Immunoglobulin (Ig) G4-related disease (IgG4-RD) is a fibroinflammatory process first described in 2003, with frequent multiorgan involvement, most often involving the pancreas, lungs, or retroperitoneum.1 Cardiac manifestations, however, are rare, with only a few reported cases.2
We present the case of a 47-year-old previously healthy man, brought to our emergency department following resuscitation from out-of-hospital cardiac arrest in a shockable rhythm. An electrocardiogram after return of spontaneous circulation showed high-degree atrioventricular block with a varying escape rhythm.
On admission, he was awake and asymptomatic and, after exclusion of major echocardiographic abnormalities, a transvenous temporary pacemaker was implanted; a coronary angiogram showed no significant coronary artery disease. Backup pacing to allow for intrinsic rhythm was initially preferred, but the patient developed a torsade de pointes, which was promptly shocked. The pacemaker frequency was increased with no further arrhythmias, so that the initial arrest was interpreted as bradycardia-dependent.
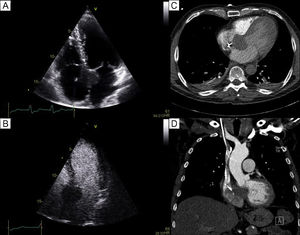
Careful echocardiographic examination, complemented by transoesophageal imaging, displayed a nodular mass extending from the aortic root into the interatrial septum, without obstruction or valvular dysfunction; the mass was not opacified by ultrasonographic contrast (Figure 1A-B). Because the temporary pacemaker contraindicated magnetic resonance imaging, computed tomography was performed, showing a 36 × 37mm mass with a density similar to that of the interventricular septum (Figure 1C-D).
A: transthoracic echocardiography revealing the nodular mass in the interatrial septum, near the mitral and tricuspid valves, without opacification after ultrasonographic contrast administration (B). C, D: computed tomography displayed the 36 × 37mm mass with a density similar to that of the interventricular septum.
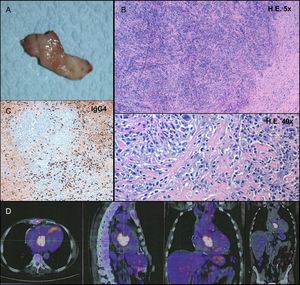
After Heart Team discussion, a decision was made to attempt to distinguish a malignant neoplasm from a benign process to inform the choice between palliative care and a curative approach. An echo-guided percutaneous biopsy was performed, revealing only nonspecific inflammatory infiltrate. In the absence of evidence of malignancy, cardiac surgery revealed an inextricable tumoral mass at the center of the heart, closely related to the aortic, mitral, and tricuspid valves. A surgical specimen was collected (Figure 2A), with intraoperative frozen section examination suggesting a benign connective tissue neoplasm; a definitive pacemaker was implanted and the procedure terminated.
A: macroscopic appearance of the surgical specimen. B: hematoxylin-eosin (HE) staining demonstrated a fibrotic lesion with a storiform pattern and a rich inflammatory infiltrate. C: a large population of plasma cells was evidenced on immunohistochemistry, with an elevated number of IgG4-producing cells (274 per high power field). D: positron emission tomography scan confirmed the hypermetabolic cardiac lesion, without extracardiac involvement.
The patient was discharged with no other intercurrent events and remained asymptomatic. Histopathologic examination of the surgical specimen showed a fibrotic stroma with spindle-shaped cells in a storiform pattern and no significant atypia; obliterative phlebitis was also observed. This diffuse lesion was remarkable for the presence of an exuberant chronic inflammatory process with numerous plasma cells and polymorphonuclear leukocytes; immunohistochemistry showed the predominance of IgG4-producing plasma cells (274 per high power field; Figure 2B-C). This prompted further immunological evaluation that confirmed increased IgG4 serum levels (202mg/dL).
A diagnosis of IgG4-RD of the heart was made and a positron emission tomography-scan obtained, confirming the presence of the hypermetabolic intracardiac mass; no extracardiac metabolically active tumoral lesions were found (Figure 2D). The patient was started on prednisone, with no additional symptoms and normalization of IgG4 serum levels, but imaging follow-up at 1 year showed no significant response. Rituximab was attempted as second-line therapy, although without mass reduction, and consequently a watchful approach was decided.
Although infrequent, cardiovascular involvement in IgG4-RD has been described in cases of aortic aneurism, aortitis, pericarditis, and coronary artery pseudotumors2,3; intracardiac pseudotumors, however, are found only in exceedingly rare reports.4–6 The latter usually present as heart failure, due to valvular dysfunction, associated in 2 cases with atrioventricular conduction disturbances.4,5 Cardiac arrest has been described as a result of ischemia in the context of coronary involvement.2
Some authors have reported successful steroid therapy for the reduction of residual lesions after surgery,4 but there are also cases in which these agents were only able to stop tumoral growth6 and even 1 patient who developed symptoms under steroid therapy for extracardiac disease.5
To the best of our knowledge, this is the first reported case of cardiac IgG4-RD presenting as nonischemic cardiac arrest. It is also the first to report the use of rituximab, a B-cell depleting agent currently regarded as second-line therapy in IgG4-RD. While clinically stable, our patient showed no signs of mass reduction; we hypothesize that these therapeutic strategies act on the inflammatory component of the lesions, but are probably unable to reduce the established fibrotic reaction.
.
We would like to thank the contribution of the multidisciplinary team involved in the management of the patient, including Doctors Rui Almeida, Helena Baldaia, João Carlos Silva, and Jorge Almeida.