The impact of left ventricular ejection fraction (LVEF) on health care resource utilization (HCRU) and cost in heart failure (HF) patients is not well known. We aimed to compare outcomes, HCRUs and costs according to LVEF groups.
MethodsRetrospective, observational study of all patients with an emergency department (ED) visit or admission to a tertiary hospital in Spain 2018 with a primary HF diagnosis. We excluded patients with newly diagnosed heart failure. One-year clinical outcomes, costs and HCRUs were compared according to LVEF (reduced [HFrEF], mildly reduced [HFmrEF], and preserved [HFpEF]).
ResultsAmong 1287 patients with a primary diagnosis of HF in the ED, 365 (28.4%) were discharged to home (ED group), and 919 (71.4%) were hospitalized (hospital group [HG]). In total, 190 patients (14.7%) had HFrEF, 146 (11.4%) HFmrEF, and 951 (73.9%) HFpEF. The mean age was 80.1±10.7 years; 57.1% were female. The median [interquartile range] of costs per patient/y was €1889 [259-6269] in the ED group and €5008 [2747-9589] in the HG (P <.001). Hospitalization rates were higher in patients with HFrEF in the ED group. The median costs of HFrEF per patient/y were higher in patients in both groups: €4763 [2076-17 155] vs €3900 [590-8013] for HFmrEF vs €3812 [259-5486] for HFpEF in the ED group, and €6321 [3335-796] vs €6170 [3189-10484] vs €4636 [2609-8977], respectively, in the hospital group (all P <.001). This difference was driven by the more frequent admission to intensive care units, and greater use of diagnostic and therapeutic tests among HFrEF patients.
ConclusionsIn HF, LVEF significantly impacts costs and HCRU. Costs were higher in patients with HFrEF, especially those requiring hospitalization, than in those with HFpEF.
Keywords
Heart failure (HF) is a major global health problem with an increasing worldwide prevalence, currently situated between 1% and 3%.1,2 This trend is reflected in an increasing impact on patient care systems, with HF currently accounting for 3% to 8% of total health care spending in developed economies.3–5
HF is a heterogeneous spectrum of disorders whose defining characteristic is cardiac dysfunction.6 The 2021 clinical practice guidelines of the European Society of Cardiology distinguish 3 types of HF according to left ventricular ejection fraction (LVEF) status: HF with reduced ejection fraction (HFrEF), mildly reduced ejection fraction (HFmrEF), and preserved ejection fraction (HFpEF).7 Despite the epidemiological and pathophysiological differences between these types of HF, previous studies have not clearly defined the relationship between LVEF category and health care resource utilization (HCRU) and associated costs; moreover, the results of the few studies addressing this question are contradictory.8–12 The aim of the present study was to compare costs, HCRU, and prognosis in HF patients in the 3 LVEF categories during follow-up after cardiac decompensation requiring treatment in the emergency department (ED) or hospitalization.
METHODSThis retrospective cohort study included all patients aged ≥ 18 years with a primary diagnosis of HF and who required treatment in the ED or hospital admission at Hospital Universitario 12 de Octubre between January 1 and December 31, 2018. The following exclusion criteria were applied: a) unknown or unavailable LVEF data; b) new HF diagnosis; c) HF secondary to thyrotoxicosis, liver cirrhosis, end-stage renal failure, etc.13 To avoid inclusion of “extraordinary costs” due to associated cardiac comorbidities, we also excluded patients with correctable valvular heart disease, acute coronary syndrome, or ventricular assist devices, as well as heart and kidney transplant recipients.
Heart failure diagnosisHF diagnoses were obtained from either a) the ED database (International Classification of Primary Care, second edition, K77) or b) the Minimum Data Set for Admission and Emergency Care (International Classification of Diseases, 10th Revision, clinical codes I11.0*, I13.0*, I13.2*, and I50*).14,15 The 3 LVEF categories are defined as follows: HFrEF for LVEF ≤ 40%, HFpEF for LVEF ≥ 50%, and HFmrEF for LVEF between 41% and 49%.7
Events and health care resource utilizationInformation on events and HCRU was obtained from the hospital's patient management information system, which combines electronic health records and administrative data. Mortality and HCRU data for the year after ED or hospital discharge were obtained from the Community of Madrid Center for Basic Strategic Health Care Information (CIBELES), which records vital status of the population and all-cause mortality data. CIBELES forms part of the information system of the Madrid Regional Health Service (SERMAS).
The index discharge event was defined as the ED or hospital discharge prompting the inclusion of the patient in the analysis. An ED visit was defined as any medical attention in the ED. A hospital stay was defined as any time spent in a hospital unit lasting beyond midnight on the day of admission. Rehospitalizations included readmissions for any cause after the index hospitalization. Admissions subsequent to direct discharge to home from the ED were classed as first admissions, not readmissions. Outpatient visits were defined as any medical, nursing, rehabilitation, or day-hospital consultation. Follow-up time points were 30 days and 1 year after the index discharge.
For cost calculations and the representation of clinical results and HCRU, we used the COHERENT model.13,16 COHERENT is a graphical system for the visual display and comparison of composite endpoints. The system consists of a hierarchical code that defines a mutually exclusive list of potentially relevant clinical situations, including patient clinical status (alive or dead) and location (at home, in the ED, admitted to hospital, or in an outpatient consultation). COHERENT is linked to a cost calculator that computes resource utilization over the observation period for each patient and for the whole study population.16
Cost calculationCosts were calculated as described previously,16,17 using data provided by the Hospital Universitario 12 de Octubre accounts department. The cost of each event was calculated by summing the patient-level unit costs of each product or activity (eg, accommodation, hospital food service, drugs, devices), the unit costs of each product or activity included in the hospital service catalogue (eg, analysis, diagnostic and therapeutic interventions, surgery times, stays in the postoperative recovery unit), and residual costs not directly imputable to the patient or event. Residual costs were linked to the event cost by indirect imputation. The costing of the different patient care processes was based on the patient-level hospital-activity costs study initiative of the Spanish Hospital Costs Network (RECH), of which our hospital is a member.17
Statistical analysisCategorical variables are presented as absolute frequency (No.) and relative frequency (%), whereas continuous variables are presented as mean±standard deviation or as median [interquartile range]. For continuous variables, differences were compared by the Student t and Mann-Whitney U tests, analysis of variance, or the Kruskal-Wallis test. For categorical variables, differences were compared by the chi-square or Fisher exact test. Costs are presented as absolute spending in euros and as the percentage of the total cost as a function of follow-up time, patient care unit, and clinical event, and as the median cost per patient and day. Multiple logistic regression models were used to identify variables that predict higher cost in the total cohort and in the 3 LVEF groups. Statistical calculations were performed in R version 4.0.3 (The R Foundation for Statistical Computing, Austria). Differences were considered statistically significant at P <.05.
The study complied with the Declaration of Helsinki and was approved by the local ethics committee.
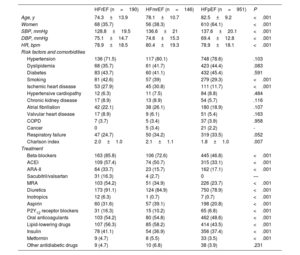
RESULTSPatientsBetween January 1 and December 31, 2018, 93 962 medical visits made by 66 551 patients were recorded. A primary diagnosis of HF was recorded in 1378 patients, with LVEF records available for 1174 (85.2%). Of these patients, 3 (0.3%) died in the ED, 365 (31.1%) were discharged, and 806 (68.7%) were admitted. An additional 127 patients without a primary diagnosis of HF in the ED had had received the diagnosis at the time of discharge after hospitalization, and LVEF records were available for 113 (90.0%) of these patients (figure 1 and ). The study cohort thus included 1287 patients, of whom 190 (14.7%) had HFrEF, 146 (11.4%) HFmrEF, and 654 (71.2%) HFpEF. Baseline patient characteristics are shown in table 1. The patients with HFpEF were on average older, and a higher proportion of them were women. The HFpEF patient group also had less ischemic heart disease and a higher prescription rate of prognosis-improving drugs and diuretics. There were no between-group differences in the distribution of hypertension, diabetes, atrial fibrillation, or other comorbidities.
Central illustration. Of 1287 patients with a primary diagnosis of HF included over a 1-year period, 365 were discharged directly from the ED, 919 were discharged after hospitalization, and 3 died. HFrEF patients discharged from the ED had a higher rate of hospital admission during the follow-up period. In the total cohort, HFrEF patients incurred higher costs whether they were discharged directly from the ED or after hospitalization. HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFmrEF, heart failure with mildly reduced ejection fraction; HFrEF, heart failure with reduced ejection fraction. gr1.
Baseline characteristics of patients with heart failure stratified by left ventricular ejection fraction category
| HFrEF (n=190) | HFmrEF (n=146) | HFpEF (n=951) | P | |
|---|---|---|---|---|
| Age, y | 74.3±13.9 | 78.1±10.7 | 82.5±9.2 | <.001 |
| Women | 68 (35.7) | 56 (38.3) | 610 (64.1) | <.001 |
| SBP, mmHg | 128.8±19.5 | 136.6±21 | 137.6±20.1 | <.001 |
| DBP, mmHg | 75.1±14.7 | 74.6±15.3 | 69.4±12.8 | <.001 |
| HR, bpm | 78.9±18.5 | 80.4±19.3 | 78.9±18.1 | <.001 |
| Risk factors and comorbidities | ||||
| Hypertension | 136 (71.5) | 117 (80.1) | 748 (78.6) | .103 |
| Dyslipidemia | 68 (35.7) | 61 (41.7) | 423 (44.4) | .083 |
| Diabetes | 83 (43.7) | 60 (41.1) | 432 (45.4) | .591 |
| Smoking | 81 (42.6) | 57 (39) | 279 (29.3) | <.001 |
| Ischemic heart disease | 53 (27.9) | 45 (30.8) | 111 (11.7) | <.001 |
| Hypertensive cardiopathy | 12 (6.3) | 11 (7.5) | 84 (8.8) | .484 |
| Chronic kidney disease | 17 (8.9) | 13 (8.9) | 54 (5.7) | .116 |
| Atrial fibrillation | 42 (22.1) | 38 (26.1) | 180 (18.9) | .107 |
| Valvular heart disease | 17 (8.9) | 9 (6.1) | 51 (5.4) | .163 |
| COPD | 7 (3.7) | 5 (3.4) | 37 (3.9) | .958 |
| Cancer | 0 | 5 (3.4) | 21 (2.2) | - |
| Respiratory failure | 47 (24.7) | 50 (34.2) | 319 (33.5) | .052 |
| Charlson index | 2.0±1.0 | 2.1±1.1 | 1.8±1.0 | .007 |
| Treatment | ||||
| Beta-blockers | 163 (85.8) | 106 (72.6) | 445 (46.8) | <.001 |
| ACEI | 109 (57.4) | 74 (50.7) | 315 (33.1) | <.001 |
| ARA-II | 64 (33.7) | 23 (15.7) | 162 (17.1) | <.001 |
| Sacubitril/valsartan | 31 (16.3) | 4 (2.7) | 0 | — |
| MRA | 103 (54.2) | 51 (34.9) | 226 (23.7) | <.001 |
| Diuretics | 173 (91.1) | 124 (84.9) | 750 (78.9) | <.001 |
| Inotropics | 12 (6.3) | 1 (0.7) | 7 (0.7) | <.001 |
| Aspirin | 60 (31.6) | 57 (39.1) | 198 (20.8) | <.001 |
| P2Y12 receptor blockers | 31 (16.3) | 15 (10.2) | 65 (6.8) | <.001 |
| Oral anticoagulants | 103 (54.2) | 80 (54.8) | 462 (48.6) | <.001 |
| Lipid-lowering drugs | 107 (56.3) | 85 (58.2) | 414 (43.5) | <.001 |
| Insulin | 78 (41.1) | 54 (36.9) | 356 (37.4) | <.001 |
| Metformin | 9 (4.7) | 8 (5.5) | 33 (3.5) | <.001 |
| Other antidiabetic drugs | 9 (4.7) | 10 (6.8) | 38 (3.9) | .231 |
ACEI, angiotensin converting enzyme inhibitors; ARA-II, angiotensin II receptor antagonists; COPD, chronic obstructive pulmonary disease; DBP, diastolic blood pressure; HFmrEF, heart failure with mildly reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; HR, heart rate; MRA, mineralocorticoid receptor antagonist; SBP, systolic blood pressure.
Data are presented as No. (%) for discrete variables and as mean ± standard deviation for continuous variables.
Of the 919 hospitalized patients, 157 (17.1%) had HFrEF, 108 (11.8%) had HFmrEF, and 654 (71.2%) had HFpEF. Baseline characteristics in LVEF each group were similar to those of the full cohort (). The HFrEF group had a higher rate of admission to the cardiology unit than the HFmrEF or HFpEFgroups (77 [49.1%], 39 [36.1%], and 89 [13.6%], respectively; P <.001) but had a low rate of admission to the internal medicine unit (72 [45.8%], 69 [63.9%], and 555 [84.9%]; P <.001). There were no between-group differences in the length of stay in the index hospitalization (median 7 [5-10], 7 [5-10], and 7 [4-10] days; P=.35).
The baseline characteristics of patients discharged from the ED (n=365) were similar to those of the hospitalized group (). The mean length of stay in the ED was 0.7±0.7 days, with no differences between LVEF groups.
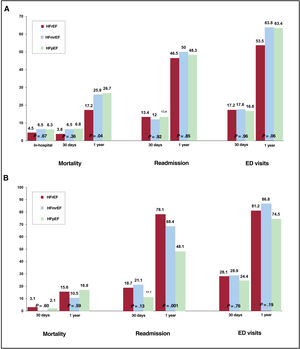
Clinical results and resource utilization stratified by LVEF groupAmong the hospitalized patients, in-hospital and 30-day mortality rates were similar for the 3 LVEF groups, but 1-year mortality was significantly lower in hospitalized HFrEF patients than in their HFmrEF and HFpEF counterparts (17.2, 25.9, and 26.7%; P <.001) (figure 2). However, LVEF was not an independent predictor after adjusting for age, sex, and cardiovascular risk factors (P=.58).
Clincal results stratified by LVEF category. A) Clinical results of hospitalized patients at 30-days and 1-year of follow-up, stratified by left ventricular ejection fraction. B) Clinical results of patients discharged from the emergency department at 30-days and 1-year follow-up, stratified by left ventricular ejection fraction. ED, emergency department; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFmrEF, heart failure with mildly reduced ejection fraction; HFrEF, heart failure with reduced ejection fraction. gr2.
No between-group differences in hospital readmissions were observed at 30-day and 1-year follow-up. Hospital-discharged patients with HFpEF spent a higher proportion of the observation year at home than their counterparts in the other LVEF groups (figure 3). Hospital-discharged patients with HFrEF attended more outpatient consultations, whereas visits to the ED were more frequent among HFmrEF and HFpEF patients.
Clinical results, health care resource utilization, and costs (COHERENT) for hospitalized patients. A) 30-day follow-up. B) 1-year follow-up. Hospital indicates first admission during follow-up; ED indicates first treatment in the emergency department. HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFmrEF, heart failure with mildly reduced ejection fraction; HFrEF, heart failure with reduced ejection fraction. gr3.
Among patients in the ED group, the 30-day mortality rates for patients with HFrEF, HFmrEF, and HFpEF were 3.1%, 0.0%, and 2.1% (P=.60), and the 1-year rates were 15.6%, 10.5%, and 16.9% (P=.59). There were no between-group differences in the number of repeat ED visits at 30 days and 1 year.
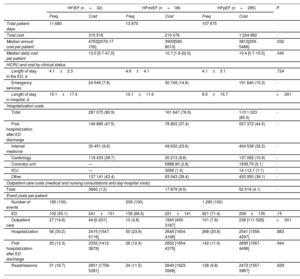
HFrEF and HFmrEF patients in the ED group had higher 30-day and 1-year hospitalization rates than their counterparts in the hospital-discharged group (HFrEF, 8.0% vs 13.4% at 30 days and 75.0% vs 46.5% at 1 year; HFmrEF, 21.1% vs 12.0% at 30 days and 68.4% vs 50% at 1 year; P <.05). Moreover, ED-discharged patients with HFrEF were hospitalized for a higher proportion of the follow-up period (10 [4-19] days) than those with HFmrEF (6 [0-16] days) or HFpEF (0 [0-11]; P <.001). ED-discharged patients had higher rates of new ED treatment at the 30-day and 1-year follow-ups, independently of LVEF category. Among ED-discharged patients, HFrEF patients had more outpatient visits (11 [3-21]) vs 11.5 [5-18] for HFmrEF and 7 [3-12] for HFpEF; P=.009) (table 3 and ).
Costs stratified by patient trajectory, clinical status, and events during 1-year follow-up of patients discharged from the emergency department
| HFrEF (n=32) | HFmrEF (n=38) | HFpEF (n=295) | P | ||||
|---|---|---|---|---|---|---|---|
| Freq. | Cost | Freq. | Cost | Freq. | Cost | ||
| Total patient-days | 11 680 | 13 870 | 107 675 | - | |||
| Total cost | 315 516 | 210 476 | 1 254 982 | - | |||
| Median annual cost per patient | 4763[2076-17 155] | 3900[590-8013] | 3812[259-5486] | .032 | |||
| Median daily cost per patient | 13.0 [5.7-47.0] | 10.7 [1.6-22.0] | 10.4 [0.7-15.0] | .040 | |||
| HCRU and cost by clinical status | |||||||
| Length of stay in the ED, d | 4.1±2.3 | 4.6±4.1 | 4.1±3.1 | .724 | |||
| Emergency services | 24 549 (7.8) | 30 749 (14.6) | 191 640 (15.3) | - | |||
| Length of stay in hospital, d | 15.1±17.4 | 10.1±11.6 | 8.5±15.7 | <.001 | |||
| Hospitalization costs | |||||||
| Total | 287 075 (90.9) | 161 847 (76.9) | 1 011 323 (80.5) | - | |||
| First hospitalization after ED discharge | 149 885 (47.5) | 78 803 (37.4) | 557 372 (44.5) | - | |||
| Internal medicine | 30 451 (9.6) | 49 632 (23.6) | 404 538 (32.2) | - | |||
| Cardiology | 119 433 (39.7) | 20 213 (9.6) | 137 082 (10.9) | - | |||
| Coronary unit | — | 5888.90 (2.8) | 1639.70 (0.1) | - | |||
| ICU | — | 3068 (1.4) | 14 112.1 (1.1) | - | |||
| Other | 137 141 (43.4) | 83 043 (39.4) | 453 950 (36.1) | - | |||
| Outpatient care costs (medical and nursing consultations and day-hospital visits) | |||||||
| Total | 3940 (1.2) | 17 879 (8.5) | 52 018 (4.1) | - | |||
| Event costs per patient | |||||||
| Number of events | 185 (100) | 209 (100) | 1 290 (100) | ||||
| ED | 102 (55.1) | 241±151 | 139 (66.5) | 221±141 | 921 (71.4) | 208±135 | .15 |
| Outpatient care | 27 (14.6) | 44 [0-231] | 10 (4.8) | 1840 [455-3187] | 101 (7.8) | 238 [111-526] | <.001 |
| Hospitalization | 56 (30.2) | 2415 [1547-5116] | 50 (23.9) | 2649 [1654-4168] | 268 (20.8) | 2541 [1556-4297] | .883 |
| First hospitalization after ED discharge | 25 (13.3) | 2332 [1412-3879] | 26 (12.4) | 2652 [1654-4375] | 142 (11.0) | 2695 [1567-4496] | .944 |
| Readmissions | 31 (16.7) | 2651 [1759-5281] | 24 (11.5) | 2649 [1623-3568] | 126 (9.8) | 2472 [1557-3967] | .629 |
ED, emergency department; Freq., frequency; HFmrEF, heart failure with mildly reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; ICU, intensive care unit.
Costs are expressed in euros as the quantity (% of the total) or as the median [interquartile range].
Whether discharged from the ED or after an index hospitalization, patients with HFrEF were more frequently hospitalized for a cardiovascular cause during follow-up, whereas patients with HFpEF were hospitalized mostly for noncardiovascular causes ().
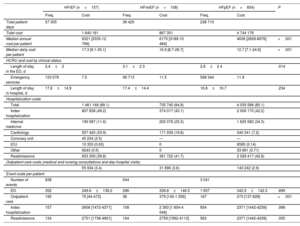
Costs by LVEF groupThe median annual cost per patient was €5008 [€2747-€9590] for patients discharged after hospitalization and €3889 [€2590-€6269] for patients discharged from the ED (P <.001). For hospital-discharged patients, the total cost was highest for the HFpEF group (€4 474 176), reflecting its size, followed by the HFrEF group (€1 640 162) and the HFmrEF group (€867 351). Nevertheless, HFrEF was associated with a higher median annual cost per patient (€6321 [€3335-€12 796]), compared with €6170 [€3189-€10 484] for the HFmrEF group and €4636 [€2609-€8977] for the HFpEF group (P <.001). The median daily cost per patient was considerably higher for patients with HFrEF (€17.3 [€9.1-€35.1] vs €16.9 [€8.7-€28.7] for HFmrEF and €12.7 [€7.1-€24.6] for HFpEF; P <.001) (table 2).
Costs stratified by patient trajectory, clinical status, and events during 1-year follow-up of initially hospitalized patients
| HFrEF (n=157) | HFmrEF (n=108) | HFpEF (n=654) | P | ||||
|---|---|---|---|---|---|---|---|
| Freq. | Cost | Freq. | Cost | Freq. | Cost | ||
| Total patient-days | 57 305 | 39 420 | 238 710 | ||||
| Total cost | 1 640 161 | 867 351 | 4 744 176 | ||||
| Median annual cost per patient | 6321 [3335-12 796] | 6170 [3189-10 484] | 4636 [2609-8976] | <.001 | |||
| Median daily cost per patient | 17.3 [9.1-35.1] | 16.9 [8.7-28.7] | 12.7 [7.1-24.6] | <.001 | |||
| HCRU and cost by clinical status | |||||||
| Length of stay in the ED, d | 2,4±2 | 3.1±2 3 | 2.8±2 4 | .014 | |||
| Emergency services | 123 078 | 7.5 | 99 713 | 11.5 | 568 344 | 11.9 | |
| Length of stay in hospital, d | 17,8±14,9 | 17.4±14.4 | 16.8±16.7 | .234 | |||
| Hospitalization costs | |||||||
| Total | 1 461 148 (89.1) | 735 740 (84.8) | 4 035 588 (85.1) | ||||
| Index hospitalization | 807 838 (49.2) | 374 017 (43.1) | 2 006 170 (42.2) | ||||
| Internal medicine | 190 587 (11.6) | 202 078 (23.3) | 1 625 582 (34.3) | ||||
| Cardiology | 557 420 (33.9) | 171 939 (19.8) | 340 341 (7.2) | ||||
| Coronary unit | 40 234 (2.5) | — | — | ||||
| ICU | 10 353 (0.63) | 0 | 6585 (0.14) | ||||
| Other | 9243 (0.5) | 0 | 33 661 (0.71) | ||||
| Readmissions | 653 309 (39.8) | 361 722 (41.7) | 2 029 417 (42.8) | ||||
| Outpatient care costs (medical and nursing consultations and day-hospital visits) | |||||||
| 55 934 (3.4) | 31 896 (3.6) | 140 242 (2.9) | |||||
| Event costs per patient | |||||||
| Number of events | 838 | 544 | 3 041 | ||||
| ED | 352 | 349.6±138.2 | 296 | 336.8±146.5 | 1 657 | 342.9±142.3 | .899 |
| Outpatient care | 195 | 75 [44-472] | 36 | 379 [145-1 256] | 167 | 273 [137-628] | <.001 |
| Index hospitalization | 157 | 2606 [1472-4371] | 108 | 2 393 [1 604-4 549] | 654 | 2371 [1442-4239] | .088 |
| Readmissions | 134 | 2751 [1736-4901] | 104 | 2759 [1562-4113] | 563 | 2371 [1442-4239] | .055 |
ED, emergency department; Freq., frequency; HFmrEF, heart failure with mildly reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; ICU, intensive care unit.
Costs are expressed in euros as the quantity (% of the total) or as the median [interquartile range].
Costs at the 30-day and 1-year follow-up were lower for patients discharged to home from the ED; the total cost for these patients at 1 year was €1 780 974, with 81.9% of this cost (€1 460 194) attributable to hospitalizations (193 first hospitalizations and 181 readmissions) and 13.9% attributable to 1161 ED visits, with no differences between LVEF groups (table 3). The highest costs for patients discharged from the ED were incurred by those with HFrEF, with a median annual cost per patient of €4763 [€2076-€17 155] and a median daily cost per patient of €13.0 [€5.70-€47.00]; the equivalent costs for patients with HFmrEF were €3900 [590-8.013] and €10.70 [€1.60-€22.00] and for those with HFpEF the costs were €3812 [€259-€5486] and €10.40 [€0.70-€15.00] (all comparisons P <.05).
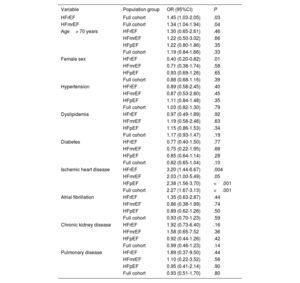
To identify predictors of higher total cost at 1-year of follow-up in the full cohort (relative to the median for our population), we conducted a multivariate analysis including LVEF group, age> 70 years, sex, diabetes, dyslipidemia, hypertension, ischemic heart disease, atrial fibrillation, chronic kidney disease, and pulmonary disease. In this analysis, HFrEF, HFmrEF, and ischemic heart disease were associated with higher cost. Female sex was associated with lower cost in the HFrEF group but not in the HFmrEF or HFpEF groups. As in the full cohort, ischemic heart disease was associated with higher cost in all the LVEF groups (table 4). The multivariate analysis was repeated to differentiate between HF with LVEF <50% and LVEF ≥ 50% ().
Multivariate analysis of the association of clinical factors with higher cost at 1-year of follow-up in the full cohort and stratified by LVEF (HFpEF, HFmrEF, and HFrEF)
| Variable | Population group | OR (95%CI) | P |
|---|---|---|---|
| HFrEF | Full cohort | 1.45 (1.03-2.05) | .03 |
| HFmrEF | Full cohort | 1.34 (1.04-1.94) | .04 |
| Age> 70 years | HFrEF | 1.30 (0.65-2.61) | .46 |
| HFmrEF | 1.22 (0.50-3.02) | .66 | |
| HFpEF | 1.22 (0.80-1.86) | .35 | |
| Full cohort | 1.19 (0.84-1.66) | .33 | |
| Female sex | HFrEF | 0.40 (0.20-0.82) | .01 |
| HFmrEF | 0.71 (0.38-1.74) | .58 | |
| HFpEF | 0.93 (0.69-1.26) | .65 | |
| Full cohort | 0.88 (0.68-1.16) | .39 | |
| Hypertension | HFrEF | 0.89 (0.58-2.45) | .40 |
| HFmrEF | 0.87 (0.53-2.80) | .45 | |
| HFpEF | 1.11 (0.84-1.48) | .35 | |
| Full cohort | 1.03 (0.82-1.30) | .79 | |
| Dyslipidemia | HFrEF | 0.97 (0.49-1.89) | .92 |
| HFmrEF | 1.19 (0.58-2.48) | .63 | |
| HFpEF | 1.15 (0.86-1.53) | .34 | |
| Full cohort | 1.17 (0.93-1.47) | .19 | |
| Diabetes | HFrEF | 0.77 (0.40-1.50) | .77 |
| HFmrEF | 0.75 (0.22-1.95) | .68 | |
| HFpEF | 0.85 (0.64-1.14) | .28 | |
| Full cohort | 0.82 (0.65-1.04) | .10 | |
| Ischemic heart disease | HFrEF | 3.20 (1.44-6.67) | .004 |
| HFmrEF | 2.03 (1.00-5.49) | .05 | |
| HFpEF | 2.38 (1.56-3.70) | <.001 | |
| Full cohort | 2.27 (1.67-3.13) | <.001 | |
| Atrial fibrillation | HFrEF | 1.35 (0.63-2.87) | .44 |
| HFmrEF | 0.86 (0.38-1.99) | .74 | |
| HFpEF | 0.89 (0.62-1.26) | .50 | |
| Full cohort | 0.93 (0.70-1.23) | .59 | |
| Chronic kidney disease | HFrEF | 1.92 (0.73-6.40) | .16 |
| HFmrEF | 1.58 (0.65-7.52 | .36 | |
| HFpEF | 0.92 (0.44-1.26) | .42 | |
| Full cohort | 0.99 (0.46-1.23) | .14 | |
| Pulmonary disease | HFrEF | 1.89 (0.37-9.50) | .44 |
| HFmrEF | 1.10 (0.22-3.52) | .56 | |
| HFpEF | 0.95 (0.41-2.14) | .90 | |
| Full cohort | 0.93 (0.51-1.70) | .80 |
95%CI, 95% confidence interval; HFmrEF, heart failure with mildly reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; LVEF, left ventricular ejection fraction; OR, odds ratio.
Increased cost was defined as a cost exceeding the median for the population group: €4248 for the full cohort (1287 patients), €5759 for the HFrEF group (190 patients), €5319 for the HFmrEF group (146 patients), and €4115 for the HFpEF group (951 patients).
Our study of a contemporary cohort of patients with acute HF shows that the treatment of patients with reduced LVEF is costlier for the health system. This elevated cost is mostly related to higher hospitalization costs: patients with reduced LVEF were more frequently admitted to critical care units, had longer hospital stays, and incurred higher costs related to diagnostic and therapeutic procedures ().
The effect of LVEF on the cost of HF care has been investigated in a small number of studies, most of them from the USA. In the 1990s, Liao et al.8 studied a cohort of 495 patients and found no cost differences at 5-years of follow-up between patients with LVEF ≤ 40% and those with LVEF> 40%. In a more contemporary US cohort with lifetime follow-up data, HFpEF (LVEF> 50%) was associated with a 24% higher total cost compared with HFrEF.18 However, in another cohort, of 564 patients, hospitalization costs were 16% higher for patients with HFrEF (LVEF ≤ 40%) than for those with LVEF> 40%, although this difference was not statistically significant.11 The discrepancies between these study outcomes can be explained by differences in the inclusion and exclusion criteria (chronic vs incident HF, stable vs decompensated HF), the inclusion period, the type of health care evaluated, and the scope of the cost analysis. The most complete study to date is that by Lam et al.,19 which examined data from more than 100 000 patients with chronic HF over an average follow-up of 18 months. That study revealed a monthly cost per patient of $9290, with a higher cost for patients with HFrEF (LVEF ≤ 40%) ($11 053) than for HF patients with LVEF> 40% ($7482).
In the Spanish context, the present study is one of the first to analyze the impact of LVEF on health care costs in a large cohort of patients with chronic HF, and also includes the HFmrEF category. HFmrEF has an intermediate cost, higher than HFpEF and closer to that of HFrEF. Our findings are in line with those of a contemporary Spanish study that found a lower overall cost during the follow-up of a population of mostly stable patients receiving outpatient care.20 The higher HCRU for the HFrEF group in our study can be attributed to several factors: a) HFrEF patients were more likely to be admitted to the cardiology unit, where they had longer hospital stays and underwent more diagnostic tests and received more specific treatments (note that the study did not include patients experiencing a first decompensation event, so the cost difference cannot be attributed to the compendium of techniques used for an initial HF diagnosis); b) these patients required more outpatient consultations, reflecting closer follow-up of this group; c) these patients were more frequently admitted to the critical care unit.
Given the diversity of study designs and the differences between health systems, it is important to obtain national and local data. In Spain, other epidemiological studies that included outpatients with HF reported lower costs at 1-year of follow-up.12,21 This result highlights the need to focus prevention strategies on patients who have been hospitalized and have a reduced LVEF, as these patients are at the highest risk and also account for the highest proportion of spending.
The results of our cost-distribution analysis are in line with the available evidence, which attributes the largest proportion of costs (40%-49%) to hospitalizations.5,22–24 Promoting outpatient stability thus has a dual benefit: improved prognosis and reduced health care spending.
In the multivariate analysis, an association with higher cost was found not only for reduced LVEF, but also for ischemic heart disease. This reflects these patients’ higher rate of interventional treatment and admission to specialist units, independently of LVEF. The multivariate analysis also showed an association between female sex and lower cost in the HFrEF group, but not in the HFpEF group, suggesting that women with HFrEF may be receiving a less-than-proportionate share of health care resources.
Although the readmission rate in our cohort was similar to that reported in other studies (approximately 50% at 1 year),25,26 it is notable that the highest rate of hospitalization during follow-up, almost 80%, was for HFrEF patients released directly from the ED. This finding suggests that LVEF is an index of hospital admission risk that could be used to improve the sometimes inadequate risk assessment of HF patients in the ED, and it is worth considering strategies to improve the care and follow-up of these patients.27,28
The proportion of patients with HFrEF in our sample is lower than that reported in a previous large population study.29 This discrepancy is likely related to several features of our study population. First, our cohort had an older age profile. Second, our study analyzed patients with chronic HF, and many of those classed as having HFmrEF or HFpEF were likely in recovery from HFrEF treated with prognosis-improving drugs, since our analysis only considered the LVEF derived from the most recently available echocardiogram at the time of inclusion. Finally, a transthoracic echocardiogram was available for most of the patients in our cohort, and the LVEF profile is thus likely to reflect the awareness at our center of the diagnostic value of echocardiography in patients with HF.
LimitationsOur findings may not be applicable in other settings due to differences in patient care between centers and health care systems, for example in the rate of discharge to home from the ED, length of stay, and readmissions. Moreover, it may not be possible to extrapolate the absolute costs to other health care funding systems. In our view, highlighting the differences between health care funding models provides an opportunity to identify areas for improvement. Although the Minimum Data Set data has inherent limitations, comparison with medical records has validated the use of administrative data as a tool for estimating health service outcomes. However, the level of precision achieved with this approach for studies based on the primary diagnosis is unlikely to be achievable for secondary diagnoses; this is likely to result in an underestimation of comorbidities, which may explain the absence of expected between-group differences in our analysis.
CONCLUSIONSLVEF has a significant impact on HCRU in patients with chronic HF. Patients with HFrEF incur higher costs during follow-up and are more frequently hospitalized after discharge from the ED. For all the LVEF groups, more than 80% of spending was associated with hospitalization. To limit HCRU and spending, health care systems should therefore prioritize strategies to maintain outpatient stability.
FUNDINGThis study is an initiative of investigators funded through an award from AstraZeneca Farmacéutica España. The funders played no role in the collection or analysis of data, but did contribute to the interpretation of the results.
AUTHOR CONTRIBUTIONSAll the authors contributed to the study design and to the writing of this manuscript and approved the final version. H. Bueno an J.L. Bernal are joint lead authors.
CONFLICTS OF INTERESTJ.C. López-Azor holds a research contract from the Instituto de Salud Carlos III (CIBERCV 1705/2076). Héctor Bueno conducts research funded by the Instituto de Salud Carlos III, the Spanish Society of Cardiology, PhaseBio, and Novartis and receives consultancy fees from AstraZeneca and Novartis.
- –
HF is a major health problem that accounts for up to 7% of health care spending in developed economies.
- –
Since the publication of the 2021 European Society of Cardiology clinical practice guidelines, HF has been classified into 3 groups: HFpEF, HFmrEF, and HFrEF.
- –
Despite the well-known pathophysiological differences between these 3 HF categories, the impact of LVEF on HCRU and the costs associated with chronic HF are unknown.
- –
LVEF influences HCRU and costs during the follow-up of patients with chronic HF. Patients with HFrEF and HFmrEF require more resources than those with HFpEF, despite having a similar prognosis.
- –
The difference in cost is mainly due to HFrEF patients’ higher rate of admission to the critical care unit and their need for more diagnostic tests and therapeutic interventions.
- –
More than 80% of health care costs for HF patients are associated with hospitalization.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2023.06.003