To the Editor,
We report the case of a 59-year-old male smoker with hypertension and dyslipidemia who, in 2007, was diagnosed with atrial fibrillation and patent foramen ovale (PFO) after suffering a cerebral ischemic attack in the region of the middle cerebral artery. The high risk of a further cerebral ischemic attack (score of 3 on the CHADS 2) was an indication for long-term oral anticoagulation. However, as it was difficult to achieve adequate levels of anticoagulation and to avoid further anticoagulation therapy, percutaneous closure of the left atrial appendage (LAA) using an Amplatzer cardiac plug (ACP) and of the PFO using an Amplatzer septal occluder (ASO) was proposed. The patient agreed to this approach.
Two- and 3-dimensional transesophageal echocardiography (2D and 3D TEE) showed the LAA anatomy to be favorable to closure and indicated the presence of PFO at the level of the fossa ovalis.
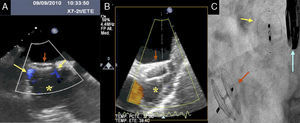
Following usual practice in the catheterization laboratory, LAA closure was carried out under fluoroscopic guidance; 2D and 3D TEE were also used. These techniques were used to control passage into the left atrium through the PFO and to measure the longitudinal diameters of the base and the middle third (20, 18 and 16mm, respectively, in left and right anterior oblique projection using fluoroscopy, and 22mm, 18mm and 17mm using 2D TEE at orientations of 0° and 116°). A 20-mm ACP device mounted on the corresponding delivery system was used for closure. The device was released after verifying that it was correctly positioned using angiography and 2D and 3D TEE. Control angiography was then used to check the device's stability and to determine that there was no contrast flow to the LAA; TEE was used to check that there was minimal flow penetration into the LAA at the edges of the device (Figure 1).
Figure 1. A: image obtained using 2-dimensional transesophageal echocardiography and showing minimum residual flow (arrows) between the edges of the device and the cavity of the appendage (asterisk). B: 2-dimensional transesophageal echocardiography image shows Amplatzer plug (arrow) released and occluding the entrance to the left atrial appendage (asterisk). C: fluoroscopic image showing the Amplatzer septal occluder device implanted at the level of foramen ovale (red arrow) and the Amplatzer cardiac plug device implanted in the left atrial appendage (yellow arrow). Blue arrow: transesophageal echocardiography probe.
Using the same delivery system, a 25-mm cribriform ASO device was implanted and its stability and efficacy confirmed in the same way. Again, no passage of contrast or color on the Doppler image was observed for the PFO closure device (Figure 2).
Figure 2. A: image obtained using 3-dimensional transesophageal echocardiography and showing the position of the device used to close the patent foramen ovale in the atrial septum, and the Amplatzer cardiac plug occluding the left atrial appendage. B: 3-dimensional transesophageal echocardiography image of the device (Amplatzer septal occluder) used to close the patent foramen ovale in the atrial septum. ASO, Amplatzer septal occluder; IAS, interatrial septum; LAA, left atrial appendage; MV, mitral valve.
The patient was discharged without complications the following day on dual antiplatelet therapy (aspirin and clopidogrel).
Percutaneous closure of the LAA is offered as a new treatment option for patients at risk of embolism in whom it may be difficult to achieve satisfactory anticoagulation control or where anticoagulation treatment is not possible or desirable.1 Ninety percent of thrombi in patients with nonrheumatic atrial fibrillation occur in the LAA.2 A PFO closure is also possible and is recommended in situations where there is a risk of paradoxical embolism,3 regardless of recent discussions and reports on its long-term usefulness.
This case shows that it is possible to carry out the double percutaneous procedure in the same intervention and to thereby act directly on the embolic focus of the LAA while also closing the PFO.
Corresponding author. calmeria.hcsc@salud.madrid.org