
| Sensitivity | 25.5 (17.1-35.6) | 76.6 (66.7-84.7) | <.001 |
| Specificity | 94.2 (90.5-96.8) | 65.7 (59.4-71.1) | <.001 |
| PPV | 63.2 (46-78.2) | 46.5 (38.4-54.6) | <.001 |
| NPV | 76.5 (71.3-81.2) | 87.8 (82.2-92.2) | <.001 |
CI, confidence interval; NPV, negative predictive value; NT-proBNP, N-terminal pro-brain natriuretic peptide; PPV, positive predictive value.
a Comparative study using the McNemar test for paired data.
In this study, a direct association was found between plasma NT-proBNP concentration and the LVMbs in patients with hypertension and preserved systolic function. Moreover, the diagnostic accuracy of plasma NT-proBNP was greater than that of the ECG study, the most widely used method for initial assessment of these patients, as was evidenced by the higher sensitivity and negative predictive value of this marker.
Several studies have analyzed the capacity of natriuretic peptides for diagnosing LVH, but the results are contradictory.9, 10 Certain factors may have contributed to these discrepancies, such as heterogeneity of the populations included (even patients with heart failure), the type of natriuretic peptide analyzed, and the method used to confirm LVH. Studies performed in the general population have shown a close relationship between natriuretic peptide concentration and presence of systolic dysfunction, although the accuracy for identifying LVH is moderate.10 In the population with hypertension, NT-proBNP level has shown a greater association with the presence of LVH, particularly in women, in whom it has been proposed as an alternative to ECG study.11
Most studies, including ours, have evaluated the presence of LVH by echocardiography. The intraobserver variability of this technique could be one cause of the differences between studies. In this line, our group recently reported a significant correlation between NT-proBNP and the LVMbs calculated by magnetic resonance in patients with hypertension (r=0.598), with an area under the ROC curve for LVH detection of 0.87 (95% CI, 0.73-1.00; P<.05), results that open the possibility of diagnosing LVH by NT-proBNP determination.12
The main strength of our study is that it includes treated and relatively well-controlled patients. Because of these conditions, the study provides relevant results that are applicable to the management of hypertensive patients in clinical practice, where the need for rational use of existing resources is increasingly more evident. In this sense, plasma NT-proBNP determination can improve the diagnostic capability of ECG for identifying LVH in hypertensive patients without associated heart failure or atrial fibrillation. Furthermore, very low NT-proBNP values can be useful for planning imaging studies because they enable reasonable exclusion of LVH based on the chosen cut-off value. Additional studies are needed to analyze the economic implications of incorporating plasma NT-proBNP measurement in all patients with hypertension, and its impact on the medical care received.
CONFLICTS OF INTERESTNone declared.
Received 29 November 2010
Accepted 5 February 2011
Corresponding author: Servicio de Cardiología, Hospital Universitario de San Juan Ctra. Valencia-Alicante s/n, 03550 Sant Joan d’Alacant, Alicante, Spain. pedromorillas@teleline.es