Despite some evidence suggesting microvascular dysfunction involvement, the pathophysiology of tako-tsubo cardiomyopathy (TTC) remains unclear. Recently, a new method has been validated to quantify volumetric coronary absolute flow (AF) and myocardial resistance (MR), based on the principle of thermodilution, using continuous saline infusion.1 We sought to evaluate the safety and feasibility of this new method in the setting of TTC.
Between May 2017 and January 2019, 8 consecutive patients diagnosed with TTC and admitted for chest pain in the 2 participating centers were prospectively included in our study. Informed consent was obtained in all patients. After coronary angiography and left ventricular angiography showing highly suggestive contractility alterations, a comprehensive invasive physiological assessment of the microcirculation in the left anterior descending coronary artery was systematically obtained in each patient by using a pressure-temperature sensor-equipped wire, as previously reported.2 The index of microvascular resistance (IMR) and coronary flow reserve were obtained by administering intravenous adenosine to induce hyperemia and then three 3-mL injections of room-temperature saline were given. The technique for AF and MR measurement requires continuous saline infusion through a specific catheter positioned in the proximal coronary artery (Figure 1).1,3 The procedure was repeated 2 weeks later in 2 patients, taking care that the same wire position was used at the second examination.
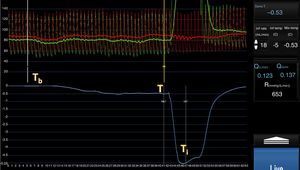
Example measurement of absolute flow (AF). Room temperature saline solution is infused into the coronary artery at a preset rate (10-20mL/min) through a specific catheter. The screen displays a real-time readout of the baseline temperature (Tb) and, after the infusion begins, there is a gradual decrease in temperature (T). Once the temperature stabilizes, the guidewire is positioned at the microcatheter tip to measure the infusion temperature (Ti). This allows quantitative measurement of AF according to the formula Qb=1.08 Ti/T Qi, where Qi is the preset saline infusion rate. Aortic pressure (red trace) and distal coronary pressure (green trace) are monitored simultaneously; this allows estimation of MR with the formula R=Pd/Qb, where Pd is the distal intracoronary pressure and Qb is the AF.
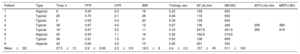
In all patients, left ventricular ejection fraction (LVEF) recovery after the acute phase was confirmed by cardiac magnetic resonance (6/8 patients, 75%), angiography (2/8 patients, 25%), or echocardiography (8/8, 100%). Seven patients were female (87.5%) and the mean age was 75±7 years. A typical apical ventricular morphology was identified in the ventriculogram in 5 patients (62.5%) and the rest were atypical morphologies. Mean left ventricular ejection was 43±6% and mean peak troponin T was 594±465 ng/mL. Coronary angiography revealed no nonsignificant epicardial coronary lesions in any of the patients; interestingly, 1 patient had angiographically moderate diffuse disease showing a grey-zone fractional flow reserve value (0.76); optical coherence tomography evaluation confirmed diffuse disease and a stable fibrocalcified plaque with a minimum luminal area of 4.1 mm2. The average time needed to complete all the physiological measurements was 19±3minutes. There were no significant adverse events. The median time from symptom onset to coronary measurements was 32 (IQR: 11-41) hours. Most patients had normal or borderline IMR index values. However, coronary flow reserve was reduced in all but 2 patients; in these patients, normal coronary flow reserve and IMR index values were obtained 38 and 42hours after the acute phase, highlighting the time-related recovery of microvascular dysfunction in TTC2 (Table 1).
Data on microvascular function in TTC patients
| Patient | Type | Time, h | FFR | CFR | IMR | Tmnhyp, sec | AF,mL/min | MR,WU | AFFU,mL/min | MRFU,WU |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Atypical | 9 | 0.93 | 2.0 | 18 | 0.23 | 159 | 605 | ||
| 2 | Typical | 26 | 0.76 | 2.1 | 28 | 0.48 | 118 | 653 | ||
| 3 | Typical | 9 | 0.93 | 2.4 | 20 | 0.39 | 128 | 634 | ||
| 4 | Typical | 38 | 0.87 | 4.0 | 12 | 0.27 | 136 | 426 | 206 | 389 |
| 5 | Typical | 16 | 0.97 | 2.5 | 11 | 0.15 | 247.8 | 451.6 | 265 | 419 |
| 6 | Atypical | 42 | 0.93 | 1.1 | 16 | 0.32 | 162.6 | 319.6 | ||
| 7 | Typical | 38 | 0.91 | 1.9 | 31 | 0.52 | 108 | 659 | ||
| 8 | Atypical | 42 | 0.94 | 4.5 | 10 | 0.26 | 201 | 343 | ||
| Mean±SD | 27.5±13 | 0.9±0.06 | 2.3±0.9 | 18.5±6 | 0.4±0.3 | 157±45 | 511±142 |
AF, absolute flow; AFFU, absolute flow at follow-up; CFR, coronary flow reserve; FFR, fractional flow reserve; h, hours since symptom onset; IMR, index of microvascular resistance; MR, myocardial resistance; MRFU, myocardial resistance at follow up; SD, standard deviation; Tmnhyp, hyperemic mean transit time in seconds.
The present study reports the first AF measurement in the setting of TTC using the thermodilution technique with continuous saline infusion. In all patients, the procedure was easily performed and took about 5minutes once the catheter and the wire were set. The safety of this technique is demonstrated by the absence of any complications or adverse effects. This method has been recently developed and some in vivo data have been published in the setting of ischemic cardiomyopathy.4–6 Compared with Doppler measurements and thermodilution based on bolus injection, this method has some significant advantages: a) it is a completely operator-independent procedure; b) adenosine is not necessary since hyperemia is induced by saline infusion2; and c) it is highly reproducible.1,4,5 Xaplanteris et al.6 assessed the feasibility of the technique in a series of 135 ischemic patients. The mean AF value was 189 [151-235mL/min] and MR was 390 [347-466 WU] in the left anterior descending coronary artery. We found a slightly lower AF and higher MR in TTC patients. In addition, our results are quite concordant with those reported in a previous series of patients with a high prevalence of microvascular disease.2 However, this comparison with previous studies should be interpreted with caution, since there are no available data providing clear reference values for this method. Furthermore, our study has a small sample size and the myocardial mass volume perfused in each patient was unknown. Therefore, the usefulness of this technique in the diagnosis or prognosis of TTC remains to be established.
In conclusion, the thermodilution technique using continuous saline infusion allows safe and feasible measurement of AF and MR in the setting of TTC. This technique provides unique and novel insights into the pathophysiology of this elusive entity and opens new avenues for its elucidation.
FUNDINGThis work was supported by grants from the Iniciativa territorial (ITI) 2014–2020 para la provincia de Cádiz, from Consejería de Salud and from Fondo Europeo de Desarrollo Regional (FEDER).