Left atrial (LA) aneurysmal dilation is often associated with rheumatic valve disease.1 Our objective was to define the actual incidence of nonvalvular aneurysmal dilation of the LA and the clinical and echocardiographic characteristics of patients with this condition.
Aneurysmal dilation was defined as an anteroposterior LA diameter of more than 6cm, measured in M-mode from the parasternal view. Echocardiographic studies recorded during 2010 and 2011 were reviewed. Patients with mitral valve prosthesis, mitral stenosis, or mitral regurgitation of more than mild severity and pericardial constriction were excluded. Patients were then classified in 1 of 2 groups: patients with LA aneurysmal dilation with diastolic dysfunction (ADDD) and those with isolated aneurysmal dilation (IAD). Diastolic dysfunction was defined as an e’ velocity of less than 8cm/s at the septal mitral annulus.2
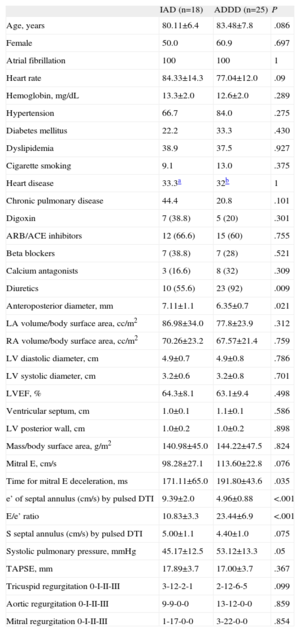
The echocardiographic parameters recorded (see Table) were as follows: anteroposterior LA diameter and indexed volume according to the Simpson rule (apical 4-chamber 2-chamber view), right atrial volume, left ventricular systolic and diastolic function, e’ and S velocities at the septal mitral annulus, pulmonary pressure, tricuspid annular plane systolic excursion, and severity of regurgitation. In each case, the mean of 5 measurements was taken.
Clinical and Echocardiographic Characteristics of Patients With Isolated Aneurysmal Dilation and Aneurysmal Dilation With Diastolic Dysfunction of the Atrium
| IAD (n=18) | ADDD (n=25) | P | |
| Age, years | 80.11±6.4 | 83.48±7.8 | .086 |
| Female | 50.0 | 60.9 | .697 |
| Atrial fibrillation | 100 | 100 | 1 |
| Heart rate | 84.33±14.3 | 77.04±12.0 | .09 |
| Hemoglobin, mg/dL | 13.3±2.0 | 12.6±2.0 | .289 |
| Hypertension | 66.7 | 84.0 | .275 |
| Diabetes mellitus | 22.2 | 33.3 | .430 |
| Dyslipidemia | 38.9 | 37.5 | .927 |
| Cigarette smoking | 9.1 | 13.0 | .375 |
| Heart disease | 33.3a | 32b | 1 |
| Chronic pulmonary disease | 44.4 | 20.8 | .101 |
| Digoxin | 7 (38.8) | 5 (20) | .301 |
| ARB/ACE inhibitors | 12 (66.6) | 15 (60) | .755 |
| Beta blockers | 7 (38.8) | 7 (28) | .521 |
| Calcium antagonists | 3 (16.6) | 8 (32) | .309 |
| Diuretics | 10 (55.6) | 23 (92) | .009 |
| Anteroposterior diameter, mm | 7.11±1.1 | 6.35±0.7 | .021 |
| LA volume/body surface area, cc/m2 | 86.98±34.0 | 77.8±23.9 | .312 |
| RA volume/body surface area, cc/m2 | 70.26±23.2 | 67.57±21.4 | .759 |
| LV diastolic diameter, cm | 4.9±0.7 | 4.9±0.8 | .786 |
| LV systolic diameter, cm | 3.2±0.6 | 3.2±0.8 | .701 |
| LVEF, % | 64.3±8.1 | 63.1±9.4 | .498 |
| Ventricular septum, cm | 1.0±0.1 | 1.1±0.1 | .586 |
| LV posterior wall, cm | 1.0±0.2 | 1.0±0.2 | .898 |
| Mass/body surface area, g/m2 | 140.98±45.0 | 144.22±47.5 | .824 |
| Mitral E, cm/s | 98.28±27.1 | 113.60±22.8 | .076 |
| Time for mitral E deceleration, ms | 171.11±65.0 | 191.80±43.6 | .035 |
| e’ of septal annulus (cm/s) by pulsed DTI | 9.39±2.0 | 4.96±0.88 | <.001 |
| E/e’ ratio | 10.83±3.3 | 23.44±6.9 | <.001 |
| S septal annulus (cm/s) by pulsed DTI | 5.00±1.1 | 4.40±1.0 | .075 |
| Systolic pulmonary pressure, mmHg | 45.17±12.5 | 53.12±13.3 | .05 |
| TAPSE, mm | 17.89±3.7 | 17.00±3.7 | .367 |
| Tricuspid regurgitation 0-I-II-III | 3-12-2-1 | 2-12-6-5 | .099 |
| Aortic regurgitation 0-I-II-III | 9-9-0-0 | 13-12-0-0 | .859 |
| Mitral regurgitation 0-I-II-III | 1-17-0-0 | 3-22-0-0 | .854 |
ACE, angiotensin converting enzyme; ADDD, aneurysmal dilation with diastolic dysfunction; AoE, aortic stenosis; ARB, angiotensin receptor blocker; AS, (operated) atrial shunt; Cor P, cor pulmonale; DCM, dilated cardiomyopathy; DTI, Doppler tissue imaging; HCM, hypertrophic cardiomyopathy; IAD, isolated aneurysmal dilation; IHD, ischemic heart disease; LA, left atrium; LV, left ventricular; LVEF, left ventricular ejection fraction; RA, right atrium; TAPSE, tricuspid annular plane systolic excursion.
Data expressed as percentage, no. (%), or mean±SD unless otherwise indicated. Continuous variables, Mann-Whitney U test; categorical variables, χ2 test; ordinal variables, Fisher exact test and Mantel-Haenszel test. Statistical comparisons are bilateral (statistical package SPSS v17).
The clinical parameters recorded were age, sex, cardiac rhythm, smoking habit, diabetes mellitus, dyslipidemia, hemoglobin in blood, hypertension, chronic pulmonary disease, heart disease, functional class, and history of admission for heart failure.
Of 22 555 echocardiograms (Figure), 644 had LA >6.0cm; 116 (18%) did not have any significant mitral valve lesions, and mitral valve prostheses were found in 43%, stenosis in 22%, mitral regurgitation in 9.3%, and annular calcification with hemodynamic impact in 6.8%. Eighty per cent of the patients without valve disease were in atrial fibrillation (AF). Twenty patients (17.2%) had e’ >8cm/s and 18 were in AF; these patients comprised the IAD group. Ninety-six patients (82.8%) had e’ <8cm/s, 82 of whom were in AF. Twenty-five of these age-matched patients comprised the ADDD group.
Apical, 4-chamber echocardiogram showing mitral filling and Doppler tissue imaging of the septal mitral annulus of a patient in the group of isolated aneurysmal dilation in the left atrium (left panel). Echocardiograms of the isolated aneurysmal dilation group (center) and aneurysmal dilation with diastolic dysfunction (right). ADDD, aneurysmal dilation with diastolic dysfunction; IAD, isolated aneurysmal dilation.
The clinical differences between the IAD and ADDD groups were not significant (Table). Likewise, there were no differences in diameter, wall thickness, and ejection fraction. The anteroposterior LA diameter was greater in the IAD group, although the volume was similar. Patients in the IAD group had an e’ wave velocity greater than expected for their age (9.39cm/s) and greater than the e’ wave velocity for the ADDD group. The E velocity and E/e’ ratio in the IAD group were lower than those of the ADDD group. An E/e’ ratio >15 was found less often in the IAD group (16.6% vs 92%). Systolic pulmonary pressure was lower in the IAD group. Within this group, patients without chronic pulmonary disease (66.6%) had a lower systolic pulmonary pressure (36 vs 58mmHg; P<.001) and greater tricuspid annular plane systolic excursion.
In the IAD group, a history of heart failure was less frequent (33% vs 75%; P=.007), patients had a better functional status (69% vs 36% with functional class
Although most atrial aneurysms continue to present in patients with mitral valve disease, 18% appear in patients without significant valve disease. Atrial fibrillation, present in 80% of the patients, accounts in part for the atrial dilation. Although no information is available on the duration of AF, given the age of the patients the condition was likely to have been long-standing.
According to the guidelines, increased atrial volume without valve disease reflects diastolic dysfunction, raised pressures,2 poor clinical condition, and poor prognosis.3 This did not occur in 17% of our patients with nonvalvular dilation. According to the guidelines, patients with atrial dilation and e’ >8cm/s are athletes or have pericardial constriction, neither of which were applicable in our patients. Atrial remodeling without any increase in atrial pressure could be one explanation.4 Another possibility is a paradoxical behavior of e’ in the presence of diastolic dysfunction.
The similar incidences of risk factors, heart disease, and even a decreased annulus S velocity in the 2 groups indicates that there is a certain degree of myocardial involvement in both groups. It may be that the patients in the IAD group have a pseudonormal e’ wave pattern associated with AF with aneurysmal dilation. When the atrium does not contract, the entire annular movement occurs during protodiastole, and could be quicker due to the large atrial dilation. Moreover, with a more dilated LA, larger loads are possible without increasing the pressure and so clinical manifestations are more limited. In any case, patients with IAD should have better diastolic function and lower pressure as their functional class and therapeutic requirements are markedly lower and they have less history of heart failure. In fact, in this group, only patients with chronic pulmonary disease showed clinical deterioration.
This study is limited in that it was retrospective and had no invasive measurements. The definition of atrial aneurysm is arbitrary. Other studies have used the term giant left atrium. It would have been better to use the atrial volume, but the coding meant that such an analysis was impossible. Several patients had mild mitral regurgitation, which could be relevant if the severity increased with exercise.
Atrial aneurysmal dilation is not always associated with mitral valve disease. It can be associated with AF and old age, often in patients with diastolic dysfunction in a poor clinical state. Some elderly patients with atrial aneurysm have a good functional status and normal pulmonary pressure; they can be identified by a paradoxically elevated e’ wave. In view of the tendency for rheumatic heart disease to disappear and given the aging of the population, nonvalvular atrial aneurysmal dilation will become increasingly common.
We thank Dr S. Ruiz Leria, Dr A. Megías Saez, and Dr A. García Martin, of the cardiology department, and Alfonso Muriel, of the biostatistics department of the Hospital Ramón y Cajal, Madrid.