To the Editor,
Kearns-Sayre syndrome is a rare disease linked to mitochondrial inheritance. The characteristic diagnostic triad consists of progressive external ophthalmoplegia, pigmentary degeneration of the retina, and atrioventricular block.1 It may also be associated with mental retardation, ataxia, deafness, muscle weakness, and endocrine disorders, such as diabetes mellitus or hypothyroidism. We present the case of a 37-year-old man with a noticeable phenotypic manifestation (Figure 1). From childhood, he had progressively presented photophobia, progressive loss of vision, external ophthalmoplegia, neurosensory deafness, Addison's syndrome, muscle weakness, and ataxia. His present clinical symptoms consisted of recurrent syncope and atrial flutter. The association of Kearns-Sayre syndrome with atrial flutter has not been described.
Figure 1. Patient phenotype. The presence of exophthalmos and bilateral ptosis is noticeable.
Twelve years before the current episode, he had been cardiologically assessed and diagnosed with Kearns-Sayre syndrome. At that time, the patient was asymptomatic, but the electrocardiogram showed right bundle-branch block and left anterior fascicular block. Periodic follow-up was prescribed. In the successive follow-ups, the patient remained asymptomatic with no changes in the electrocardiogram.
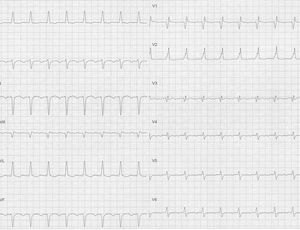
The onset of the current clinical symptoms started during the postoperative of a cholecystostomy, when the patient presented several episodes of syncope. The electrocardiogram disclosed atypical flutter rhythm and regular conduction with an approximate ventricular frequency of 106 bpm, right bundle-branch block, and left anterior fascicular block (Figure 2). The echocardiogram was normal. An electrophysiological study established the diagnosis of cavotricuspid isthmus-dependent flutter and counterclockwise rotation around the tricuspid valve. Isthmus ablation was performed successfully. After recovery of sinus rhythm, the atrioventricular conduction study showed prolongation of the HV interval and a short AH interval. Increased atrial stimulation disclosed worsening of infra-His conduction. These findings were considered to explain the recurrent syncope symptoms and therefore, a dual-chamber pacemaker was implanted. The patient subsequently remained asymptomatic, with no signs of further rhythm disorders. The most frequent and characteristic cardiac manifestation in this syndrome is conduction alteration, which progresses in an accelerated and unpredictable manner to complete block.2 This is considered the main mechanism behind an elevated incidence of sudden death in Kearns-Sayre syndrome.
Figure 2. Atypical atrial flutter with an image of right bundle-branch block and left anterior fascicular block.
The practice guidelines recommend pacemaker implantation in patients with Kearns-Sayre syndrome, Class I indication, and level of evidence C in the cases of third-degree and advanced second-degree (but still asymptomatic) atrioventricular block, and with Class IIb indication in any degree of block.3
We are not aware of any previous report of Kearns-Sayre syndrome associated with atrial flutter. Localized slow conduction is a necessary condition for a reentrant arrhythmia such as atrial flutter to occur. In Kearns-Sayre syndrome, only infra-His conduction defects have been described. It is unknown whether there may be other areas of slow conduction that would promote reentrant arrhythmias.
In this syndrome, the atrioventricular conduction abnormality is characterized by prolongation of His-ventricular associated with atrial-His shortening and therefore, the finding of a normal PR interval may be an error. We question the value of serial observation of the surface electrocardiogram to predict the occurrence of syncope due to the particularity of the conduction disorder and unpredictable progress.
In this case, it is possible that atrial flutter acted as a trigger of syncope, although the electrophysiological study after flutter ablation showed an infra-His conduction disorder. This finding, along with the association described between paroxysmal atrioventricular block and the high incidence of sudden death in these patients, justifies implantation of a pacemaker.
The association of this case with atrial flutter indicates the need to be aware of published series or cases that confirm other forms of cardiac involvement in Kearns-Sayre syndrome.