Percutaneous coronary intervention (PCI) is the treatment of choice for ST-segment elevation acute myocardial infarction (STEMI). The main aim of PCI is to reduce infarct size. Despite the development and widespread use of this procedure, as well as the optimization of intervention times and of antithrombotic therapy, the 30-day mortality of patients with STEMI in Spain is about 8%.1
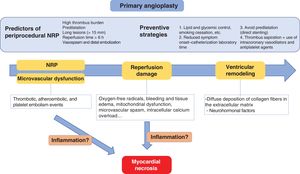
The size of the infarct depends on the area perfused by the occluded coronary artery (area at risk), the duration of the hypoperfusion, the myocardial metabolic demand, and the residual intracoronary flow after angioplasty.2 Accordingly, epicardial revascularization is not synonymous with myocardial reperfusion. Recanalization of an epicardial coronary artery is associated with a secondary deterioration of the coronary microcirculation via mechanisms such as endothelial edema, luminal obstruction, interstitial hemorrhage, and distal embolization3 (figure 1). This microvascular damage contributes to the absence of reperfusion (no-reflow phenomenon [NRP]), which is defined as the ineffective reperfusion of a previously ischemic region after recanalization of the culprit artery. Angiographically, NRP is characterized by reduced anterograde coronary flow (defined as a Thrombolysis In Myocardial Infarction [TIMI] flow ≤ 2) in the absence of mechanical obstruction or as a myocardial blush grade (MBG) between 0 and 1.4 The incidence of NRP in patients with STEMI varies between 5% and 50% and depends on the angiographic assessment method used.5 NRP can counteract the benefits of PCI on acute myocardial infarction by favoring the onset of in-hospital complications and worsening the postdischarge prognosis.6
Predictors and preventive strategies for no-reflow phenomenon (NRP) in primary angioplasty, as well as the main mechanisms involved in the acute myocardial injury and converging on myocardial necrosis and adverse ventricular remodeling. Modified with permission from Fordyce et al.3.
To improve outcomes, various strategies have been developed and analyzed in recent decades to boost coronary flow after recanalization of the culprit artery. The thrombus aspiration technique reduces the incidence of NRP but its medium- to long-term benefit, in terms of outcome, could not be confirmed in large randomized trials, such as TASTE7 and TOTAL.8 In addition, the technique has been linked to a slight, although nonsignificant, increase in the risk of stroke.9 Moreover, in the TASTE and TOTAL trials, subgroup analysis failed to show a clear benefit of manual thrombus aspiration in patients with high thrombus burden. Similar results have been seen with the combined use of thrombus aspiration and intracoronary antithrombotic agents. In the INFUSE-AMI clinical trial, intracoronary administration of abciximab (a glycoprotein IIb/IIIa inhibitor) was associated with a decrease in 30-day infarct size vs patients treated with thrombus aspiration alone, although the results did not translate into a reduction in major adverse cardiovascular events (MACE) during follow-up in any of the treatment groups.10 However, in a composite analysis of 11 clinical trials, the combination of thrombus aspiration with intracoronary abciximab was associated with a significant reduction in infarct size, as well as a decrease in MACE at 1 year of follow-up.11 This possible beneficial effect appears to depend on the intracoronary administration of the antithrombotic drug and was diluted with intravenous administration.12 Finally, there is contradictory evidence regarding the benefit of vasodilators such as adenosine, verapamil, and intracoronary nitroprusside in the prevention and treatment of NRP, particularly regarding their clinical impact.13,14 In a study by Nazir et al.,15 sodium nitroprusside and adenosine were not associated with a reduction in infarct size or a significant improvement in coronary microcirculation estimated using cardiac magnetic resonance imaging; adenosine was even linked to a higher rate of adverse effects (particularly hypotension and symptomatic bradycardia).
Given all of the above, clinical practice guidelines do not recommend the systematic use of thrombus aspiration and/or the intracoronary injection of vasodilators and antithrombotic agents in patients undergoing emergency PCI in the context of a STEMI in an attempt to prevent NRP. However, although there is no solid scientific evidence, these drugs could be used as a rescue strategy in situations in which the initial response is unsatisfactory or in the presence of intraprocedural complications (class IIb recommendation, level of evidence C).16
In a highly pertinent study recently published in Revista Española de Cardiología, Hamza and Elgendy17 analyzed the impact of a strategy based on thrombus aspiration followed by the distal intracoronary injection of eptifibatide (a glycoprotein IIb/IIIa inhibitor) and intracoronary vasodilators (verapamil and nitroglycerin). The comparison group underwent manual thrombus aspiration alone. The study involved a multicenter clinical trial that block-randomized 413 patients enrolled between December 2016 and May 2019; all patients had diabetes mellitus and had been treated with emergency PCI in the context of a STEMI with onset <12hours previously and with a high thrombus burden (TIMI ≥ 3). Balloon predilatation was permitted in patients with ineffective thrombus aspiration, depending on operator criteria. The primary endpoint was analysis of the angiographic outcome via parameters such as MBG, postprocedural TIMI flow, and corrected TIMI frame count. As a secondary endpoint, MACE was analyzed at 6 months of follow-up. In addition, an echocardiographic study was performed at discharge and at the end of follow-up to assess changes in left ventricular ejection fraction (LVEF). Two treatment groups were obtained, which were well-balanced in terms of not only epidemiological and clinical factors, but also anatomical factors, such as the presence of multivessel disease, and procedural factors, such as symptom-to-balloon time. The authors determined that the group receiving eptifibatide and intracoronary vasodilators, in addition to thrombus aspiration, obtained significantly better results in all primary angiographic objectives. These results are in line with other favorable observations in the intervention group, such as improved in-hospital and 6-month LVEF, as well as a lower positivity, in absolute numbers, of creatine kinase-MB (CK-MB) and a lower time to reach peak CK-MB. The prognostic impact of both strategies, from a clinical perspective, was analyzed as a secondary endpoint. No significant differences were found between the 2 groups in terms of MACE during the first 6 months of follow-up.
The study17 has a number of limitations deserving mention. First, one of the seeds for the study lies in the greater bioavailability and effectiveness of antithrombotic agents and vasodilators after their administration via the thrombus aspiration catheter, distal to the culprit artery, compared with their intracoronary administration via a guide catheter, where a large amount of the drug will be washed through the epicardial coronary flow to nonculprit vessels. In this regard, it is important to note that this clinical trial was not placebo controlled. The observed differences in the MBG, corrected frame count, and TIMI flow could have been influenced by the differences in the time from thrombus aspiration to angiographic assessment in the 2 groups. Second, the authors partly explain the neutral impact of the intervention strategy on clinical events by the small sample size and short follow-up period. However, it is striking that no differences were found in the normalization of the ST-segment between the 2 treatment groups. In patients with STEMI, ST-segment normalization after reperfusion is a parameter strongly linked to effective reperfusion, the myocardial area at risk, and the myocardial salvage index estimated using cardiac magnetic resonance imaging.2 In addition, a persistently elevated ST-segment has been associated with worse prognosis during follow-up.18 However, the long ischemia times reported in the 2 groups could have contributed to these findings. Another factor with a strong inverse relationship with effective reperfusion is adverse left ventricular remodeling.19 In this regard, the results of this study did show an LVEF improvement during hospitalization and follow-up; however, the LVEF was assessed at the end of follow-up, after analysis of the clinical outcomes (MACE). Finally, due to the study design, it was not possible to establish if the improved angiographic data were due to the combination of the glycoprotein IIb/IIIa inhibitors and vasodilators or if the effect depended on 1 of the 2 treatments alone.
In summary, there is insufficient evidence to support the systematic use of thrombus aspiration combined with antithrombotic agents and/or vasodilators as a preventive treatment for NRP in the context of STEMI. Although most of the available studies suggest an improvement in immediate angiographic parameters, the results are predominantly negative regarding their effectiveness in the improvement of indirect data related to effective reperfusion, as well as the reduction in MACE during follow-up. The work by Hamza and Elgendy provides new evidence indicating a beneficial effect of this treatment approach in a specific population, namely, diabetic patients, who are characterized by greater platelet reactivity, worse microvascular function, and, therefore, greater thrombus burden and higher rates of NRP. Nonetheless, there is a need for new clinical trials with a larger sample size and longer follow-up that evaluate the prognostic impact of a combination of these strategies in both diabetic patients and other high-risk populations.
FUNDINGThis work has not received funding.
CONFLICTS OF INTERESTThe authors have no conflicts of interest.