ST-segment elevation myocardial infarction (STEMI) emergency care networks aim to increase reperfusion rates and reduce ischemic times. The influence of sex on prognosis is still being debated. Our objective was to analyze prognosis according to sex after a first STEMI.
MethodsThis multicenter cohort study enrolled first STEMI patients from 2010 to 2016 to determine the influence of sex after adjustment for revascularization delays, age, and comorbidities. End points were 30-day mortality, the 30-day composite of mortality, ventricular fibrillation, pulmonary edema, or cardiogenic shock, and 1-year all-cause mortality.
ResultsFrom 2010 to 2016, 14 690 patients were included; 24% were women. The median [interquartile range] time from electrocardiogram to artery opening decreased throughout the study period in both sexes (119 minutes [85-160] vs 109 minutes [80-153] in 2010, 102 minutes [81-133] vs 96 minutes [74-124] in 2016, both P=.001). The rates of primary PCI within 120 minutes increased in the same period (50.4% vs 57.9% and 67.1% vs 72.1%, respectively; both P=.001). After adjustment for confounders, female sex was not associated with 30-day complications (OR, 1.06; 95%CI, 0.91-1.22). However, female 30-day survivors had a lower adjusted 1-year mortality than their male counterparts (HR,0.76; 95%CI, 0.61-0.95).
ConclusionsCompared with men, women with a first STEMI had similar 30-day mortality and complication rates but significantly lower 1-year mortality after adjustment for age and severity.
Keywords
Although coronary heart disease (CHD) mortality has markedly fallen in Europe in the last 20 years, it is still the leading cause of death in most countries.1 Despite an increase in the number of incident ST-segment elevation myocardial infarction (STEMI) cases as the population ages, the number of STEMI patients in Europe has declined and stabilized.2,3
Data from the latest European registries show that men are at higher risk of incident STEMI at any age vs women but that STEMI incidence with age increases linearly in men but exponentially in women.4 Recent studies have shown that improvements in STEMI prognosis are due to both the implementation of a standard of care for reperfusion programs and the universalization of evidence-based medical treatments.5 STEMI networks increase reperfusion rates, reduce mortality, improve survival, and decrease the risk of recurrent ischemic events. Nationwide registries are essential to monitor STEMI treatments and outcomes, to evaluate the true effectiveness of treatments, and to account for changes in outcomes.3 Besides the exponential increase in STEMI in women, various studies have shown that women's prognosis after STEMI is worse than men's, not only because the condition affects women at older ages6 and those with clustering of risk factors,7 but also due to longer delays before medical help is sought,8,9 lower use of evidence-based treatments, and higher rates of kidney disease and bleeding.10
The aim of this study was to investigate the effect of sex on 30-day mortality and complications and on 1-year mortality in first STEMI patients during the first 7 years of implementation of the Codi IAM Emergency STEMI Care network (2010-2016) in Catalonia, Spain.
METHODSThe Codi IAM Catalan Emergency STEMI Care network was launched in 2010 in a region with 7.6 million inhabitants. The 3 main objectives of the network are to increase the rate of reperfusion therapy among STEMI patients, to achieve primary percutaneous coronary intervention (pPCI) in less than 120minutes from first contact with the health system,5 and to monitor the results of the program through a registry. The network was initially integrated into 5 hospitals with a 24-hour a day, 7-day a week pPCI facility and 5 daytime pPCI facilities. From 2015, the network spread across Catalonia, with 9 pPCI hospitals open 24hours a day, 7 days a week and 2 hospitals with daytime pPCI. The operational details of the Codi IAM have been published elsewhere.11 Briefly, the Emergency Medical Service organization coordinates the link between patients, ambulance transfers, and pPCI facilities according to the delay until treatment. Fibrinolysis is only considered if the pPCI transfer delay is unacceptable and there are no prior contraindications. Postfibrinolysis PCI (rescue PCI) is urgently performed in patients with no evidence of effective reperfusion. In those with effective fibrinolysis, PCI is performed after between 3 and 24hours, in line with ESC guidelines.5 STEMI was defined according to guidelines as acute myocardial infarction with ST-segment elevation ≥ 1mm in at least 2 contiguous leads (2mm in precordial leads) in the qualifying electrocardiogram (ECG).5
The Codi IAM registry was started in 2010 and includes demographic, clinical, care, therapeutic, and discharge data on patients with a STEMI onset ≤ 12hours. The Principal Investigator of the Codi IAM team of each participating hospital entered the data into an electronic case report form. Epicardial coronary flow in the STEMI culprit artery was graded according to the Thrombolysis in Myocardial Infarction (TIMI) flow grade,12 and reperfusion was considered optimal when TIMI 3 flow was obtained at the culprit lesion in less than 120minutes from first medical contact. Data collection was extended to new variables in 2012 (acute pulmonary edema, number of diseased vessels, and TIMI flow) and in 2015 (hypertension, dyslipidemia, smoking status, previous stroke, previous treatment, and type and number of stents). Bleeding was only included in the registry when the patient required transfusion.
The study included patients from the Codi IAM Registry who had been diagnosed with a STEMI from 2010 to 2016. Patients with cardiac arrest or death during first medical contact were also included if ST-segment elevation or a new left bundle branch block was diagnosed in any ECG during the initial care. All patients with known previous CHD (previous myocardial infarction or any revascularization) were excluded.
Patients’ mortality data were obtained from the Spanish mortality registry. The quality of the data included in the registry is periodically verified by external audits.
This project was approved by the ethics committee of Hospital del Mar (2020/9134) and all data are anonymous. Procedures and data collection were performed in accordance with the Declaration of Helsinki and Spanish Data Protection Laws.
End pointsThe primary assessment end points were all-cause mortality within 30 days and 1 year. In addition, the composite end point comprised 30-day complications, adjudicated as mortality during the first 30 days or ventricular fibrillation, pulmonary edema, or cardiogenic shock during the admission.
Statistical analysisDichotomous variables are shown as numbers and percentages, whereas continuous variables are shown as mean and standard deviation or, if nonnormally distributed, as median and interquartile range. Patient characteristics and treatment times were compared for each assessment end point: 30-day mortality or 30-day complications (cardiogenic shock, pulmonary edema, ventricular fibrillation, or death), and death of 30-day STEMI survivors within the first year after the intervention. Student t test or Mann-Whitney U test was used for continuous variables, whereas the chi-square or Fisher exact test was used for categorical variables. The association between sex and 30-day mortality or complications was evaluated with odds ratios (ORs) obtained by logistic regression models, and 1-year mortality in 30-day survivors was evaluated with hazard ratios (HRs) using Cox proportional hazards regression models. Models were adjusted for confounding variables associated with STEMI prognosis that had <8% missing values (ie, age, diabetes mellitus, recruitment year, time from symptom onset to culprit coronary artery opening, and Killip class). Symptom onset to artery opening and ECG to artery opening time variables had 7.6% missing data. The numbers of missing values for other variables were as follows: initial TIMI (31.1%), final TIMI (33.4%), no angiographical epicardial disease or 3-vessel disease (31.2%), left main disease (25.0%), bare-metal stent (83.7%), drug-eluting stent (82.3%), Killip class (1.5%), smoking (54.5%), hypertension (54.5%), dyslipidemia (54.5%), previous stroke (54.5%), and previous treatments (69.4%).
Survival curves were fit for both sexes and P values were obtained using the log-rank test.
An age-matched analysis (± 2 years) with 2 men for each woman was also performed. This subset of patients was used to confirm the effect of female sex in models adjusted for comorbidity (diabetes) and delay (time from symptom onset to artery opening) variables, as well as the year of registration and care center. Patients were assigned to the hospital in which they spent most of their hospital stay. One-year mortality was analyzed up to 2017 to obtain the 1-year mortality rates of patients from 2016.
Analyses were performed using R software version 3.6.0 (R Foundation for Statistical Computing, Austria). P <.05 was considered statistically significant.
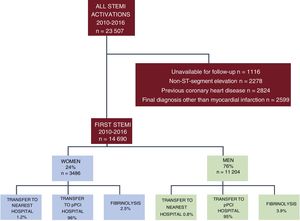
RESULTSFrom January 2010 to December 2016, 23 507 STEMI patients were included in the Codi IAM registry. The selection flowchart for the present study is shown in figure 1. The final cohort consisted of 14 690 patients (24% women) without previous CHD and with a discharge diagnosis of myocardial infarction and 1-year follow-up data.
The proportion of women was similar over the 7-year study period (P=.12).
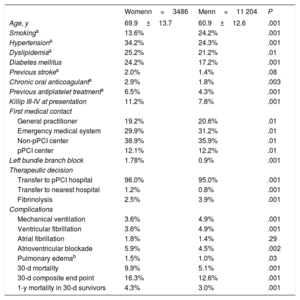
The baseline and complication characteristics of the cohort are shown in table 1. Women were older and had higher prevalence of diabetes mellitus, hypertension, and dyslipidemia and higher rates of heart failure. Women tended to be more frequently first attended in non-pPCI centers and less often cared for by the emergency ambulance system (P=.01). Women more frequently had left bundle branch block and had higher rates of heart failure and atrioventricular blockade (P <.01). Men had higher rates of ventricular fibrillation and need for mechanical ventilation.
Baseline patient and first medical contact characteristics by sex in the Codi IAM registry 2010-2016
| Womenn=3486 | Menn=11 204 | P | |
|---|---|---|---|
| Age, y | 69.9±13.7 | 60.9±12.6 | .001 |
| Smokinga | 13.6% | 24.2% | .001 |
| Hypertensiona | 34.2% | 24.3% | .001 |
| Dyslipidemiaa | 25.2% | 21.2% | .01 |
| Diabetes mellitus | 24.2% | 17.2% | .001 |
| Previous strokea | 2.0% | 1.4% | .08 |
| Chronic oral anticoagulanta | 2.9% | 1.8% | .003 |
| Previous antiplatelet treatmenta | 6.5% | 4.3% | .001 |
| Killip III-IV at presentation | 11.2% | 7.8% | .001 |
| First medical contact | |||
| General practitioner | 19.2% | 20.6% | .01 |
| Emergency medical system | 29.9% | 31.2% | .01 |
| Non-pPCI center | 38.9% | 35.9% | .01 |
| pPCI center | 12.1% | 12.2% | .01 |
| Left bundle branch block | 1.78% | 0.9% | .001 |
| Therapeutic decision | |||
| Transfer to pPCI hospital | 96.0% | 95.0% | .001 |
| Transfer to nearest hospital | 1.2% | 0.8% | .001 |
| Fibrinolysis | 2.5% | 3.9% | .001 |
| Complications | |||
| Mechanical ventilation | 3.6% | 4.9% | .001 |
| Ventricular fibrillation | 3.6% | 4.9% | .001 |
| Atrial fibrillation | 1.8% | 1.4% | .29 |
| Atrioventricular blockade | 5.9% | 4.5% | .002 |
| Pulmonary edemab | 1.5% | 1.0% | .03 |
| 30-d mortality | 9.9% | 5.1% | .001 |
| 30-d composite end point | 16.3% | 12.6% | .001 |
| 1-y mortality in 30-d survivors | 4.3% | 3.0% | .001 |
pPCI, primary percutaneous coronary intervention.
Data are expressed as % or mean±standard deviation.
Crude 30-day mortality, 30-day composite end point, and 1-year mortality rates were significantly lower in men than in women. Univariate analysis of factors associated with 30-day complications and 1-year mortality are shown in .
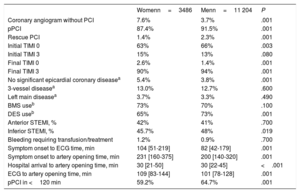
First medical contact and angiography and pPCI characteristics according to sex are shown in table 2. Time delays in STEMI care were longer in women than in men. Compared with men, women undergoing pPCI had significantly less initial TIMI 0 at the initial coronary angiography and less TIMI 3 at the final coronary angiography. Significant coronary disease (< 70% stenosis in epicardial vessels) was significantly less frequent in women; however, the coronary disease extension and severity (3-vessel disease or left main involvement) did not differ according to sex. Women waited a significant median of 22minutes longer for the first ECG than men and the time from ECG to reperfusion or to hospitalization was longer in women than in men.
Primary reperfusion procedure characteristics in men and women in the Codi IAM network from 2010 to 2016
| Womenn=3486 | Menn=11 204 | P | |
|---|---|---|---|
| Coronary angiogram without PCI | 7.6% | 3.7% | .001 |
| pPCI | 87.4% | 91.5% | .001 |
| Rescue PCI | 1.4% | 2.3% | .001 |
| Initial TIMI 0 | 63% | 66% | .003 |
| Initial TIMI 3 | 15% | 13% | .080 |
| Final TIMI 0 | 2.6% | 1.4% | .001 |
| Final TIMI 3 | 90% | 94% | .001 |
| No significant epicardial coronary diseasea | 5.4% | 3.8% | .001 |
| 3-vessel diseasea | 13.0% | 12.7% | .600 |
| Left main diseasea | 3.7% | 3.3% | .490 |
| BMS useb | 73% | 70% | .100 |
| DES useb | 65% | 73% | .001 |
| Anterior STEMI, % | 42% | 41% | .700 |
| Inferior STEMI, % | 45.7% | 48% | .019 |
| Bleeding requiring transfusion/treatment | 1.2% | 0.9% | .700 |
| Symptom onset to ECG time, min | 104 [51-219] | 82 [42-179] | .001 |
| Symptom onset to artery opening time, min | 231 [160-375] | 200 [140-320] | .001 |
| Hospital arrival to artery opening time, min | 30 [21-50] | 30 [22-45] | <.001 |
| ECG to artery opening time, min | 109 [83-144] | 101 [78-128] | .001 |
| pPCI in <120 min | 59.2% | 64.7% | .001 |
BMS, bare-metal stent; DES, drug-eluting stent; ECG, electrocardiogram; PCI, percutaneous coronary intervention; pPCI, primary percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; TIMI, Thrombolysis in Myocardial Infarction flow score.
Data are expressed as No. (%) or median [interquartile range].
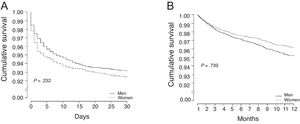
The trends in treatment delays, mortality, and the composite end point at 30 days are shown in table 3. Times from ECG to artery opening decreased during the study period for both sexes but the total ischemic time decreased only in men. At the end of the study period, a significantly lower proportion of women were reperfused in less than 120minutes than men (table 3). Survival curves at 30 days and 1 year are shown in figure 2: no significant differences were observed in these crude mortality curves between men and women.
Trends in delays to different levels of care and in end points over the 7-year period of the Codi IAM emergency care network for ST-elevation myocardial infarction patients
| Women | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | P for trend |
|---|---|---|---|---|---|---|---|---|
| SO to first medical contact | 94 [42-190] | 80 [40-168] | 90 [36-206] | 90 [42-212] | 90 [41.5-180] | 85 [40-195] | 73 [36-179] | .276 |
| First medical contact to ECG | 10 [5-20] | 8 [4-15] | 9 [4-20] | 8 [4-18] | 10 [5-20] | 9 [4-15] | 8 [3-15] | .029 |
| SO to hospital | 155 [89-268] | 130 [78-254] | 114 [67-214] | 150 [84-274] | 149 [80-288] | 135 [75-280] | 129 [78-270] | .012 |
| ECG to artery opening | 119 [85-160] | 113 [85-150] | 110 [83-147] | 110 [83-146] | 110 [84-146] | 104 [81-135] | 102 [81-133] | .001 |
| SO to artery opening | 250 [176-374] | 227 [159-375] | 245 [160-419] | 235 [163-376] | 248 [165-392] | 220 [152-354] | 203 [148-350] | .279 |
| pPCI in <120 min | 50.4% | 54.6% | 56.9% | 59% | 57.5% | 65.0% | 67.0% | <.001 |
| 30-d mortality | 9.7% | 8.3% | 10.8% | 10.7% | 9.5% | 10.2% | 9.7% | .906 |
| 30-d composite end point | 15.5% | 13.4% | 18.0% | 17.6% | 14.8% | 18.0% | 15.7% | .357 |
| 1-y mortality* | 4.2% | 4.0% | 4.0% | 4.7% | 4.9% | 4.6% | 3.6% | .952 |
| Men | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | P for trend |
|---|---|---|---|---|---|---|---|---|
| SO to first medical contact | 80 [35-170] | 67 [31-150] | 65 [29-150] | 69 [29-157] | 65 [29-150] | 63 [29-160] | 69 [33-160] | .009 |
| First medical contact to ECG | 8 [3-15] | 7 [3-15] | 7 [3-15] | 7 [4-15] | 7 [4-15] | 7 [4-15] | 7 [3-15] | .06 |
| SO to hospital | 125 [73-230] | 114 [54-219] | 114 [67-214] | 115 [64-226] | 115 [66-224] | 110 [64-227] | 118 [68-230] | .11 |
| ECG to artery opening | 109 [80-153] | 110 [83-150] | 105 [80-145] | 101 [76-134] | 102 [78-137] | 94 [74-125] | 96 [74-124] | .0001 |
| SO to artery opening | 224 [155-344] | 210 [149-330] | 204 [145-325] | 200 [140-326] | 197 [140-313] | 190 [134-305] | 190 [136-309] | .006 |
| pPCI in <120 min | 57.9% | 57.2% | 60.7% | 66.5% | 64.3% | 71.1% | 72.1% | <.001 |
| 30-d mortality | 5.2% | 4.4% | 4.8% | 4.7% | 5.4% | 5.9% | 5.3% | .539 |
| 30-d composite end point | 11.9% | 12.6% | 12.8% | 12.2% | 12.8% | 13.3% | 12.4% | .941 |
| 1-y mortality* | 2.5% | 3.2% | 2.7% | 3.6% | 3.2% | 3.3% | 3.0% | .668 |
ECG, electrocardiogram; pPCI, primary percutaneous intervention; SO, symptom onset.
Data are expressed as No. (%), mean±standard deviation, or median [interquartile range].
The effects of female sex on 30-day mortality and complications and 1-year mortality were tested with multivariate analyses with progressive adjustment for potential confounders: for the whole cohort in table 4A and for the male-female 2:1 age-matched subcohort in table 4B. Female STEMI patients had no increased risk of 30-day mortality or complications but had a significantly lower risk of 1-year mortality after adjustment for diabetes mellitus, year and center of recruitment, time from symptom onset to culprit coronary artery opening, age, and Killip class. Interestingly, the model not adjusted for age and Killip class showed an increased risk of 1-year mortality in women, indicating that age and STEMI severity are determinants of mortality in 30-day STEMI survivors (table 4A). The models fit to the age-matched cohort showed results of a similar magnitude and consistency to the findings for the full cohort but did not reach statistical significance due to lower statistical power.
Female STEMI patients in the Codi IAM network from 2010 to 2016 in the whole cohort (A) and in an age-matched subsample of 2 men:1 women (B): adjusted risks of 30-day mortality (models 1 and 2), the 30-day composite end point (mortality, ventricular fibrillation, acute pulmonary edema, or cardiogenic shock) (models 3 and 4), and 1-year mortality in 30-day survivors (models 5 and 6)
| A. 30-d mortality risk for female STEMI patients in the whole cohort | ||
|---|---|---|
| MODEL 1, n=13 468 | OR | 95%CI |
| Female sex | 1.90 | 1.63-2.23 |
| MODEL 2, n=13 468 | OR | 95%CI |
| Female sex | 1.06 | 0.92-1.33 |
| 30-d composite end point risk for female STEMI patients in the whole cohort | ||
|---|---|---|
| MODEL 3, n=14 690 | OR | 95%CI |
| Female sex | 1.29 | 1.15-1.45 |
| MODEL 4, n=14 690 | OR | 95%CI |
| Female sex | 1.05 | 0.91-1.21 |
| 1-y mortality risk for female 30-d STEMI survivors in the whole cohort | ||
|---|---|---|
| MODEL 5, n=13 770 | HR | 95%CI |
| Female sex | 1.57 | 1.28-1.93 |
| MODEL 6, n=13 770 | HR | 95%CI |
| Female sex | 0.78 | 0.63-0.97 |
| B. 30-d mortality risk for female STEMI patients paired by age with men | ||
|---|---|---|
| MODEL 1, n=8313 | OR | 95%CI |
| Female sex | 1.04 | 0.85-1.26 |
| MODEL 2, n=8313 | OR | 95%CI |
| Female sex | 0.98 | 0.79-1.22 |
| 30-d composite end point risk for female STEMI patients paired by age with men | ||
|---|---|---|
| MODEL 3, n=8313 | OR | 95%CI |
| Female sex | 1.00 | 0.87-1.15 |
| MODEL 4, n=8313 | OR | 95%CI |
| Female sex | 0.94 | 0.79-1.11 |
| 1-y mortality risk in 30-d female STEMI survivors paired by age with men | ||
|---|---|---|
| MODEL 5, n=7724 | HR | 95%CI |
| Female sex | 0.85 | 0.66-1.08 |
| MODEL 6, n=7724 | HR | 95%CI |
| Female sex | 0.84 | 0.65-1.08 |
95%CI, 95% confidence interval; HR, hazard ratio; OR, odds ratio; STEMI, ST-segment elevation myocardial infarction.
Models 1, 3, and 5 were adjusted for diabetes mellitus, recruitment year, center of recruitment, and time from symptom onset to culprit coronary artery opening. Models 2, 4, and 6 were adjusted as in models 1, 2, and 3 but with Killip class and age.
Our results show that women with a first STEMI are older, have more cardiovascular risk factors, and have longer delays vs men. In addition, although mortality and a composite of mortality and other complications (ventricular fibrillation, acute pulmonary edema, or cardiogenic shock) at 30 days are similar in men and women with a first STEMI, women have significantly lower mortality within 1 year.
Previous studies have evaluated the influence of female sex on STEMI prognosis. Female sex is generally considered to be a prognostic confounder due to its multiple divergent interactions with age and the related clinical profile and due to sex-related increases in treatment delays.8,9 However, the relationship between sex and outcomes after STEMI may also be due to global undercare or sex-based treatments: increased treatment delays and ischemic times,13 lower reperfusion rates, and underuse of evidence-based treatments during all STEMI phases.6 Optimal care is therefore a cornerstone of a favorable STEMI prognosis and of the utmost importance in female patients. In our cohort, women had longer treatment times than men. Delayed diagnoses are driven by sex-related pathophysiological differences such as an absence of typical male-related symptoms (chest pain) and less frequent ST-elevation on first ECG.14 In our cohort, female patients waited longer to ask for help (mean, 22minutes) and the ECG was performed with a longer delay than in men. The time between symptom onset and first medical contact accounted for 38% of the total ischemic time in women and for 34% of that in men. “Patient-related” delays are consistent across time periods and throughout literature and are challenging to reduce.15 Decreases in prehospital delays might have tremendous benefits on STEMI morbidity and mortality prognoses because many deaths occur in the very early phase from malignant arrhythmias16 and other acute-phase complications, which are known to be sex-specific, such as heart failure. Despite a general tendency for a decrease in pretreatment delays during the study period, women had a longer pretreatment delay than men. This may be partially because, compared with men, women more frequently first attended a non-pPCI center17 and also less frequently called emergency medical services, resulting in longer delays to STEMI revascularization treatment.18 Recent data from European registries showed that a decrease in delays could be influenced by media campaigns tailored not only to help women to identify the symptoms of CHD and thus rapidly access the health care system,19 but also to alert all health care providers participating in STEMI emergency care networks of the need to prevent possible gender gaps. In previous work, patients with prior myocardial infarction or prior revascularization had a shorter treatment delay, underlining the importance of knowledge or understanding of CHD pathophysiology to promote STEMI treatment.20
There is strong evidence that health care system delays are associated with mortality and heart failure-related readmission.21 However, despite the decrease in the ECG to artery opening time and the increase in the rate of pPCI in less than 120minutes during the study period, we observed no significant reduction in mortality in either sex in our cohort. The absence of a mortality decrease from 2010 to 2016 may be explained by the short study period and a slight increase in the mean age but warrants further and longer studies. Previous work from the same decade showed no further reduction in mortality, reinforcing the idea of a plateau in mortality after STEMI.3
In our cohort, sex did not have a significant effect on 30-day mortality or complications. Similar results were obtained in a subanalysis of age-matched male and female patients. The absence of a significant association remained after adjustment for time to treatment and year and hospital of treatment.
Women were about 9 years older than men in the STEMI cohort. The lack of an association of female sex with 30-day complications after age-matching of men and women is in contrast to some studies2,22 but in accordance with others.23–27 Several factors may explain this inconsistency. The first is that the vast majority of patients underwent coronary angiography catheterization during the acute phase (97.4% of women and 96.4% of men), reflecting the extensive implementation of systematic reperfusion, which reduced the “gender gap” observed several decades ago.26,28 It may also reflect the distinct nature of the underlying CHD affecting women: less angiographical evidence of significant epicardial disease than in men,29 with more plaque disruption or coronary dissection30 and CHD that affects smaller vessels with less ischemic burden.31 It may also reflect the incorporation of evidence-based therapies for both sexes in terms of primary prevention, baseline risk factors, and cardiovascular treatments after the first ischemic event.3,32 In our study, the 1-year crude mortality rate was higher in women than in men. This association was mostly accounted for by women's higher age and more comorbidities, as reflected by the regression analysis, which showed that women actually have better prognosis after 1 year than men after a first STEMI. The worse prognosis of men after STEMI has previously been reported and may reflect the higher cardiovascular risk burden and the higher risk of reinfarction25,33 at 1 year.
LimitationsSeveral important limitations should be considered. First, all data were derived from the first 7 years of a regional STEMI transportation network. Thus, some treatment and management variables are available for only a few years of the Codi IAM registry. For instance, the number of unavailable pulmonary edema events from 2010 to 2011 may represent as many as 60 events out of 1979 (3%). In addition, no records were available for medical treatment administered by the emergency medical system or at discharge. These treatments have a net beneficial impact on mortality both in-hospital and at 1 year of follow-up.3 In contrast, the network has a STEMI protocol for medications such as antithrombotic agents administered to all participants. Data regarding left ventricle ejection fraction was not available at the time of the study. The cause of death was also not available. Therefore, we cannot know the weight of cardiovascular diseases in the all-cause mortality. Optimal epicardial reperfusion was considered TIMI grade 3 at the end of the procedure but there were no details on ST resolution at ECG or TIMI myocardial blush grade to further evaluate reperfusion. In addition, and of note, the registry still has no records available on the menopausal status of women, which has a clear impact on the pathophysiology of cardiovascular diseases.34 Sex-related risk factors should be considered and recorded.
CONCLUSIONSIn the Codi IAM emergency STEMI transportation network, women underwent PCI with a greater delay than their male counterparts but showed similar 30-day mortality and complication rates and lower mortality 1 year after STEMI.
ACKNOWLEDGEMENTSWe thank Carme Carrel for data preparation and statistical management.
- –
Previous evidence showed that women with STEMI had worse prognosis than men.
- –
This gender gap has been partly explained by women's older age, more comorbidities, and lower receipt of evidence-based treatments.
- –
The implementation of the STEMI network Codi IAM has progressively reduced treatment delays.
- –
Despite worse risk profiles and longer delays in treatment, women showed similar 30-day cardiac complications vs men and lower 1-year all-cause mortality when age and comorbidities were considered.
This project received a research grant from Departament de Salut, Generalitat de Catalunya, in 2016.
CONFLICTS OF INTERESTNone declared.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.06.002