Network systems have achieved reductions in both time to reperfusion and in-hospital mortality in patients with ST-segment elevation myocardial infarction (STEMI). However, the data have not been disaggregated by sex. The aim of this study was to analyze the influence of network systems on sex differences in primary percutaneous coronary intervention (pPCI) and in-hospital mortality from 2005 to 2015.
MethodsThe Minimum Data Set of the Spanish National Health System was used to identify patients with STEMI. Logistic multilevel regression models and Poisson regression analysis were used to calculate risk-standardized in-hospital mortality ratios and incidence rate ratios (IRRs).
ResultsOf 324 998 STEMI patients, 277 281 were selected after exclusions (29% women). Even when STEMI networks were established, the use of reperfusion therapy (PCI, fibrinolysis, and CABG) was lower in women than in men from 2005 to 2015: 56.6% vs 75.6% in men and 36.4% vs 57.0% in women, respectively (both P<.001). pPCI use increased from 34.9% to 68.1% in men (IRR, 1.07) and from 21.7% to 51.7% in women (IRR, 1.08). The crude in-hospital mortality rate was higher in women (9.3% vs 18.7%; P<.001) but decreased from 2005 to 2015 (IRRs, 0.97 for men and 0.98 for women; both P < .001). Female sex was an independent risk factor for mortality (adjusted OR, 1.23; P<.001). The risk-standardized in-hospital mortality ratio was lower in women when STEMI networks were in place (16.9% vs 19.1%, P<.001). pPCI and the presence of STEMI networks were associated with lower in-hospital mortality in women (adjusted ORs, 0.30 and 0.75, respectively; both P<.001).
ConclusionsWomen were less likely to receive pPCI and had higher in-hospital mortality than men throughout the 11-year study period, even with the presence of a network system for STEMI.
Keywords
Rapid advances in reperfusion therapies and pharmacotherapies for ST-segment elevation myocardial infarction (STEMI) and its associated risk factors have helped to reduce the incidence and mortality associated with this disease in recent years.1,2 The introduction of STEMI network systems has had a particularly beneficial effect on the care of patients with STEMI.3–7 However, the overall burden associated with STEMI remains high. The estimated annual incidence of acute myocardial infarction (AMI) is fluctuating in different countries and the estimated annual mortality rate is highly variable among European regions, with in-hospital mortality ranging from 4.1% in northern countries to 10.1% in eastern countries and similar variability evident in North American regions.8,9 Women hospitalized with STEMI are at a higher risk of adverse outcomes than men.10–12 The underlying reasons for this difference are multifactorial and include an older age at presentation, higher comorbidity burden, delayed presentation with more atypical symptoms, and sex-based differences in treatment.10–14 Other studies have shown that women presenting with STEMI are less likely to undergo revascularization and have higher risk-adjusted in-hospital mortality than men.10–12 Nonetheless, it is not completely understood whether the higher mortality in women is driven by a worse baseline risk profile or by sex-based disparities in treatment.
Although network systems have achieved significant reductions in time to reperfusion and in-hospital mortality in patients with STEMI, the data have not been disaggregated by sex.3–9 Hence, we analyzed the sex-stratified trends and influence of a network system on reperfusion and mortality in STEMI to further study their temporal changes from 2005 to 2015 in Spain.
METHODSStudy design, data source, and patient populationWe conducted a retrospective longitudinal study using information derived from the Minimum Data Set (MDS) of the Spanish National Health System (SNHS). This administrative database includes the demographic and clinical information of all patients discharged from all public hospitals affiliated with the SNHS. The information included age, sex, principal diagnosis, up to 13 secondary diagnoses, and up to 20 procedures performed during hospitalization, all coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). All episodes with a principal diagnosis of STEMI from January 1, 2005, to December 31, 2015, were included. A principal diagnosis of STEMI was identified by ICD-9-CM codes (410.x1, except 410.71). We described the temporal trends in reperfusion procedures (thrombolysis, percutaneous coronary intervention [PCI], and coronary artery bypass grafting [CABG]). PCI was identified by ICD-9-CM codes 00.66, 36.01, 36.02, 36.05, 36.06, and 36.07; thrombolysis by V45.88 and 99.10; and CABG by 36.10 to 36.19. Primary PCI (pPCI) was considered to have been performed when PCI codes were not accompanied by thrombolysis codes in the same episode.15 Isolated coronary angiography was identified by codes 88.56 to 88.57 without PCI codes in the episode.
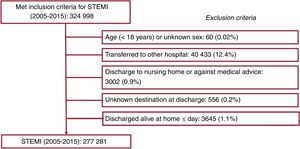
To improve the consistency and quality of the data, we excluded all episodes lacking information on sex, age, admission date, or principal diagnosis, as well as patients who were discharged alive to home after a hospital length of stay of 1 day or less, those whose reason for discharge was unclear, and those who left against medical advice. Discharges to other hospitals were also excluded to avoid duplicate episodes of patients transferred to other hospitals after PCI. The use of the MDS of the SNHS to study acute coronary syndrome has previously been validated.16
Regional STEMI networksThe year of the development of organized care systems for STEMI patients in the different autonomous communities was checked against data from the National Cardiac Catheterization and Interventional Cardiology Annual Registry in each autonomous community.17
Analyzed outcomesThe primary end point was an analysis of the influence of network systems on sex differences in in-hospital mortality in patients with STEMI according to age group from 2005 to 2015. In-hospital mortality was defined as death from any cause during a hospitalization episode. The secondary end point was a comparison of differences between the sexes in the use of reperfusion techniques (PCI, thrombolysis, and CABG) for STEMI and their impact on in-hospital mortality.
Statistical analysisThe risk-standardized in-hospital mortality ratio (RSMR) was defined as the ratio between the predicted mortality and expected mortality (which considers a standard performance according to the average of all hospitals) multiplied by the crude mortality rate. The RSMR was calculated using logistic regression multilevel risk adjustment models developed by the Medicare and Medicaid Service,18 which were adapted to the structure of the MDS database and considered interhospital variability and clinical and demographic variables. Secondary diagnoses were included in the groups of risk factors described by Pope19 and updated each year by the Agency for Health Research and Quality. For the adjustment model, we considered only comorbidities with an odds ratio (OR) > 1.0. Levels of significance for selecting and eliminating risk factors were P <.05 and P ≥ .10, respectively. Model discrimination was assessed by calculating receiver operating characteristics (ROC) curves and their corresponding areas under the curve (AUROCs). The RSMR was used to compare outcomes related to sex and the effect of regional AMI networks on pPCI performance.
Temporal trends in in-hospital mortality during the observation period were modeled using Poisson regression analysis with years as the only independent variable. In all models, incidence rate ratios (IRRs) and their 95% confidence intervals (95%CIs) were calculated.
Continuous variables are expressed as mean±standard deviation and categorical variables as numbers and rates. A t test was used to compare 2 categories and ANOVA corrected by the Bonferroni test was used to compare 3 or more categories. Categorical variables were compared by the chi-square test or Fisher exact test. All statistical tests were 2-sided, and the level of significance for P values was set at .05. Statistical analysis was performed using STATA 13 and SPSS 21.0.
RESULTSBaseline characteristicsOut of 324 998 STEMI episodes in patients ≥ 18 years old hospitalized in Spain from 2005 to 2015, 277 281 were selected after exclusions (figure 1); 80 547 (29%) were women. Women were 10 years older than men (mean age, 64.3±13.7 vs 74.7±13.1 years; P <.001). Comorbidities were more frequent in women, but women were less likely to be smokers, to have cancer, chronic obstructive pulmonary disease, or chronic liver disease, and to have undergone invasive procedures related to ischemic heart disease (table 1). Women more frequently had cardiac failure and cardiogenic shock in the episode than men (table 1).
Baseline demographics and comorbidities in patients with ST-segment elevation myocardial infarction during admission
| Men(n=196 734) | Women(n=80 547) | P | |
|---|---|---|---|
| Age, y | 64.3±13.7 | 74.7±13.1 | <.001 |
| Smoking (ICD-9-CM codes V15.82, 305.1) | 33 641 (17.1) | 1691 (2.1) | <.001 |
| Hypertension (CC 89, 91) | 90 629 (46.1) | 48 050 (59.7) | <.001 |
| DM or DM complications, except proliferative retinopathy (CC 15-20, 120) | 50 690 (25.8) | 28 530 (35.4) | <.001 |
| Stroke (CC 95-96) | 1718 (0.9) | 1177 (1.5) | <.001 |
| Cerebrovascular disease (CC 97-99, 103) | 4298 (2.2) | 2638 (3.3) | <.001 |
| Vascular disease and complications (CC 104-105) | 20 182 (10.3) | 8453 (10.5) | .06 |
| Renal failure (CC 131) | 19 237 (9.8) | 11 042 (13.7) | <.001 |
| COPD (CC 108) | 18 977 (9.6) | 2621 (3.3) | <.001 |
| Chronic liver disease (CC 25-27) | 925 (0.5) | 72 (0.1) | <.001 |
| Valvular or rheumatic heart disease (CC 86) | 20 008 (10.2) | 14 373 (17.8) | <.001 |
| History of PTCA (ICD-9-CM code V45.82) | 15 413 (7.8) | 3870 (4.8) | <.001 |
| History of CABG surgery (ICD-9-CM code V45.81) | 2748 (1.4) | 654 (0.8) | <.001 |
| Other acute/subacute forms of ischemic heart disease (CC 82) | 16 304 (8.3) | 8708 (8.3) | .724 |
| Mechanical complications (ICD-9-CM code 423.3 without 996.03, 996.70-996.79, or 998.2 in the same episode; 429.71; 429.6; 429.5) | 506 (0.3) | 307 (0.4) | <.001 |
| Congestive heart failure (CC 80) | 42 800 (21.8) | 26 831 (33.3) | <.001 |
| Cardiorespiratory failure or shock (CC 79 without cardiogenic shock [ICD-9-CM code 785.51]) | 17 522 (8.9) | 8736 (10.8) | <.001 |
| Cardiogenic shock (ICD-9-CM code 785.51) | 10 352 (5.3) | 6433 (8) | <.001 |
| Pneumonia (CC 111-113) | 9319 (4.7) | 5968 (7.4) | <.001 |
| Protein-calorie malnutrition (CC 21) | 470 (0.2) | 361 (0.4) | <.001 |
| Dementia or other specified brain disorders (CC 49-50) | 6190 (3.1) | 6451 (8) | <.001 |
| Hemiplegia, paraplegia, paralysis, and functional disability (CC 67-69, 100-102, 177-178) | 4484 (2.3) | 2328 (2.9) | <.001 |
| Metastatic cancer, acute leukemia, and other severe cancers (CC 7-8) | 2430 (1.2) | 672 (0.8) | <.001 |
| Trauma in last year (CC 154-156, 158-162) | 793 (0.4) | 414 (0.5) | <.001 |
CABG, coronary artery bypass graft; CC, Condition Category20; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus; ICD-9-CM, International Classification of Diseases, Ninth Edition, Clinical Modification; PTCA, percutaneous transluminal coronary angioplasty.
Data are expressed as No. (%) or mean±standard deviation. Comorbidities were extracted from the database using International Classification of Diseases, Ninth Edition, Clinical Modification codes.
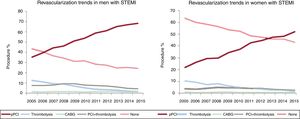
Temporal trends in revascularization in men and women are shown in figure 2. The use of reperfusion therapy (PCI, CABG, and fibrinolysis) increased in both sexes from 2005 to 2015: from 56.6% to 75.6% in men (IRR, 1.02; 95%CI, 1.02-1.03; P <.001) and from 36.4% to 57% in women (IRR, 1.04; 95%CI, 1.04-1.05; P <.001). However, women were less likely to undergo pPCI therapy for STEMI than men in the overall cohort (53.1% vs 36.9%, P <.001). This sex-related gap in pPCI performance was maintained after adjustment for age and comorbidities (OR, 0.69; 95%CI, 0.68-0.70) (). Overall, the pPCI rate increased from 2005 to 2015: from 34.9% to 68.1% in men (IRR, 1.07; 95%CI, 1.06-1.08; P <.001) and from 21.7% to 51.7% in women (IRR, 1.08; 95%CI, 1.07-1.1; P <.001), whereas the performance of thrombolysis alone or associated with pPCI decreased in both sexes from 2005 to 2015: from 19.8% to 5.6% in men (IRR, 0.82; 95%CI, 0.81-0.83; P <.001) and from 13.7% to 4.1% in women (IRR, 0.85; 95%CI, 0.83-0.86; P <.001). CABG was performed in 1.3% of men and 0.7% of women (P <.001), without any statistically significant variations throughout the study period in both men and women (from 1.5% to 1.2% in men and from 0.8% to 0.8% in women) (figure 2).
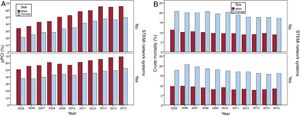
Influence of network systems on the use of primary PCIIn our cohort, 32.3% of patients with STEMI (32.6% of men and 31.5% of women) were managed through a network system. pPCI was more frequently performed, in both men and women, when a regional AMI network was present (63.5% vs 48.1% in men and 46.6% vs 32.4% in women; both P <.001). Even with the presence of a STEMI network system, women were less likely than men to be treated with pPCI (63.5% vs 46.6%; P <.001) throughout the overall study period (figure 3A). The pPCI rate increased from 2005 to 2015 whether AMI networks were present or not in both men (IRRs, 1.03; 95%CI, 1.02-1.03 vs 1.07; 95%CI, 1.06-1.08; P <.001) and women (IRRs, 1.03; 95%CI, 1.03-1.04 vs 1.09; 95%CI, 1.07-1.10; P <.001). The relative differences between men and women in pPCI performance were maintained over the 11-year study period, even with the presence of a regional network system for the care of STEMI, with PCI performed 19% less frequently in women than in men (figure 3A). Differences in pPCI performance between men and women were statistically significant for all age groups, except for those aged between 18 and 34 years. Differences between the sexes in the pPCI rate increased with age from−9% (35-44 years old) to 50% (> 94 years old) ().
Trends in PCI performance from 2005 to 2015 for men and women. A: PCI in men with STEMI vs women according to network system presence. B: mortality in men with STEMI vs women according to network system presence. P <.001 for both PCI and mortality. PCI, percutaneous coronary intervention; pPCI, primary PCI; STEMI, ST-segment elevation myocardial infarction.
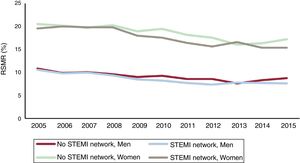
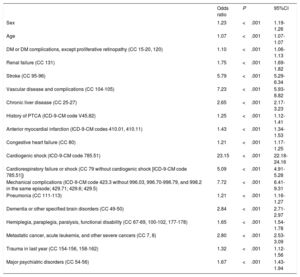
The crude in-hospital mortality rate for the whole study period was higher in women than in men (9.3% vs 18.7%, P <.001). Clinical and demographic variables independently associated with in-hospital mortality in the multilevel risk adjustment model are shown in table 2. This model showed a good discriminative ability (AUROC, 0.90; 95%CI, 0.90-0.90) and calibration (P < .001) (). Female sex was independently associated with higher in-hospital mortality (OR, 1.23; 95%CI, 1.19-1.26; P <.001) (table 2). There was a statistically significant interaction between age and sex in STEMI mortality (P=.03). However, female sex was a statistically significant risk-adjusted risk factor in all age groups, except the oldest group (> 94 years old) (). The crude in-hospital mortality rate decreased for both men and women from 2005 to 2015: from 11.1% to 8.4% in men (IRR, 0.97; 95%CI, 0.97-0.98; P <.001) and from 20.5% to 16.4% in women (IRR, 0.98; 95%CI, 0.97-0.98; P <.001) (figure 3B). Furthermore, the RSMR decreased during the study period in both men (IRR, 0.97; 95%CI, 0.96-0.97; P <.001) and women (IRR, 0.97; 95%CI, 0.97-0.97; P <.001), regardless of whether a STEMI network had been established (figure 4). In addition, the RSMR was lower for women with STEMI where regional networks were in place (19.1%±4.6% vs 16.7%±4.6%; P <.001) (figure 4).
Demographic and clinical variables independently associated with in-hospital mortality
| Odds ratio | P | 95%CI | |
|---|---|---|---|
| Sex | 1.23 | <.001 | 1.19-1.26 |
| Age | 1.07 | <.001 | 1.07-1.07 |
| DM or DM complications, except proliferative retinopathy (CC 15-20, 120) | 1.10 | <.001 | 1.06-1.13 |
| Renal failure (CC 131) | 1.75 | <.001 | 1.69-1.82 |
| Stroke (CC 95-96) | 5.79 | <.001 | 5.29-6.34 |
| Vascular disease and complications (CC 104-105) | 7.23 | <.001 | 5.93-8.82 |
| Chronic liver disease (CC 25-27) | 2.65 | <.001 | 2.17-3.23 |
| History of PTCA (ICD-9-CM code V45.82) | 1.25 | <.001 | 1.12-1.41 |
| Anterior myocardial infarction (ICD-9-CM codes 410.01, 410.11) | 1.43 | <.001 | 1.34-1.53 |
| Congestive heart failure (CC 80) | 1.21 | <.001 | 1.17-1.25 |
| Cardiogenic shock (ICD-9-CM code 785.51) | 23.15 | <.001 | 22.18-24.16 |
| Cardiorespiratory failure or shock (CC 79 without cardiogenic shock [ICD-9-CM code 785.51]) | 5.09 | <.001 | 4.91-5.28 |
| Mechanical complications (ICD-9-CM code 423.3 without 996.03, 996.70-996.79, and 998.2 in the same episode; 429.71; 429.6; 429.5) | 7.72 | <.001 | 6.41-9.31 |
| Pneumonia (CC 111-113) | 1.21 | <.001 | 1.16-1.27 |
| Dementia or other specified brain disorders (CC 49-50) | 2.84 | <.001 | 2.71-2.97 |
| Hemiplegia, paraplegia, paralysis, functional disability (CC 67-69, 100-102, 177-178) | 1.65 | <.001 | 1.54-1.78 |
| Metastatic cancer, acute leukemia, and other severe cancers (CC 7, 8) | 2.80 | <.001 | 2.53-3.09 |
| Trauma in last year (CC 154-156, 158-162) | 1.32 | <.001 | 1.12-1.56 |
| Major psychiatric disorders (CC 54-56) | 1.67 | <.001 | 1.43-1.94 |
95%CI, 95%, confidence interval; CC, Condition Category20; DM, diabetes mellitus; ICD-9-CM, International Classification of Diseases, Ninth Edition, Clinical Modification; PTCA, percutaneous transluminal coronary angioplasty.
Comorbidities were extracted from the database using International Classification of Diseases, Ninth Edition, Clinical Modification codes.
A multivariate regression model for adjusted in-hospital mortality considering only women identified the presence of heart failure or shock during admission as the most powerful independent predictor (OR, 23.3; 95%CI, 21.7-25; P <.001) (). This model showed good discriminative ability (AUROC, 0.86; 95%CI, 0.85-0.86) (). In addition, lower in-hospital mortality in women with STEMI was associated with the performance of pPCI during hospitalization (OR, 0.30; 95%CI, 0.26-0.32; P <.001) and the presence of a STEMI network system (OR, 0.75; 95%CI, 0.71-0.80; P <.001).
DISCUSSIONThis nationwide registry- and population-based observational study concerned patients with STEMI treated from 2005 to 2015, 29% (80 547) of whom were women. In this period, the crude in-hospital mortality rate in women was twice that in men (18.7% vs 9.3%) and 23% higher when adjusted for age and comorbidities. Our study reveals a higher in-hospital RSMR in women with STEMI than in men from 2005 to 2015, despite the presence of a network system. Although the RSMR was lower for women where regional networks were in place, their benefit was stronger for men.
In our cohort, STEMI network systems managed 32.3% of patients (32.6% of men and 31.5% of women) and pPCI rates for STEMI increased over time in both sexes. Nevertheless, women were less likely than men to be treated with pPCI, maintaining this disparity over the 11-year study period. Moreover, 43% of women with STEMI did not receive any reperfusion therapy in 2015 vs 24% of men. Differences in pPCI performance were found for all age groups, except for those aged 18 to 34 years.
Describing reperfusion therapy in 37 European countries, Kristensen et al.4 reported that there are still large national variations in treatment strategies for patients admitted with STEMI. Despite the recommendations of international guidelines, a substantial number of patients are still not offered any reperfusion therapy, particularly in some southern and eastern European countries. Several reasons can be postulated to explain these results. First, women were older and had more disabilities. They can therefore be considered to be less likely to obtain benefits from reperfusion therapies, although this supposition has not been proven in either clinical terms or in cost-benefit outcomes.20,21 On the other hand, lower revascularization rates can partially be explained by a higher frequency of alternative etiologies to atherosclerotic lesions, such as spontaneous coronary artery disease or coronary vasospasm in women.22 In contrast, it should be considered that these pathologies are more common in young patients and that they represent 6% of overall MIs in women (STEMI and non-STEMI).23 Nonetheless, our findings are consistent with previous reports showing a lower revascularization rate in women with STEMI than in men11,12,14,20,22 and indicate inequalities in medical care between the sexes, which may lead to increased mortality in women vs men.20,22 It is very unlikely that these differences can be explained by the higher incidence of MI without obstructive coronary disease in women. In our cohort, there was only a difference of 0.6 in the percentage of coronary angiography without PCI between women and men, and differences in pPCI were sustained and even higher in older age groups.
Claeys et al.5 showed that a STEMI network increased the pPCI rate from 60% to 80%, as in our study, but they did not perform a subanalysis of the impact of this increase on women, leaving the possible mortality causes unexplained.
Explanations for the higher mortality rates in womenIn our study, women with STEMI showed a 23% higher risk of adjusted in-hospital mortality vs men. In-hospital mortality was persistently increased in female STEMI patients after adjustment for common cardiovascular risk factors. However, although other authors did not find any differences between the sexes, age played a role, with increased mortality in young women and those ≥ 80 years.11,13,14
In our series, after multivariate risk adjustment, female sex was found to be an independent risk factor for in-hospital mortality. Although some unexplained biological reasons could contribute to this association, it must be taken into account that the pPCI delay was not recorded in the MDS of the SNHS. Besides, women with STEMI experience treatment delays at hospital arrival,5,7,12 which reduce the benefit of revascularization. Therefore, in our series, women more frequently experienced cardiogenic shock during admission than men (8% vs 5.3%; P <.001), possibly as a consequence of a more extensive MI due to a delay in the reperfusion therapy. One possible explanation for this finding is that STEMI is too often undetected in women because the symptoms are considered noncardiac, although chest pain is not as different between men and women as commonly thought.24 Women in our STEMI cohort were more likely to have heart failure than men, as a possible consequence of a combination of older age, late presentation, selection bias, and misdiagnosis. In our study, the most powerful factor contributing to mortality in women was the presence of heart failure or shock, in accordance with the findings of some other authors. All of these factors culminate in lower revascularization and higher mortality rates in women.25–27
STEMI-related in-hospital mortality in women: role of percutaneous coronary intervention and network systemsNetwork systems have been crucial in reducing mortality in patients with STEMI,5,7,20 offering equally good medical support to all inhabitants of communities with no interventional capabilities. Remarkably, we observed a trend for increased use of pPCI in the absence of an established regional network in hospitals with the interventional capabilities to implement the guideline recommendations for STEMI. The low percentage (32%) of episodes attended by STEMI networks during the study period (2005-2015) is because many autonomous communities had not established STEMI networks. These data are similar to those of other published studies.6
Our findings are consistent with those of previous studies on mortality in patients with STEMI that showed a higher mortality rate in women,2,14,20–27 although they focused on patient outcomes and none included the impact of network systems on mortality in women.
Despite considerable reductions in mortality in women with STEMI in recent decades, a significant gap is still evident.2,14,21,25–27 However, the reasons for this sex disparity in mortality are unclear. By collecting data from 8834 patients with STEMI treated in 41 hospitals and comparing the results from 2010 to 2016, Cenko et al.24 determined that women had a higher unadjusted 30-day mortality rate than men (11.6% vs 6.0%; P <.001). Wilkinson et al.25 showed a higher adjusted 30-day mortality in women vs men in a nationwide cohort study comprising 691 290 AMI hospitalizations in England between 2003 and 2013. A meta-analysis including over 700 000 patients (32% women) identified a consistently higher crude in-hospital mortality rate in women vs men.27 Nonetheless, the SWEDEHEART registry showed that the lower survival of women than men was attenuated by adjustment for the use of pharmacotherapies and an invasive coronary strategy, which suggests that sex-dependent differences in STEMI mortality are potentially modifiable through improvements in the guideline-indicated care, particularly the use of pPCI.11
We want to stress that our real-life setting contributes new insight into sex differences in STEMI care. The most important aspects of our study include an update on the current time frame and an analysis of the impact of regional network systems on these differences.
Although our study noted that some causes of the sex-based gap might include differences in women's risk factors, such as older age and comorbidities, we found excess mortality among female patients. Despite the presence of network systems, the performance of pPCI in women was lower than in men and, given the protective effect of pPCI on in-hospital mortality, these differences are probably related to the higher mortality observed in women.
Study limitationsThis study is a retrospective analysis of administrative data, with its inherent drawbacks. However, the use of administrative records to estimate outcomes in health care services has been validated by comparison with data from medical records16 and has been applied to research into health service outcomes.19
Our data specifically included hospitalized patients with STEMI and did not account for out-of-hospital deaths. The secondary diagnoses used as risk adjustment variables may correspond to conditions that are present on admission or to complications that may occasionally reflect inadequate treatment. There was no available information on some STEMI performance measures, such as the time from symptom presentation to reperfusion, angiographic data, or the use of guideline-recommended therapies. Finally, we cannot exclude the presence of unmeasured confounding factors that may adversely impact prognosis.
CONCLUSIONSWomen with STEMI had an adjusted risk of mortality 23% higher than that of men. Although the relative gap in the rate of PCI between women and men was reduced over the 11-year study period, PCI was still performed 19% less frequently in women than in men in 2015.
Women with STEMI had a lower percentage of pPCI. This finding could have contributed to the higher risk-adjusted in-hospital mortality in women. This difference in mortality was attenuated by the presence of regional network systems of STEMI care. Hence, the implementation of an integrated regional network to establish rapid reperfusion for STEMI patients offers the opportunity to reduce this inequality between the sexes.
FUNDINGThis study was sponsored by an unconditional grant from Menarini.
CONFLICTS OF INTERESTF. Marín reports personal fees from Bayer, Boehringer Ingelheim, AstraZeneca, Daiichi Sankyo, and Pfizer outside the submitted work. A. Sambola reports an unconditional grant from Amgen and personal fees from AstraZeneca, Novartis, Boehringer Ingelheim, Novo Nordisk, and Pfizer-BM outside the submitted work. J.L. Ferreiro reports personal fees from Eli Lilly Co, Daiichi Sankyo, Inc, Roche Diagnostics, Pfizer, Abbott, Boehringer Ingelheim, Bristol-Myers Squibb, Ferrer, and Boston Scientific and grants and personal fees from AstraZeneca outside the submitted work. H. Bueno reports grants from Instituto de Salud Carlos III, personal fees from Bayer and Novartis, grants, personal fees, and nonfinancial support from AstraZeneca, grants and personal fees from BMS-Pfizer, and personal fees from Ferrer, Medscape-theheart.org, and Janssen outside the submitted work. M. Anguita, Á. Cequier, N. Murga, C. Fernández, F.J. Elola, J.L. Bernal, and L. Rodríguez-Padial have nothing to disclose.
- -
The introduction of STEMI network systems has had a particularly beneficial effect on the care of patients with STEMI.
- -
Previous studies showed that women with STEMI are less likely to receive revascularization and have higher risk-adjusted in-hospital mortality than men. Nonetheless, it is not completely understood whether the higher mortality in women is driven by a worse baseline risk profile or by sex-based disparities in treatment.
- -
Although network systems have achieved significant reductions in time to reperfusion and in-hospital mortality in patients with STEMI, the data have not been disaggregated by sex.
- -
Women with STEMI had an adjusted risk of mortality 23% higher than that of men. Although the relative gap in the rate of PCI between women and men was reduced from 2005 to 2015, PCI was performed 19% less frequently in women in 2015.
- -
Women with STEMI had a lower percentage of pPCI, which may have contributed to the higher risk-adjusted in-hospital mortality in women.
- -
This difference in mortality was attenuated by the presence of regional network systems for STEMI. The implementation of a regional network to establish rapid reperfusion for STEMI patients may reduce inequality between the sexes.
The authors thank the Spanish Ministry of Health, Consumer Affairs, and Social Welfare for the facilities it has made available to the Spanish Society of Cardiology for the development of the RECALCAR study.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.08.001