In current clinical practice, only a small percentage of patients with acute coronary syndrome are treated conservatively (receiving neither coronary angiography nor fibrinolysis). Evidence-based clinical practice guidelines1 recommend that patients suffering an acute myocardial infarction (AMI) undergo invasive intervention, in addition to medical treatment of proven prognostic efficacy; this invasive treatment should take the form of emergent reperfusion therapy for ST segment elevation myocardial infarction (STEMI) and early coronary angiography for non-ST segment elevation myocardial infarction (NSTEMI). Certain clinical situations accompanying acute coronary syndrome exclude patients from this intensive management strategy. The typical clinical profile in such cases is that of a fragile elderly patient with anemia and renal failure or other important comorbidities that justify conservative management.
Here we present an analysis of in-hospital and long-term mortality among AMI patients in our population who were assigned to conservative treatment by the on-duty physician. The aim was to identify variables that predict poor prognosis in these patients.
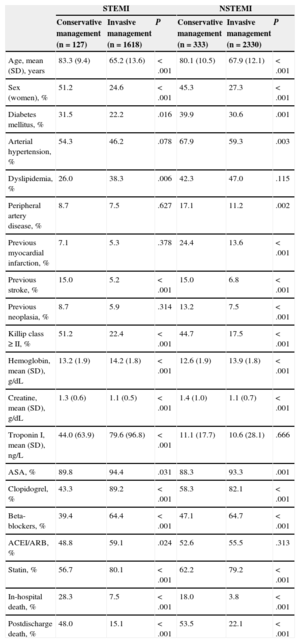
We analyzed the records of 4408 patients consecutively admitted to our hospital between 2003 and 2012 with a diagnosis of AMI (1745 with STEMI and 2663 with NSTEMI). Of these patients, 460 received conservative medical treatment (127 [7.3%] with STEMI and 333 [12.5%] with NSTEMI); 84 STEMI patients presented > 24hours after symptom onset. Among the total group of STEMI patients, 54 (3.1%) received fibrinolytic treatment and all were later examined by angiography. Patients assigned to conservative management tended to be older, and this group included a higher percentage of women and patients with diabetes mellitus, had a worse Killip class, and had lower hemoglobin and higher creatinine readings (Table). All of this, as is well known, implies a poor prognosis for patients receiving conservative medical treatment.1
Basal Characteristics of Patients Hospitalized for STEMI and NSTEMI, Stratified According to Treatment Received Cconservative vs Invasive Management)
| STEMI | NSTEMI | |||||
|---|---|---|---|---|---|---|
| Conservative management (n = 127) | Invasive management (n = 1618) | P | Conservative management (n = 333) | Invasive management (n = 2330) | P | |
| Age, mean (SD), years | 83.3 (9.4) | 65.2 (13.6) | < .001 | 80.1 (10.5) | 67.9 (12.1) | < .001 |
| Sex (women), % | 51.2 | 24.6 | < .001 | 45.3 | 27.3 | < .001 |
| Diabetes mellitus, % | 31.5 | 22.2 | .016 | 39.9 | 30.6 | .001 |
| Arterial hypertension, % | 54.3 | 46.2 | .078 | 67.9 | 59.3 | .003 |
| Dyslipidemia, % | 26.0 | 38.3 | .006 | 42.3 | 47.0 | .115 |
| Peripheral artery disease, % | 8.7 | 7.5 | .627 | 17.1 | 11.2 | .002 |
| Previous myocardial infarction, % | 7.1 | 5.3 | .378 | 24.4 | 13.6 | < .001 |
| Previous stroke, % | 15.0 | 5.2 | < .001 | 15.0 | 6.8 | < .001 |
| Previous neoplasia, % | 8.7 | 5.9 | .314 | 13.2 | 7.5 | < .001 |
| Killip class ≥ II, % | 51.2 | 22.4 | < .001 | 44.7 | 17.5 | < .001 |
| Hemoglobin, mean (SD), g/dL | 13.2 (1.9) | 14.2 (1.8) | < .001 | 12.6 (1.9) | 13.9 (1.8) | < .001 |
| Creatine, mean (SD), g/dL | 1.3 (0.6) | 1.1 (0.5) | < .001 | 1.4 (1.0) | 1.1 (0.7) | < .001 |
| Troponin I, mean (SD), ng/L | 44.0 (63.9) | 79.6 (96.8) | < .001 | 11.1 (17.7) | 10.6 (28.1) | .666 |
| ASA, % | 89.8 | 94.4 | .031 | 88.3 | 93.3 | .001 |
| Clopidogrel, % | 43.3 | 89.2 | < .001 | 58.3 | 82.1 | < .001 |
| Beta-blockers, % | 39.4 | 64.4 | < .001 | 47.1 | 64.7 | < .001 |
| ACEI/ARB, % | 48.8 | 59.1 | .024 | 52.6 | 55.5 | .313 |
| Statin, % | 56.7 | 80.1 | < .001 | 62.2 | 79.2 | < .001 |
| In-hospital death, % | 28.3 | 7.5 | < .001 | 18.0 | 3.8 | < .001 |
| Postdischarge death, % | 48.0 | 15.1 | < .001 | 53.5 | 22.1 | < .001 |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ASA, acetylsalicylic acid; NSTEMI: non-ST segment elevation myocardial infarction; STEMI: ST segment elevation myocardial infarction.
Among patients receiving conservative treatment, we analyzed variables associated with a worse prognosis during in-hospital care and long-term follow-up; in-hospital and long-term mortality were analyzed independently in the two types of AMI by multivariate analysis (binary logistic regression for in-hospital mortality and Cox regression for long-term mortality), with adjustments for first-order interactions between covariates.
Among NSTEMI patients, univariate analysis indicated an association of high in-hospital mortality with diabetes mellitus (odds ratio [OR] = 1.79; 95% confidence interval [95%CI], 1.02-3.14; P = .042), Killip class ≥ II (OR = 6.81; 95%CI, 3.46-13.43; P < .001), hemoglobin (OR = 0.85; 95%CI, 0.73-0.98; P = .027), creatinine (OR = 1.49; 95%CI, 1.17-1.90; P = .001) and troponin (OR = 1.02; 95%CI, 1.01-1.04; P = .001). In-hospital mortality in these patients was also associated with nontreatment with beta-blockers (OR = 0.19; 95%CI, 0.09-0.39; P < .001), angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers (OR = 0.35; 95%CI, 0.19-0.63; P < .001), or statins (OR = 0.23; 95%CI, 0.16-0.32; P < .001). In the multivariate analysis, only Killip class ≥ II persisted as an independent predictor of in-hospital mortality (OR = 4.5; 95%CI, 2.13-9.53; P < .001).
Long-term mortality in NSTEMI patients (4.2 ± 2.8 years) was positively associated with the following variables: age (hazard ratio [HR] = 1.06; 95%CI, 1.04-1.08; P < .001), peripheral artery disease (HR = 1.70; 95%CI, 1.18-2.46; P = .005), previous AMI (HR = 1.46; 95%CI, 1.06-2.02; P = .022), Killip class ≥ II (HR = 2.43, 95%CI, 1.79-3.28; P < .001), hemoglobin (HR = 0.88; 95%CI, 0.81-0.95; P = .001), creatinine (HR = 1.27; 95%CI, 1.13-1.44; P < .001), and troponin (HR = 1.01; 95%CI, 1.01-1.02; P < .001). Indicators of good prognosis were treatments with beta-blockers (HR = 0.50; 95%CI, 0.37-0.68; P < .001) and statins (HR = 0.55; 95%CI, 0.47-0.66; P < .001). After the multivariate analysis, the following persisted as independent predictors of mortality: age (HR = 1.06; 95%CI, 1.03-1.09; P < .001), peripheral artery disease (HR = 1.71; 95%CI, 1.06-2.76; P = .028), previous AMI (HR = 1.76; 95%CI, 1.15-2.71; P = .009), Killip class ≥ II (HR = 1.59; 95%CI, 1.05-2.41; P = .028), hemoglobin (HR = 0.87; 95%CI, 0.77-0.98; P = .020), creatinine (HR = 1.38; 95%CI, 1.07-1.77; P = .013), and nontreatment with statins (HR = 0.79; 95%CI, 0.62-0.99; P = .042).
Among patients with STEMI, univariate analysis showed association of high in-hospital mortality with Killip class ≥ II (OR = 8.00; 95%CI, 3.02-21.17; P < .001), creatinine (OR = 1.72; 95%CI, 0.97-3.05; p = .062), and troponin (OR = 1.01; 95%CI, 0.99-1.02; P = .079). Indicators of good prognosis were treatments with beta-blockers (OR = .21; 95%CI, 0.08-0.56; P = .002), angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers OR = 0.19; 95%CI, 0.08-0.48; P < .001), and statins (OR = 0.15; 95%CI, 0.06-0.36; P < .001). In the multivariable analysis, the only independent predictors of in-hospital mortality were Killip class ≥ II (OR = 5.22; 95%CI, 1.44-18.86; P = .012) and treatment with statins (OR = 0.79; 95%CI, 0.06-0.63; P = .006).
Long-term mortality of STEMI patients was associated with age (HR = 1.09; 95%CI, 1.04-1.15; P = .001), hemoglobin (HR = 0.86; 95%CI, 0.76-0.97; P = .015), and creatinine (HR = 1.72; 95%CI, 1.18-2.49; P = .004). After multivariate analysis, only age persisted as an independent mortality predictor (HR = 1.09; 95%CI, 1.04-1.15; p = .001).
For in-hospital mortality, we conducted a sensitivity analysis, eliminating patients who died during the first 48 hours (68 with STEMI and 18 with NSTEMI, out of 307 in-hosptial deaths). Killip class ≥ II remained as an independent mortality predictor in both the NSTEMI group (OR = 7.41; 95%CI, 4.82-11.39; P < .001) and the STEMI group (OR = 10.58; 95%CI, 6,26-17,89; P < .001), and statins treatment persisted as a predictor of good prognosis in the STEMI group (OR = 0.19; 95%CI, 0.12-0.32; p < .001).
Our results clearly show that patients under conservative management have a higher basal risk than those treated invasively, which could justify invasive therapy. Of the variables analyzed, the only independent predictor of in-hospital mortality in the 2 infarction groups is Killip class ≥ II, an indicator of major clinical and hemodynamic instability. Notably, age is not a predictor of in-hospital mortality in either of the AMI groups, but is a predictor of mortality risk during follow-up. The influence of age on the treatment of acute coronary syndrome was analyzed in the MINAP registry, which showed that the use of invasive treatment was less frequent in older patients, despite demonstrated mortality reductions with this approach in all age groups.2
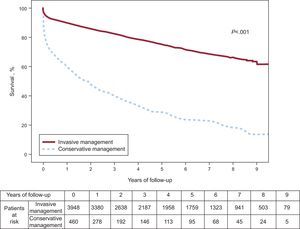
In conclusion, in daily clinical practice it is common to encounter patients with AMI who are treated conservatively, without coronary angiography (approximately 1 in 10). These patients have a poor cardiovascular risk profile and a dismal prognosis (Figure), with mortality exceeding 20% during hospital care and approaching 50% during postdischarge follow-up. Killip class is the only predictor of mortality during hospitalization, and age is the variable most strongly associated with mortality during follow-up.