Primary mitral regurgitation (MR) is the most frequent valve dysfunction in developed countries and mitral prolapse is the most common etiology. Although percutaneous therapy has emerged as an option for the treatment of MR in selected cases,1 surgical repair is the gold-standard treatment and most of these valves are repairable in expert centers.2,3 Driven by the excellent results of surgical repair, a trend toward earlier intervention has emerged, provided a successful and durable result is likely. However, 50% of patients currently undergoing surgery in Europe and North America still receive a prosthetic replacement instead.4
Our objective was to describe our early and mid-term results of the surgical repair of mitral prolapse. We conducted a retrospective review of all patients who underwent surgery due to severe MR secondary to valve prolapse from November-2011 to December-2018, excluding all concomitant procedures other than atrial fibrillation ablation. All patients had a comprehensive transthoracic echocardiogram shortly before the intervention and before discharge, and intraoperative transesophageal echocardiography was performed in all cases. All patients underwent at least 1 year of annual clinical and echocardiographic follow-up.
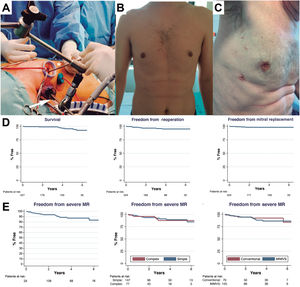
During the study period, 1456 patients underwent a mitral intervention and 229 met the inclusion criteria (table 1). Of these, 147 patients underwent a minimally-invasive mitral valve surgery (MIMVS) (64%) and 82 a median sternotomy (36%) (figure 1). MIMVS was performed almost entirely by 1 surgeon (93%). Complex morphologies (isolated anterior, commissural or bileaflet prolapse) were present in more than one third of patients. Concomitant atrial fibrillation ablation was performed in 30 patients (13%).
Patient characteristics and perioperative results
| Total (n=229) | MIMVS (n=147) | Conventional (n=82) | P | |
|---|---|---|---|---|
| Preoperative data | ||||
| Age, y | 61 ±12 | 60 ±12 | 63±12 | .04 |
| Male sex, % | 157 (69) | 100 (68) | 57 (70) | .87 |
| Weight, kg | 73±14 | 73±14 | 74±13 | .42 |
| Height, cm | 169±10 | 170±10 | 168±9 | .29 |
| Creatinine, mg/dL | 0.95±0.32 | 0.93±0.31 | 1.00±0.34 | .11 |
| Smoking, % | 64 (28) | 39 (27) | 25 (30) | .56 |
| Ischemic heart disease, % | 11 (5) | 4 (3) | 7 (9) | .06 |
| Hypertension, % | 97 (43) | 61 (42) | 36 (44) | .79 |
| Dyslipidemia, % | 65 (29) | 40 (28) | 25 (31) | .60 |
| Diabetes, % | 16 (7) | 10 (7) | 6 (7) | 1.00 |
| Prior stroke, % | 10 (4) | 5 (3) | 5 (6) | .34 |
| AF, % | 63 (28) | 36 (25) | 27 (33) | .17 |
| COPD, % | 17 (8) | 8 (6) | 9 (11) | .13 |
| NYHA, % | <.01 | |||
| I-II | 150 (66) | 106 (72) | 44 (54) | |
| III-IV | 79 (34) | 41(28) | 38 (46) | |
| Left ventricular ejection fraction, % | 61±7 | 61±7 | 60±8 | .47 |
| End-diastolic diameter, mm | 57±7 | 56±7 | 58±6 | .12 |
| End-systolic diameter, mm | 35±6 | 35±6 | 36±5 | .19 |
| Prolapse location, % | .34 | |||
| Posterior | 149 (65) | 98 (67) | 51 (62) | |
| Anterior | 20 (9) | 14 (10) | 7 (9) | |
| Bileaflet | 58 (25) | 34 (23) | 24 (29) | |
| Previous cardiac operation, % | 7 (3) | 2 (1) | 5 (6) | .10 |
| EuroSCORE II | 1.95±2.34 | 1.57±1.37 | 2.64±3.36 | <.01 |
| Perioperative results | ||||
| Prosthetic mitral replacement, % | 5 (2) | 2 (1.4) | 3 (4) | .35 |
| In-hospital mortality, % | 2 (0.9) | 1 (0.7) | 1 (1.2) | 1 |
| Intensive care unit stay, d | 1 [1-1] | 1 [1-1] | 1 [1-2] | <.01 |
| Hospital stay, d | 7 [6-11] | 7 [6-10] | 8 [7-11] | .03 |
| RBC units transfused | 0 [0-0] | 0 [0-0] | 0 [0-1] | .19 |
| Hemoglobin on day 5, mg/dL | 11±2 | 11±2 | 10±2 | <.01 |
| Mechanical ventilation duration, h | 3 [0-7] | 0 [0-6] | 6 [3-10] | <.01 |
| De novo postoperative AF, % | 68 (30) | 39 (27) | 29 (36) | .14 |
| Permanent pacemaker, % | 7 (3) | 4 (3) | 3 (4) | .70 |
| Permanent stroke, % | 3 (1) | 2 (1) | 1 (1) | .66 |
| Hemodialysis or CRRT | 2 (1) | 1(1) | 1 (1) | 1 |
| Tamponade, % | 4 (2) | 1(1) | 3 (4) | .13 |
| Echocardiographic MR at discharge, % | n=224* | n=145* | n=79* | .28 |
| No MR | 183 (81.7) | 118 (81.4) | 65 (82.3) | |
| Mild (and trace) | 38 (17.0) | 26 (17.9) | 12 (15.2) | |
| Moderate | 3 (1.3) | 1 (0.7) | 2 (2.5) | |
| Severe | 0 | 0 | 0 | |
AF, atrial fibrillation; AKI, acute kidney insufficiency; COPD, chronic obstructive pulmonary disease; CRRT, continuous renal replacement therapy; MIMVS, minimally-invasive mitral valve surgery; MR, mitral regurgitation; NYHA, New York Heart Association; RBC, red blood cells.
Values are expressed as No. (%), mean±standard deviation, or median [interquartile range].
Transareolar MIMVS picture. Arrow demonstrates the videocamera used, asterisk shows the long-shafted instruments (A). Cosmetic result after MIMVS using a minithoracotomy (B) or periareolar approach (C). Follow-up data showing survival, freedom from reoperation and from mitral replacement (D). Echocardiographic follow-up showing: overall freedom from recurrent moderate-or-severe regurgitation, the same for simple and complex forms and after Conventional or MIMVS repair (E). MIMVS, minimally-invasive mitral valve surgery; MR, mitral regurgitation.
Successful mitral repair was achieved in 224 patients (97.8%) and the incidence of adverse events was low (table 1). Median intensive care unit and hospital stay were 1 and 7 days, respectively. Five patients underwent reoperation before hospital discharge due to increased MR compared with the intraoperative assessment. In all patients, we performed a successful immediate re-repair during the same admission. A total of 99% of the patients repaired were discharged from the hospital with mild-or-less MR.
Clinical follow-up (median: 4; maximum: 8.3 years) showed that at 1-, 3- and 5-year survival was 99%, 99% and 95%, freedom from reoperation was 98%, 97%, and 95% and, finally, freedom from mitral replacement was 99%, 98%, and 98%, respectively. Echocardiographic follow-up (median: 3 years; maximum: 8.3 years) showed a freedom from recurrent MR (moderate-or-more) after 1, 3 and 5 years of 96%, 90%, and 89%, respectively. During follow-up, 10 patients underwent reoperation (range: 1 month to 7 years), in all cases for recurrent severe MR (due to disease progression in 60%). In 6 of these patients (60%), the mitral valve was re-repaired successfully. There were no reoperations for mitral stenosis or endocarditis and there were no differences in follow-up duration between groups.
Our data show that surgical repair of MR due to leaflet prolapse can be safely accomplished in most patients in a referral center. In contrast to most published series, which analyze patients undergoing repair excluding patients selected for other treatments, our cohort was defined by the valve dysfunction regardless of the procedure planned or performed.
Regarding the approach, thoracoscopic MIMVS was performed in 64% of patients, with increasing frequency over time. MIMVS provided excellent results, with decreased length of hospital stay (7 vs 8 days; P <.01), intensive care unit stay (1 vs 1 day; P <.01) and mechanical ventilation (median 0 vs 6h; P <.001), although the procedure required longer cardiopulmonary bypass (+30min; P <.01) and aortic cross-clamp duration (+19min; P <.01). Blood loss was reduced after MIMVS, as shown by the higher hemoglobin level after surgery (11 vs 10mg/dL; P <.01). MIMVS had no negative impact on repair quality, despite being offered to all types of patients regardless of repair complexity. Mid-term outcomes were similar with both approaches and freedom from valve replacement at 5 years was higher after MIMVS (100% vs 95%; P <.01). The main limitation of this study comparing the 2 approaches is the risk of selection bias due to its retrospective nature. To account for this, we performed a propensity score matching (79 matched-pairs), which confirmed that all these differences, with the exception of total hospital stay, remained significant (data not shown).
Since we are currently recommending early surgery to younger, asymptomatic patients, there is growing demand to achieve excellent long-lasting results, with the lowest possible risk and surgical aggression. As shown in this study, equivalent or even superior results can be obtained with MIMVS in expert centers.5 This highlights the importance of publishing institutional results of surgical repair, making this key information available to cardiologists and patients to help them make the best decisions about options and timing of intervention.6
Mitral repair of severe MR due to leaflet prolapse can be accomplished with very good results (97.8% repair rate and 0.87% mortality). MIMVS can be offered to most patients without compromising outcomes and providing a faster recovery. Results up to 8 years after the procedure suggest excellent durability, regardless of the approach. Extended follow-up is required to establish long-term results.