Angiography, the primary imaging method for coronary artery disease assessment, has well-established limitations. These limitations stem from its provision of biplanar projections of the 3-dimensional coronary tree, presenting a lumenogram rather than the vessel wall where atherosclerosis is located. In contrast, intravascular imaging (IVI), such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), allows for cross-sectional tomographic imaging of the coronary artery, offering complementary information to angiography.1
Stone et al.2 recently presented the results of an updated network meta-analysis merging data from the recent ILUMIEN IV and OCTOBER trials with prior studies.3-4 The objective was to investigate the effects of IVI-guidance vs angiography-guidance in percutaneous coronary intervention (PCI) procedures. All comparisons indicated that the use of IVI, whether OCT or IVUS, led to enhanced stent implantation, reduced complications, and lower stent thrombosis rates compared with angiography-guidance.
Guidelines from the European Society of Cardiology and the American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography (ACC/AHA/SCAI) recommend considering IVUS or OCT in selected patients to optimize stent implantation in various scenarios.5,6 However, the comparative effectiveness of these 2 contemporary imaging strategies for PCI guidance remains unclear. In this regard, the study conducted by Stone et al., which evaluated data from 4 different trials (ILUMIEN III, iSIGHT, MISTIC-1, and OPINION) involving a total of 1316 patients comparing IVUS vs OCT, demonstrated the noninferiority of OCT to IVUS in guiding PCI.7-8 This concept gained further support from the OCTIVUS study (not included in the meta-analysis), which excluded patients with acute ST-segment elevation myocardial infarction (non–ST-segment elevation myocardial infarctioin and unstable angina were included).9
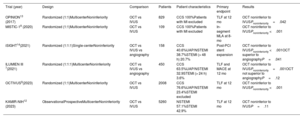
Despite evidence supporting the use of IVI to optimize PCI procedures, there is limited evidence comparing the results of OCT vs IVUS in patients with acute myocardial infarction (MI), including those with ST-segment elevation.4,10-11 This population has been systematically excluded from most registries and trials (table 1). To address this gap, in a recent article published in Revista Española de Cardiología, Lee et al.12 conducted a retrospective analysis using data from the Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH) to compare OCT and IVUS in guiding PCI procedures among patients with MI.
IVUS versus OCT comparison studies
| Trial (year) | Design | Comparison | Patients | Patient characteristics | Primary endpoint | Results |
|---|---|---|---|---|---|---|
| OPINION13 (2017) | Randomized (1:1)MulticenterNoninferiority | OCT vs IVUS | 829 | CCS 100%Patients with MI excluded | TLF at 12 mo | OCT noninferior to IVUSPnoninferiority=.042 |
| MISTIC-18 (2020) | Randomized (1:1)MulticenterNoninferiority | OCT vs IVUS | 109 | CCS 100%Patients with MI excluded | In-segment MLA at 8-mo | OCT noninferior to IVUSPnoninferiority <.001 |
| iSIGHT14(2021) | Randomized (1:1:1)Single-centerNoninferiority | OCT vs IVUS vs angiography | 158 | CCS 40.6%UAP/NSTEMI 38.7%STEMI (> 48 h) 20.7% | Post-PCI stent expansion | OCT noninferior to IVUSPnoninferiority <.001OCT superior to angiographyP=.041 |
| ILUMIEN III 7(2021) | Randomized (1:1:1)MulticenterNoninferiority | OCT vs IVUS vs angiography | 450 | CCS 63.5%UAP/NSTEMI 32.9STEMI (> 24 h) 3.6% | TLF and MACE at 12 mo | OCT noninferior to IVUSPnoninferiority=.001OCT not superior to angiographyP=.12 |
| OCTIVUS9(2023) | Randomized (1:1)MulticenterNoninferiority | OCT vs IVUS | 2008 | CCS 76.6%UAP/NSTEMI 23.4%STEMI excluded | TLF at 12 mo | OCT noninferior to IVUSPnoninferiority <.001 |
| KAMIR-NIH12 (2023) | ObservationalProspectiveMulticenterNoninferiority | OCT vs IVUS | 5260 | NSTEMI 57.1%STEMI 42.9% | TLF at 12 mo | OCT noninferior to IVUSP=.11 |
CCS, chronic coronary syndrome; IVUS, intravascular ultrasound; MI, myocardial infarction; MLA, minimal lumen area; NSTEMI, non–ST-segment elevation myocardial infarction; OCT, optical coherence tomography; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction; TLF, target lesion failure; UAP, unstable angina pectoris.
The authors presented findings from the KAMIR-NIH registry involving 5260 patients with acute MI and underwent PCI with a second-generation drug-eluting stent, either under IVUS guidance (4725 patients) or OCT guidance (535 patients). The objective was to investigate the comparative efficacy of OCT and IVUS in guiding PCI procedures among MI patients, offering insights into procedural success rates, stent optimization, and post-PCI outcomes. The main finding of the present report is that there were no significant differences between PCI guided with IVUS and OCT in relation to the primary endpoint of target lesion failure (composite of cardiac death, target vessel MI, or ischemia-driven target vessel revascularization) (hazard ratio, 0.61; 95% confidence interval, 0.33-1.12; P=.11) and major adverse cardiovascular events (hazard ratio, 0.88; 95% confidence interval, 0.52-1.47, P=.61) at 12 months of OCT- compared with IVUS-guided PCI.
The authors delve into a topic of considerable interest by providing the first extensive analysis IVI use in patients with acute coronary syndrome and ST-segment elevation MI. This is noteworthy considering that existing literature has not primarily focused on or has even excluded patients with MI. However, despite the substantial number of patients involved, this registry carries certain limitations. Its retrospective and nonrandomized design restricts the ability to effectively discern whether OCT could serve as a valid alternative to IVUS in guiding PCI for MI cases. Moreover, and despite propensity score matching, there remained a considerable gap in baseline characteristics between the IVUS-guided and OCT-guided groups. This discrepancy could potentially be influenced by factors such as the younger age and fewer comorbidities observed in the OCT group. Additionally, differences in the practices among centers and operators, including their experience and the availability of each imaging technique, might significantly impact the selection of either IVUS or OCT, thereby potentially affecting the presented data.
Indeed, comparing OCT and IVUS is not straightforward, especially considering their dissimilarities and real-world practice, where OCT is notably less used than IVUS. This substantial discrepancy, with OCT accounting for less than 5% of the total treated patients in this registry, could significantly impact the final outcomes. Differences in angiographic and procedural characteristics, such as the prevalence of multivessel disease or left main disease, as well as variations in stent number and size, may be attributed to the limitations and advantages inherent in each imaging technique.
Importantly, major factors that limit the use of OCT include its costs and challenges associated with its use in patients with chronic kidney disease or left main disease. OCT assessment of aorto-ostial coronary segments is known to be challenging, due to difficulties in achieving optimal blood clearance at the coronary ostia; however, as observed in the literature as well as in this registry and in the OCTIVUS trial, the contrast medium used to perform OCT seems not to significantly affect postprocedural acute kidney injury. Furthermore, a detailed description of procedural data (procedure time, radiation, amount of contrast, pre/postdilatation) as well as comprehensive information about IVI (timing, minimal stent area, complications) is lacking. The situations when one method over the other might be more effective therefore remain unclear.
The enhanced capability of OCT in meticulously evaluating coronary artery morphology and plaque composition is particularly beneficial in these scenarios. An independent subanalysis comparing ST-segment elevation MI and non–ST-segment elevation MI cases could yield substantial insights.
CONCLUSION AND FUTURE DIRECTIONSThis study agrees with the results of prior research in the MI setting, reinforcing observations from earlier studies. It echoes the 2021 ACC/AHA/SCAI guidelines for PCI, emphasizing the equivalence of OCT to IVUS in the management of complex scenarios such as left main disease, bifurcation, and stent optimization and adds to the increasing evidence supporting the use of IVI to guide PCI. Moreover, the present work provides further support to the evolving notion of equipoise between IVUS and OCT, which both have superior results to angiography. Future research lines should consist of randomized trials, studies focusing on specific patient subsets, and long-term follow-up data to strengthen the IVI evidence supporting PCI for MI. The authors should be complimented for their present work, which significantly adds to the field.
FUNDINGThere was no external funding.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest related to the content of this manuscript.