To the Editor,
Long QT Syndrome Type 3 (LQT3) is caused by mutations in the SCN5A gene which result in a hyperactive sodium channel. Although beta -blockers are the only therapeutic option outlined in clinical guidelines,1 the addition of a sodium channel blocker drug (such as mexiletine, lidocaine, flecainide, and ranolazine) can also be useful.2, 3, 4 However, not all sodium blockers have the same effect in the channel. Some preferably bind to activated open channels (such as flecainide), while others do so to inactivated channels (such as mexiletine and lidocaine). There are very few studies published regarding the effect of these drugs in patients with LQT3 and their effectiveness has not been compared in any regulated manner.
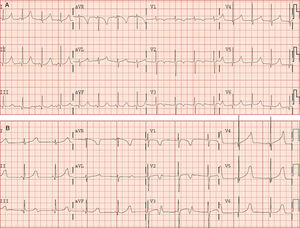
A 2-year-old girl was diagnosed with possible LQT following the chance discovery of a QTc interval of 485ms (Figure 1A) and up to 530ms during periods of intermittent 2:1 atrioventricular block (AVB) (Figure 1B), asymptomatic at all times. There was no family history of this condition and the girl's parents were also asymptomatic, with normal electrocardiogram results. After obtaining the relevant informed consent to proceed, bidirectional direct sequencing was performed on the exons and introns adjacent to the KCNQ1, KCNH2, and SCN5A genes in DNA taken from the child's peripheral blood.
Figure 1. Electrocardiogram without medication. A: sinus rhythm, normal atrioventricular conduction, and QTc 485ms. B: sinus rhythm, 2:1 second degree atrioventricular block and QTc 530ms.
A SCN5A V411M mutation was detected in heterozygosis which was not present in either parent. Recently, Horne et al. studied the functional behavior of said mutation (SCN5A V411M) with different sodium channel blockers. They did not find any relevant changes in vivo in the QTc of a newborn baby with said mutation, long QT and 2:1 AVB, after administering lidocaine or mexiletine. However, the addition of flecainide significantly improved the repolarization of in vitro cell samples.5
SCN5A V411M mutation leads to a hyperactive sodium channel, apparently due to an increase in the probability of aperture of the mutated channel during the plateau and repolarization phases. Drugs such as flecainide, which binds to open channels, can be more effective than other sodium blockers that have more affinity to inactivated channels.
In light of these results, the patient was admitted and monitored, and tests using orally administered flecainide (up to 4mg/kg/day in 2 doses) were carried out. The flecainide was added to the background medication (oral propranolol 2mg/kg/day). The clinical tolerance was excellent, the intermittent 2:1 AVB disappeared, the QTc decreased considerably (to 440ms) after 3 days of the new therapeutic regime, and continued in that manner. The patient has had no arrhythmic episodes of note over the 7 months of treatment (Figure 2).
Figure 2. Electrocardiogram 7 months after treatment with flecainide 4mg/kg/day and propranolol 2mg/kg/day. Sinus rhythm, normal atrioventricular conduction, and QTc 440ms.
Given the rarity of this illness6 and the difficulties for genetic diagnosis in many centers, clinical cardiologists are frequently unaware of other therapeutic options for patients with LQT3, except for beta -blockers and defibrillators. If we also take into consideration the limitations presented by the use of defibrillators in young children, the role of sodium channel blockers is of utmost importance in patients with phenotypes where the use of such devices is not indicated.
This study contributes additional data to those recently published by Horne et al.5 regarding the SCN5A V411M mutation. It provides new clinical and electrocardiographic data that endorse the use of flecainide in this mutation.
These data suggest that the effect of sodium blocker drugs can be, at least in part, dependent on the type of mutation, which could thereby predict a differential effect from those based on functional studies, with more benefit being gained from one drug or another depending on the specific mutation identified.
Acknowledgments
This study was partially financed with grants from the Instituto de Salud Carlos III (PI07/0831, PI11/00019, CP07/00326, CP09/00065, and RECAVA network RD06/0014/0004).
Corresponding author: zorio_est@gva.es