To the Editor,
A 62-year-old woman with dyspnea at rest and chest pain persisting for 2 months was referred to our hospital with a presumptive diagnosis of pulmonary thromboembolism (PTE). On admission the physical examination revealed signs of right-sided heart failure and systolic murmur in the pulmonary area. The electrocardiogram showed signs of overload of the right chambers, whereas transesophageal echocardiography showed dilatation of the pulmonary trunk, a heterogeneous hypoechoic image straddling the bifurcation, and a right ventricle with severe dilatation and deterioration of the systolic function. A ventilation-perfusion scintigraphy suggested a high probability of PTE and, therefore, anticoagulant therapy with sodium heparin was initiated. Venous Doppler ultrasound of the lower limbs ruled out the presence of thrombosis. The differential diagnosis included a tumor of the pulmonary artery.
Computed tomography angiography of the chest showed an occlusive endoluminal filling defect that involved the pulmonary trunk, extending toward both main branches but primarily affecting the left: some sectors of the image were late-phase contrast-enhanced (Figure 1A). The lesion was confirmed by pulmonary angiography (Figure 1B), and found to produce a critical obstruction with a translesional pressure gradient of 53 mmHg. Atypical, vimentin-positive Ki67 cells were observed in specimens taken with a bioptome. The anatomical pathology diagnosis was angiosarcoma of the pulmonary trunk.
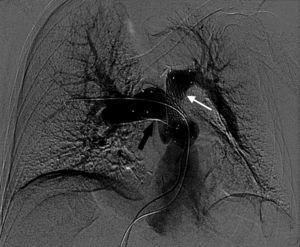
Figure 1. A: tomography angiography of the chest; endoluminal mass affecting the trunk (white arrow) and invading the right branch of the pulmonary artery (yellow arrow); its relationship with the aorta can also be seen (blue arrow). B: pulmonary angiography confirming the previous finding: absence of filling with iodinated contrast material.
Given the infiltration of the pulmonary artery and adjacent cardiac structures and the patient's poor overall condition and high surgical risk, it was considered that the tumor could not be surgically resected. To relieve the dyspnea, palliative treatment consisting of angioplasty of the pulmonary trunk with 2 stents of 26/40 mm and 24/60 mm was successfully undertaken (Figure 2).
Figure 2. Digital subtraction angiography: stents placed in the right (black arrow) and left (white arrow) branches of the pulmonary artery.
Following the procedure, the patient's symptoms improved. She was discharged with functional class II dyspnea and was able to return to her normal activities. After 4 months, she presented progressive dyspnea up to functional class III, caused by severe stent obstruction due to tumor growth. Repeat angioplasty was not technically feasible. Following considerable discussion by the medical team and in accordance with the patient's wishes, surgical reduction of the tumor mass was undertaken as the last therapeutic option to relieve the progressive symptoms. The patient died 3 days later, due to multiple postoperative complications.
Primary angiosarcomas of the pulmonary artery are rare, and only a few cases have been described. The similarity of acute and chronic PTE at onset and the inability of imaging techniques to yield an accurate diagnosis (although they may be useful in the differential diagnosis) lead to delays in the definitive diagnosis, which can only be obtained by tissue sampling or autopsy (60% of cases).1 Percutaneous endomyocardial biopsy is a safe, easily performed procedure with low morbidity and mortality. To enhance the diagnostic benefit, the biopsy can be taken under fluoroscopic guidance, as in the case described, or under transesophageal echocardiographic guidance.2
Angiosarcoma presents in middle age (40-65years) and tends to affect only one of the pulmonary branches, unlike PTE which tends to affect both. The tumor grows rapidly and produces local invasion and distant metastasis. Vascular occlusion is the main cause of death. The prognosis is poor: the mean survival is 1.5 months if surgical resection is not possible and about 12 months if the patient undergoes surgery, which is usually partial.3
Angioplasty of the pulmonary trunk is a minimally invasive, palliative procedure that has only been reported in a few cases.4 The procedure could be useful to improve symptoms due to obstruction and can be combined with chemotherapy or radiotherapy to reduce the tumor size and improve the quality of life in patients excluded from surgical treatment.
Corresponding author: mlgarate@ffavaloro.org