Recently, different strategies have been described for achieving commissural alignment during transcatheter aortic valve implantation (TAVI).1–3 Computed tomography (CT) is the most accurate imaging technique to measure final orientation after TAVI implant. However, post-TAVI CT is not performed routinely and not clinically justified. Other strategies like co-registry of pre-TAVI CT and fluoroscopy could be useful but are not the standard of care.1 We propose an algorithm to identify the final position of TAVI devices with recognizable commissural markers relying only in fluoroscopy with a resolution of 15° degrees.
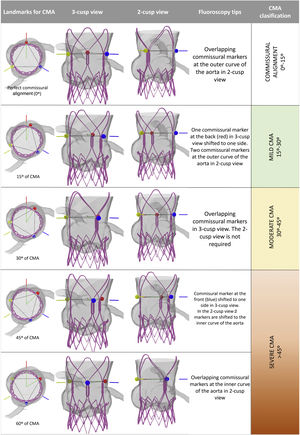
Using a CT derived aortic root simulation, different rotational orientations of a virtual TAVI device were tested, ranging from perfect commissural alignment to complete misalignment. The relationship between the commissural markers (CM) and the native commissures was evaluated in a simulated 3-cusp and 2-cusp (right coronary cusp to left coronary cusp) views. From the results obtained, we can determine the degree of commissural misalignment (CMA) as follows (figure 1, ):
- 1.
Perfect commissural alignment (0°): in the 3-cusp view one commissural marker is centered back. In the 2-cusp view, 2 commissural markers are overlapping each other at the outer curve of the aorta.
- 2.
15-degree CMA (15°): the CM located at the back of the aorta is shifted to one side, intersecting the inner quarter radius of the stent frame in the 3-cusp view. In the 2-cusp view, 2 CM are close to the outer curve of the aorta.
- 3.
30-degree CMA (30°): in the 3-cusp view 2 CM are overlapping, either at the inner or at the outer curve of the aorta, depending on the direction of the misalignment. The 2-cusp view is not needed in this orientation.
- 4.
45-degree CMA (45°): in the 3-cusp view one CM is shifted to one side of the center of the aorta, intersecting the inner quarter of stent frame radius. Conversely to the 15° position, in the 2-cusp view two CM appears close to the inner curve of the aorta.
- 5.
60-degree CMA (60°): in the 3-cusp view the image is similar to the “perfect commissural alignment”. However, in this case one CM is centered front. In the 2-cusp view 2 CM appear overlapping at the inner curve of the aorta.
Landmarks for fluoroscopic identification of commissural alignment. CMA: commissural misalignment. Red line: left coronary to non-coronary native commissure. Blue line: left coronary to right coronary native commissure. Yellow line: right coronary to non-coronary native commissures. Colored circles highlight the commissural markers of the transcatheter aortic valve implantation device (colors match the lines of the native commissures in a commissural aligned implant). CMA, commissural misalignment.
The proposed algorithm stratifies the orientation of TAVI using the current stablished classification for CMA1: aligned (0°-15°), mild CMA (15°-30°), moderate CMA (30°-45°) and severe CMA (45°-60°).
The clinical applicability of this algorithm was tested in 18 patients. Twelve patients were included in an ongoing prospective study evaluating a method to achieve a commissural alignment implant,3 CT was used to measure the final implant orientation. Other 6 patients who received a conventional implant were included; in those cases, fluoroscopy, and CT co-registry1 were used to evaluate the implant orientation. Patients provided informed consent and the study was approved by the ethical committee of the center. One cardiologist, blinded to the results, was trained in the proposed algorithm; 16/18 patients were correctly assigned to their CMA group, only 2 cases with a CMA near 15° were misclassified as good commissural alignment while CT scan reveal mild CMA.
There are some limitations of this method: a) TAVI devices without identifiable radiopaque markers for all 3 commissural posts (Evolut Medtronic, USA) cannot be evaluated although newer iteration will incorporate them; b) 2 complementary projections are needed to perform the analysis (3-cusp and 2-cups views), but there is no need for additional contrast dye administration.
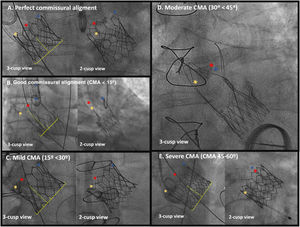
Examples of actual cases with assessment of the degree of CMA using the aforementioned algorithm are shown in figure 2.
Examples of the application of the algorithm for commissural alignment assessment. A: perfect commissural alignment. One commissural marker is centered in 3-cusp view and 2 commissural markers are overlapped at the outer curve of the aorta in 2-cusp view. B: good commissural alignment (< 15°). One commissural marker is shifted to one side within inner quarter of the radius of the valve stent frame with overlapped commissural markers at the outer curve of the aorta in 2-cusp view. C: mild commissural misalignment (15°-30°). One commissural marker is shifted beyond the inner quarter in the 3-cusp view with two commissural markers located at the outer curve of the aorta in the 2-cusp view. D: moderate commissural misalignment (30°-45°): commissural markers are overlapping at either side in the 3-cusp view. E: severe commissural misalignment (45°-60°). One commissural marker is within the inner quarter of the stent frame radius in the 3-cusp view and 2 commissural markers are located at the inner curve of the aorta; in the worst scenario (a misalignment at 60°), one commissural marker is centered in the 3-cusp view with commissural markers overlapping at the inner curve of the aorta in 2-cusp view. CMA, commissural misalignment.
In conclusion, the degree of CMA of TAVI can be easily measured immediately after the implant based exclusively on fluoroscopy. CMA has not only investigational relevance, but also potential clinical benefits in patients requiring eventual coronary angiograms or valve-in-valve procedures and might be associated to better residual gradients, lower pacemaker rate, and reduced risk of leaflet thrombosis.
FUNDINGThis investigation received funding resources from the Spanish Society of Cardiology (SEC) with the grant number: SEC/FEC-INV-CLI 21/023. Alfredo Redondo Diéguez is beneficiary of a Contrato Rio Hortega grant from the Instituto de Salud Carlos III: CM20/00068. The project was developed thank to a FIS grant (PI21/01188, from the Instituto de Salud Carlos III, Madrid, Spain).
AUTHORS’ CONTRIBUTIONSA. Redondo designed the project and, in collaboration with I.J. Amat-Santos and S. Santos-Martínez, wrote the final manuscript. R. Delgado-Arana, C. Baladrón Zorita and J.A. San Roman performed a critical review and approved the final version of the manuscript
CONFLICTS OF INTERESTI.J. Amat-Santos is proctor for Boston Scientific, Meril Life and Medtronic. There are no other conflicts of interest to declare.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.08.010