Currently, biological prostheses account for more than 80% of valves implanted by surgery. The possibility of transcatheter aortic valve implantation (TAVI) to replace a degenerated biological valve often tilts the balance towards the use of a bioprosthesis. This type of intervention is less invasive than open surgery. A meta-analysis found that hospital mortality rates were similar for TAVI and surgery.1 However, there is a lack of long-term results. When a bioprosthesis degenerates, this lack is sometimes used as an indication for open surgery on a hostile mediastinum that has already undergone intervention.
The aim of the present study was to compare long-term survival after TAVI vs open surgery for the treatment of degenerated aortic bioprostheses.
The study was a retrospective cohort study using prospective data collection from a digital database. Between January 2012 and November 2018, we selected all patients undergoing TAVI or open surgery in our hospital for degenerated bioprosthetic aortic valves. We excluded patients undergoing other valvular or concomitant proximal aortic surgery.
The primary objective was to compare long-term survival after the application of the 2 techniques. The secondary objective was to determine the combined survival rates and hospital readmission rates for cardiovascular causes.
Continuous variables are expressed as medians [interquartile range]. Patients were matched on propensity scores (PS) to minimize the bias inherent to observational studies. This score was calculated using logistic regression in which the dependent variable was TAVI or surgery. In line with expert recommendations, we selected as independent variables those theoretically related to survival.2 After we obtained the PS, open-surgery patients with a PS similar to that of the TAVI group were selected according to the nearest-neighbor method with replacement. The final balance between the 2 groups was verified using several statistical methods.
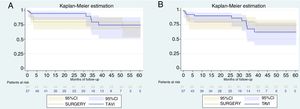
Once the pairs were created, Kaplan-Meier survival curves were compared using a stratified log-rank test.
The characteristics of the patients and the implanted prostheses are shown in Table 1. The analyzed cohort was at high surgical risk, with a EuroSCORE II of 7.1 [5.6-9.7] for TAVI and 8.6 [4.9-10.8] for surgery.
Baseline Variables Before and After Matching
| Raw Data | Matched Data | |||||
|---|---|---|---|---|---|---|
| Variable | TAVI | Surgery | SMD | TAVI | Surgery | SMD |
| Patients, n | 57 | 97 | 57 | 57 | ||
| Age, y | 79.82 | 74.98 | 0.55 | 79.82 | 78.81 | 0.11 |
| Women | 29 (50.9) | 42 (43.3) | 0.14 | 29 (50.9) | 35 (61.4) | -0.21 |
| Creatinine clearance, mL/min | 69.33 | 68.16 | .05 | 69.33 | 70.91 | -0.06 |
| COPD | 7 (12.3) | 6 (6.2) | .21 | 7 (12.3) | 1 (1.8) | .36 |
| Peripheral vascular disease | 3 (5.3) | 4 (4.1) | .05 | 3 (5.3) | 0 | .24 |
| Mobility abnormalities | 7 (12.3) | 6 (6.2) | .21 | 7 (12.3) | 3 (5.3) | .24 |
| Critical preoperative status | 3 (5.3) | 21 (21.7) | -0.50 | 3 (5.3) | 3 (5.3) | 0 |
| NYHA | ||||||
| I | 3 (5.3) | 5 (5.2) | 3 (5.3) | 3 (5.3) | ||
| II | 5 (8.8) | 34 (35.4) | -0.67 | 5 (8.8) | 6 (10.5) | -0.04 |
| III | 36 (63.2) | 51 (53.1) | .20 | 36 (63.2) | 32 (56.1) | 0.14 |
| IV | 13 (22.8) | 7 (7.2) | .48 | 13 (22.8) | 16 (28.1) | -0.15 |
| Angina IV CCS | 4 (7) | 18 (18.6) | -0.35 | 4 (7) | 1 (1.8) | .15 |
| Left ventricular function, % | 60 (49-62) | 60 (50-63) | -0.14 | 60 (49-62) | 51 (50-60) | .16 |
| Urgent surgery | 8 (14) | 32 (33) | -0.46 | 8 (14) | 6 (10.5) | .08 |
| PASP, mmHg | 38.51 | 36.83 | .12 | 38.51 | 38.91 | -0.02 |
| EuroSCORE II | 8.34 | 13.01 | -0.41 | 8.34 | 11.14 | -0.25 |
| Degenerated prosthesis | TAVI | Surgery | TAVI | Surgery | ||
| Sorin Mitroflow | 57 (100) | 62 (63.9) | 57 (100) | 45 (80) | ||
| St Jude Epic | 18 (18.6) | 4 (7) | ||||
| St Jude Biocor | 4 (4.1) | 4 (7) | ||||
| Edwards Perimount | 1 (1.03) | 2 (3.51) | ||||
| Sorin Perceval | 1 (1.03) | |||||
| Medtronic Mosaic | 3 (3.1) | 2 (3.51) | ||||
| Toronto stentless | 8 (8.2) | |||||
| Implanted prosthesis | TAVI | Surgery | TAVI | Surgery | ||
| Medtronic Core-Valve | 11 (19.3) | 11 (19.3) | ||||
| Medtronic Evolut | 46 (80.7) | 46 (80.7) | ||||
| St Jude Trifecta | 27 (17.5) | 21 (36.8) | ||||
| Sorin Mitroflow | 18 (11.7) | 15 (26.3) | ||||
| St Jude Regent | 28 (18.2) | 9 (15.8) | ||||
| Carbomedics Top Hat | 15 (9.74) | 8 (14) | ||||
| Medtronic ATS | 2 (1.3) | 1 (1.75) | ||||
| Edwards Magna | 5 (3.3) | 1 (1.75) | ||||
| Edwards Perimount | 1 (0.7) | 1 (1.75) | ||||
| Carbomedics | 1 (0.7) | 1 (1.75) | ||||
CCS, Canadian Cardiovascular Society; COPD, chronic obstructive pulmonary disease; NYHA, New York Heart Association functional class; PASP, pulmonary artery systolic pressure; SMD, standardized mean difference; TAVI, transcatheter aortic valve implantation.
Note: The table shows baseline variables, EuroSCORE II, and the type of implanted prostheses, as well as the raw data and data after propensity score matching. Unless otherwise indicated, values are expressed as n (%) or median [interquartile range].
After 57 matched pairs were created, in-hospital mortality from surgery and TAVI were 2 (3.5%) and 4 (7%), respectively, with no significant difference (P=0.68). Median follow-up was 33.9 [6.5-50.7] months and there were no losses. The Figure 1 shows the Kaplan-Meier survival curves. Survival in the surgery group vs the TAVI group at 1, 3, and 5 years was 77.2% (95% confidence interval [95%CI] 64.0%-86.1%), 77.2% (95%CI, 64.0%-86.1%), and 67.5% (95%CI, 51.45-79.3%) vs 94.6% (95%CI, 84.1%-98.2%), 79.9% (95%CI, 57.9%-91.3%), and 74.5% (95%CI, 50.9%-87.9%), respectively. As shown in the Figure 1, the log-rank test did not reach significance for survival (P=.0.25) or for the combined objective (P=.0.67).
The study included a total of 114 matched patients who underwent TAVI or surgery for degenerated bioprosthetic aortic valves. To the best of our knowledge, this series of high-risk patients is the largest comparative series with the longest follow-up time published to date.
The superposition of the confidence intervals shows that the survival curves in both groups are comparable. At 3 and 5 years of follow-up, survival rates approach 80% and 70%, respectively. These results are similar to those of Ejiofor et al.3 who recently compared the 3-year survival of 22 matched pairs. The authors of that retrospective study suggested that hospital mortality was similar and that the survival rate was slightly more than 75% in both groups at 3 years.
Around 70% to 90% of patients with degenerated biological prostheses do not undergo reoperation and this degeneration increases the risk of death by 4.5.4 This study shows that TAVI achieves at least the same 5-year survival rate as surgery and could reduce the percentage of patients with nonintervened degenerated bioprosthetic valves who die.
The main limitation of this study is the sample size, which made it difficult to achieve perfect matching and showed standardized mean differences of more than 10%. Other potentially relevant variables, such as the presence of coronary artery disease, the number of vessels, and the number of aortocoronary grafts, could not even be included in the creation of the PSs, despite the differences between the 2 groups. In addition, this study is an observational single-center retrospective study and was therefore subject to the possible biases and limitations inherent to this methodological design. However, given that it is the largest comparative series published to date, it can be considered to be a pilot study and a hypothesis generator.
Therefore, in the absence of multicenter studies with large sample sizes, the present series suggests that the 5-year survival rate could be the same in both groups.
CONFLICTS OF INTERESTC. Moris is proctor for Medtronic.