There are no guidelines regarding the most appropriate approach for provisional side branch (SB) intervention in left main (LM) bifurcation lesions.
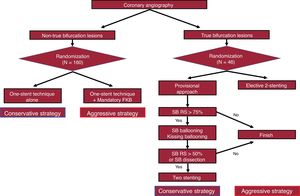
MethodsThe present prospective, randomized, open-label, multicenter trial compared conservative vs aggressive strategies for provisional SB intervention during LM bifurcation treatment. Although the trial was designed to enroll 700 patients, it was prematurely terminated due to slow enrollment. For 160 non-true bifurcation lesions, a 1-stent technique without kissing balloon inflation was applied in the conservative strategy, whereas a 1-stent technique with mandatory kissing balloon inflation was applied in the aggressive strategy. For 46 true bifurcation lesions, a stepwise approach was applied in the conservative strategy (after main vessel stenting, SB ballooning when residual stenosis> 75%; then, SB stenting if residual stenosis> 50% or there was a dissection). An elective 2-stent technique was applied in the aggressive strategy. The primary outcome was a 1-year target lesion failure (TLF) composite of cardiac death, myocardial infarction, or target lesion revascularization.
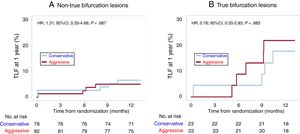
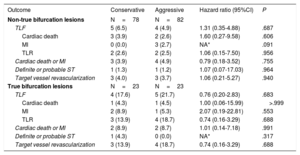
ResultsAmong non-true bifurcation lesions, the conservative strategy group used a smaller amount of contrast dye than the aggressive strategy group. There were no significant differences in 1-year TLF between the 2 strategies among non-true bifurcation lesions (6.5% vs 4.9%; HR, 1.31; 95%CI, 0.35-4.88; P=.687) and true bifurcation lesions (17.6% vs 21.7%; HR, 0.76; 95%CI, 0.20-2.83; P=.683).
ConclusionsIn patients with a LM bifurcation lesion, conservative and aggressive strategies for a provisional SB approach have similar 1-year TLF rates.
Keywords
Despite recent advances in drug-eluting stents and interventional techniques, percutaneous coronary intervention (PCI) of lesions at bifurcations remains a challenging procedure. Intervention of bifurcation lesions carries a risk of side branch (SB) closure, which can lead to periprocedural myocardial infarction and adverse clinical outcomes.1 Prior studies have investigated the optimal strategy for bifurcation lesions. The accepted standard treatment for bifurcation lesions is a simple 1-stent technique with a provisional SB approach.2–4 However, there are limited data regarding left main (LM) bifurcation lesions because most previous studies have been conducted on non-LM bifurcation lesions.
Several observational studies have found that the 1-stent strategy with a provisional SB approach obtains favorable results in LM bifurcation lesions.5–8 The SMART-STRATEGY study reported that the provisional SB approach was safe and effective in the treatment of 114 patients with a LM bifurcation lesion.9 However, given the large amount of subtended myocardium in SBs, the need for additional SB dilatation after main vessel (MV) stenting is a challenging issue. Although routine use of a final kissing balloon (FKB) after MV stenting has been discouraged in non-LM bifurcation lesions,10,11 it has not been established whether routine FKB would be beneficial in the provisional SB approach for LM bifurcation lesions.12 Therefore, we compared clinical outcomes among patients with a LM bifurcation lesion treated with conservative vs aggressive strategies for SB intervention. In doing so, we sought to determine the optimal criteria for the provisional SB approach.
METHODSStudy design and patientsThe SMART-STRATEGY II study was a prospective, randomized, open-label, multicenter trial comparing conservative vs aggressive strategies for provisional SB intervention during LM bifurcation PCI at 15 centers in Korea between March 2013 and December 2016 (ClinicalTrials.gov, NCT01798433). The study protocol was approved by the local institutional review boards. Written informed consent was obtained from all participants. Inclusion criteria were as follows: a) age ≥ 20 years; b) a LM bifurcation lesion on coronary angiography with a reference diameter of the main branch (left anterior descending artery) and SB (left circumflex artery) ≥ 2.5mm by visual estimation; c) significant myocardial ischemia in the main branch or SB diameter stenosis> 75% or 50%-75% with angina and/or objective evidence of ischemia in the noninvasive stress test; and d) patients who voluntarily signed the written informed consent form. Exclusion criteria were as follows: a) patients with coronary artery stenosis only in the SB ostium of the LM bifurcation lesion (Medina 0.0.1 lesion); b) patients with known hypersensitivity or contraindication to heparin, aspirin, clopidogrel, or biolimus; or c) patients who previously underwent stent implantation in the target lesion prior to enrollment. All of the study patients in this trial met the inclusion criteria and none of the exclusion criteria.
Patients were stratified according to whether they had a non-true bifurcation lesion (SB stenosis diameter <50%) or true bifurcation lesion (SB stenosis diameter ≥ 50%). Patients were then randomized 1:1 to a conservative or aggressive strategy group for provisional SB intervention after MV stenting (figure 1). For non-true bifurcation lesions, the conservative strategy included MV stenting alone without FKB. The aggressive strategy included MV stenting followed by mandatory FKB. For true bifurcation lesions, the conservative strategy was SB ballooning followed by kissing ballooning for an SB stenosis diameter ≥ 75% after MV stenting. SB stenting was only performed when the SB stenosis diameter was ≥ 50% or there was a SB dissection. The aggressive strategy included an elective 2-stent approach for the MV and SB. In all cases, the choice of the 2-stenting technique was made at the operator's discretion. Intravascular ultrasound use was recommended, but not mandatory. For the stent implantation, the BioMatrix stent (Biosensors Interventional Technologies Pte. Ltd, Singapore) was used except when it was clinically unavailable. After the index procedure, measurement of the myocardial band fraction of creatine kinase was mandatory.
Quantitative coronary analysis and follow-up angiographyAngiograms were obtained in the 15 participating centers using portable storage devices and sent to the core laboratory (Cardiac and Vascular Center, Samsung Medical Center, Korea). All cine coronary angiograms were reviewed and quantitatively analyzed at the Core Laboratory by 2 independent experienced staff members. Quantitative coronary analysis was performed for LM bifurcation lesions before and after the intervention using the same projections with the optimal view. Routine follow-up angiography was recommended at 9 months after the index procedure. However, the rate of follow-up angiography was 54.9% (113 out of 206 patients).
Study end points and follow-upThe primary end point was the occurrence of target lesion failure (TLF), a composite of cardiac death, myocardial infarction, or target lesion revascularization at 1 year of follow-up. The secondary end points included the individual components of the primary end point: cardiac death or myocardial infarction, stent thrombosis, and target vessel revascularization at 1 year of follow-up. All deaths were considered cardiac unless a definite noncardiac cause could be established. Myocardial infarction was defined as elevated cardiac enzymes (troponin or the myocardial band fraction of creatine kinase) greater than the upper limit of normal that occurred with ischemia symptoms or electrocardiogram findings indicative of ischemia that were unrelated to the index procedure. Procedure-related myocardial infarction was defined as an elevated myocardial band fraction of creatine kinase more than 3 times above the upper limit of normal within 48hours of the index procedure. Target lesion revascularization was defined as repeat PCI of the lesion within 5mm of stent deployment. Target vessel revascularization was defined as repeat PCI or bypass graft surgery of the target vessel. Stent thrombosis was defined as definite or probable stent thrombosis according to the definitions of the Academic Research Consortium.13
Data regarding the primary and secondary end points were obtained through office visits or by telephone contact 1, 6, 9, and 12 months after the index procedure. For validation, information regarding vital status was obtained until September 2018 from the National Population Registry of the Korea National Statistical Office using a unique personal identification number. When available, each participating center was encouraged to collect additional follow-up information up to 3 years after the index procedure.
Statistical analysisThe expected rate of TLF was 5% in the conservative strategy group and 14% in the aggressive strategy group in patients with a non-true LM bifurcation lesion; the corresponding rates in those with a true bifurcation lesion were 7% in the conservative strategy group and 14% in the aggressive strategy group .5,14,15 With 5% type I error, 80% power, and a 5% drop-out rate, a total of 700 patients were needed (350 with a non-true bifurcation lesion and 350 with a true bifurcation lesion) to show that the conservative strategy was superior to the aggressive strategy. However, the SMART-STRATEGY II study was terminated early due to slow enrollment.
All data were analyzed according to the intention-to-treat principle. Categorical variables are summarized as numbers with percentages and were compared using Pearson chi-square or Fisher exact test. Continuous variables are presented as means with standard deviations and were compared using an independent t-test or Wilcoxon rank-sum test according to distribution normality. Time-to-event hazard curves were plotted using Kaplan-Meier estimates and were compared using a log-rank test. To ascertain variables independently associated with 1-year TLF, multivariable Cox regression was performed using clinically relevant covariates, including age, male sex, dyslipidemia, current smoking, diabetes, hypertension, chronic kidney disease, previous myocardial infarction, left ventricular ejection fraction, performance of follow-up angiography, treatment strategy, type of bifurcation lesion (true or non-true), bifurcation angle, length of MV disease, and presence of significant SB ostial stenosis (≥ 50%) after the index procedure.
All of the probability values are 2-tailed and P values <.05 were considered statistically significant. R software version 3.4.3 (R Foundation for Statistical Computing) was used for all statistical analyses.
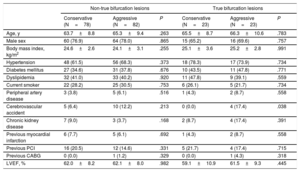
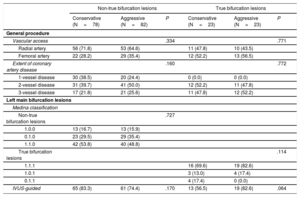
RESULTSBaseline clinical and procedural characteristicsA total of 206 patients with a LM bifurcation lesion (160 non-true bifurcation lesions and 46 true bifurcation lesions) were included in this study. The baseline clinical characteristics are shown in table 1 and were well-matched between the conservative and aggressive strategy groups. Regarding the procedural characteristics, there were no significant differences in vascular access, number of diseased vessels, Medina classification of the LM lesion, and intravascular ultrasound use between the 2 strategies in patients with non-true and true bifurcation lesions (table 2). All study patients were receiving dual antiplatelet therapy at the index procedure, and the rate of 1-year dual antiplatelet therapy did not differ between the conservative and aggressive strategy groups (97.0% vs 97.1%, P=.962).
Baseline clinical characteristics
| Non-true bifurcation lesions | True bifurcation lesions | |||||
|---|---|---|---|---|---|---|
| Conservative (N=78) | Aggressive (N=82) | P | Conservative (N=23) | Aggressive (N=23) | P | |
| Age, y | 63.7±8.8 | 65.3±9.4 | .263 | 65.5±8.7 | 66.3±10.6 | .783 |
| Male sex | 60 (76.9) | 64 (78.0) | .865 | 15 (65.2) | 16 (69.6) | .757 |
| Body mass index, kg/m2 | 24.6±2.6 | 24.1±3.1 | .255 | 25.1±3.6 | 25.2±2.8 | .991 |
| Hypertension | 48 (61.5) | 56 (68.3) | .373 | 18 (78.3) | 17 (73.9) | .734 |
| Diabetes mellitus | 27 (34.6) | 31 (37.8) | .676 | 10 (43.5) | 11 (47.8) | .771 |
| Dyslipidemia | 32 (41.0) | 33 (40.2) | .920 | 11 (47.8) | 9 (39.1) | .559 |
| Current smoker | 22 (28.2) | 25 (30.5) | .753 | 6 (26.1) | 5 (21.7) | .734 |
| Peripheral artery disease | 3 (3.8) | 5 (6.1) | .516 | 1 (4.3) | 2 (8.7) | .558 |
| Cerebrovascular accident | 5 (6.4) | 10 (12.2) | .213 | 0 (0.0) | 4 (17.4) | .038 |
| Chronic kidney disease | 7 (9.0) | 3 (3.7) | .168 | 2 (8.7) | 4 (17.4) | .391 |
| Previous myocardial infarction | 6 (7.7) | 5 (6.1) | .692 | 1 (4.3) | 2 (8.7) | .558 |
| Previous PCI | 16 (20.5) | 12 (14.6) | .331 | 5 (21.7) | 4 (17.4) | .715 |
| Previous CABG | 0 (0.0) | 1 (1.2) | .329 | 0 (0.0) | 1 (4.3) | .318 |
| LVEF, % | 62.0±8.2 | 62.1±8.0 | .982 | 59.1±10.9 | 61.5±9.3 | .445 |
CABG, coronary artery bypass grafting; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention.
Values are presented as No. (%) or mean±standard deviation.
Procedural characteristics
| Non-true bifurcation lesions | True bifurcation lesions | |||||
|---|---|---|---|---|---|---|
| Conservative (N=78) | Aggressive (N=82) | P | Conservative (N=23) | Aggressive (N=23) | P | |
| General procedure | ||||||
| Vascular access | .334 | .771 | ||||
| Radial artery | 56 (71.8) | 53 (64.6) | 11 (47.8) | 10 (43.5) | ||
| Femoral artery | 22 (28.2) | 29 (35.4) | 12 (52.2) | 13 (56.5) | ||
| Extent of coronary artery disease | .160 | .772 | ||||
| 1-vessel disease | 30 (38.5) | 20 (24.4) | 0 (0.0) | 0 (0.0) | ||
| 2-vessel disease | 31 (39.7) | 41 (50.0) | 12 (52.2) | 11 (47.8) | ||
| 3-vessel disease | 17 (21.8) | 21 (25.6) | 11 (47.8) | 12 (52.2) | ||
| Left main bifurcation lesions | ||||||
| Medina classification | ||||||
| Non-true bifurcation lesions | .727 | |||||
| 1.0.0 | 13 (16.7) | 13 (15.9) | ||||
| 0.1.0 | 23 (29.5) | 29 (35.4) | ||||
| 1.1.0 | 42 (53.8) | 40 (48.8) | ||||
| True bifurcation lesions | .114 | |||||
| 1.1.1 | 16 (69.6) | 19 (82.6) | ||||
| 1.0.1 | 3 (13.0) | 4 (17.4) | ||||
| 0.1.1 | 4 (17.4) | 0 (0.0) | ||||
| IVUS-guided | 65 (83.3) | 61 (74.4) | .170 | 13 (56.5) | 19 (82.6) | .064 |
IVUS, intravascular ultrasound.
Values are presented as No. (%).
Procedural outcomes are shown in table 3. Among patients with a non-true bifurcation lesion, the mean amount of contrast dye used was significantly smaller in the conservative than aggressive strategy group (221.1±77.7mL vs 259.9±117.9mL, P=.017). The mean fluoroscopic time and the rate of procedure-related myocardial infarction were not significantly different between the 2 strategies. During the procedure, 7 patients (9.0%) in the conservative strategy group underwent kissing balloon inflation due to SB compromise during the procedure. Among patients with a true bifurcation lesion, there were no significant differences in the fluoroscopic time, amount of contrast dye, and rate of procedure-related myocardial infarction between the conservative and aggressive strategy groups.
Procedural outcomes
| Non-true bifurcation lesions | True bifurcation lesions | |||||
|---|---|---|---|---|---|---|
| Conservative (N=78) | Aggressive (N=82) | P | Conservative (N=23) | Aggressive (N=23) | P | |
| General procedure | ||||||
| Number of treated lesions | 1.6±0.9 | 1.7±0.8 | .571 | 2.6±0.9 | 2.7±0.7 | .464 |
| Total number of stents | 1.7±0.9 | 1.8±0.9 | .375 | 2.1±0.7 | 2.8±0.9 | .005 |
| Mean time of fluoroscopy, min | 49.2±30.4 | 55.1±32.6 | .247 | 63.3±33.0 | 66.3±35.0 | .766 |
| Mean amount of contrast dye, mL | 221.7±77.7 | 259.9±117.9 | .017 | 245.0±85.2 | 286.9±141.8 | .233 |
| Procedure-related myocardial infarctiona | 9 (11.5) | 10 (12.2) | .898 | 3 (13.0) | 2 (8.7) | .642 |
| Main vessel | ||||||
| Number of stents per lesion, mm | 1.1±0.3 | 1.1±0.4 | .406 | 1.1±0.3 | 1.1±0.4 | .608 |
| Total stent length, mm | 24.7±10.2 | 27.7±12.5 | .100 | 24.7±12.5 | 24.8±12.8 | .993 |
| Maximal stent diameter, mm | 3.7±0.4 | 3.7±0.4 | .710 | 3.4±0.4 | 3.5±0.4 | .807 |
| Side branch | ||||||
| Balloon inflation | 7 (9.0) | 82 (100.0) | <.001 | 19 (82.6) | 23 (100.0) | .116 |
| Final kissing balloon inflation | 7 (9.0) | 82 (100.0) | <.001 | 16 (69.6) | 22 (95.7) | .052 |
| Stent implantation | 1 (1.3) | 2 (2.4) | .592 | 8 (34.8) | 23 (100.0) | <.001 |
| Number of stents per lesion, mm | 2.0 | 1.0±0.0 | NA | 1.0±0.0 | 1.0±0.2 | .329 |
| Total stent length, mm | 28.0 | 14.0±0.0 | NA | 17.4±4.7 | 19.6±8.6 | .527 |
| Maximal stent diameter, mm | 3.5 | 3.1±0.5 | NA | 3.2±0.3 | 3.0±0.5 | .446 |
| Treatment according to randomizationb | 78 (100.0) | 82 (100.0) | NA | 21 (91.3) | 23 (100.0) | .470 |
NA, not available.
Values are presented as No. (%) or mean±standard deviation.
Baseline characteristics and procedural outcomes according to treatment strategy in the overall population are presented in , , and .
Quantitative coronary analysisQuantitative coronary analysis was possible in 200 patients (97.1%) at baseline and in 113 patients at 9 months (54.5% of the conservative strategy group and 55.2% of the aggressive strategy group, P=.910) (figure 2 and ). Among non-true bifurcations lesions, there were no significant differences in the minimal lumen diameter of the SB or in binary (re)stenosis between the conservative and aggressive strategy groups after the index procedure and at follow-up. There were no significant differences in the MV in quantitative coronary analysis.
Among true bifurcation lesions, the conservative strategy had a lower minimal lumen diameter of the SB (2.1±0.9 vs 2.9±0.5mm; P=.001) after the index procedure than the aggressive strategy. SB (re)stenosis occurred in 6 patients (40.0%) in the conservative strategy group and in 3 patients (25.0%) in the aggressive strategy group; the difference was not significant (P=.681). There were no significant differences in the MV in quantitative coronary analysis.
Clinical outcomesThe median follow-up duration was 1028 days. Of a total of 206 patients, 200 (97.1%) completed the planned 1-year clinical follow-up (figure 2 and table 4). One-year TLFs were not significantly different between the conservative and aggressive strategies among patients with a non-true bifurcation lesion (6.5% vs 4.9%; hazard ratio [HR], 1.31; 95% confidence interval [95%CI], 0.35-4.88; P=.687) and among those with a true bifurcation lesion (17.6% vs 21.7%; HR, 0.76; 95%CI, 0.20-2.83; P=.683) (figure 3). The incidences of cardiac death, myocardial infarction, target lesion revascularization, and stent thrombosis were also not significantly different between the strategies. Out of 11 target lesion revascularizations during the first year after the index procedure, 3 events were due to angiographic restenosis incidentally found in follow-up angiography. Clinical outcomes according to treatment strategy in the overall population are presented in .
Clinical outcomes at 1 year
| Outcome | Conservative | Aggressive | Hazard ratio (95%CI) | P |
|---|---|---|---|---|
| Non-true bifurcation lesions | N=78 | N=82 | ||
| TLF | 5 (6.5) | 4 (4.9) | 1.31 (0.35-4.88) | .687 |
| Cardiac death | 3 (3.9) | 2 (2.6) | 1.60 (0.27-9.58) | .606 |
| MI | 0 (0.0) | 3 (2.7) | NA* | .091 |
| TLR | 2 (2.6) | 2 (2.5) | 1.06 (0.15-7.50) | .956 |
| Cardiac death or MI | 3 (3.9) | 4 (4.9) | 0.79 (0.18-3.52) | .755 |
| Definite or probable ST | 1 (1.3) | 1 (1.2) | 1.07 (0.07-17.03) | .964 |
| Target vessel revascularization | 3 (4.0) | 3 (3.7) | 1.06 (0.21-5.27) | .940 |
| True bifurcation lesions | N=23 | N=23 | ||
| TLF | 4 (17.6) | 5 (21.7) | 0.76 (0.20-2.83) | .683 |
| Cardiac death | 1 (4.3) | 1 (4.5) | 1.00 (0.06-15.99) | >.999 |
| MI | 2 (8.9) | 1 (5.3) | 2.07 (0.19-22.81) | .553 |
| TLR | 3 (13.9) | 4 (18.7) | 0.74 (0.16-3.29) | .688 |
| Cardiac death or MI | 2 (8.9) | 2 (8.7) | 1.01 (0.14-7.18) | .991 |
| Definite or probable ST | 1 (4.3) | 0 (0.0) | NA* | .317 |
| Target vessel revascularization | 3 (13.9) | 4 (18.7) | 0.74 (0.16-3.29) | .688 |
95%CI, 95% confidence interval; MI, myocardial infarction; NA, not available; ST, stent thrombosis; TLF, target lesion failure; TLR, target lesion revascularization.
Values are presented as No. (%).
TLF is a composite of cardiac death, MI, and TLR.
Of a total of 206 patients, 116 (56.3%) completed the 3-year follow-up. At 3 years, there were no significant differences in clinical outcomes between the conservative and aggressive strategies ().
Independent predictors of TLFIn multivariable Cox analysis, factors independently associated with 1-year TLF were a true bifurcation lesion (HR, 4.94; 95%CI, 1.60-15.21; P=.005), bifurcation angle (per 10°; HR, 0.78; 95%CI, 0.61-1.00; P=.046), and chronic kidney disease (HR, 5.45; 95%CI, 1.16-25.64; P=.032).
DISCUSSIONWe compared 2 different strategies for provisional SB ballooning and stenting in patients undergoing LM bifurcation interventions using a prospective, randomized trial. The principal findings were as follows: a) among patients with a non-true bifurcation lesion, the conservative strategy had a similar 1-year TLF using a smaller amount of contrast dye to the aggressive strategy; b) among patients with a true bifurcation lesion, there was no significant difference in 1-year TLF between the conservative and aggressive strategies; and c) the independent predictors of 1-year TLF were a true bifurcation lesion, bifurcation angle, and chronic kidney disease.
Previous studies have demonstrated that a provisional SB approach is superior to an elective 2-stent strategy in non-LM coronary bifurcation lesions.2–4,16 The provisional SB approach is also safe and feasible in LM bifurcation lesions.5,7–9 However, it has not been well-established when and how to perform a SB intervention after MV stenting during the provisional approach to LM bifurcation lesions. Although 1 study suggested that residual SB stenosis> 75% should be a criterion for SB intervention after MV stenting, the SB approach by type of bifurcation lesion was not provided in that study.9 The present study showed the feasibility of a conservative strategy for the provisional SB approach to both non-true and true bifurcation lesions.
FKB after MV stenting may improve SB ostial opening but requires SB rewiring. FKB after MV stenting also carries a risk of MV stent deformity or SB injury. Although FKB is considered mandatory in the elective 2-stent strategy, its role in the provisional SB approach is controversial. In non-LM bifurcation lesions, FKB during the provisional 1-stent strategy was associated with a longer procedural time, larger contrast volume, and similar clinical outcomes in a randomized study,11 whereas conflicting outcomes are found in real-world data.10,17 However, in LM bifurcation lesions, no randomized study has examined the role of FKB during the provisional SB approach, despite the significance of SBs with their large territory of subtended myocardium. One retrospective study found that the risk of adverse cardiac events was similar for MV stenting with and without FKB. However, the usefulness of this result was limited because the use of FKB was at the operator's discretion during the procedure.12
Among non-true bifurcation lesions in the present study, MV stenting alone without FKB had similar clinical outcomes to MV stenting with mandatory FKB. Our findings may be explained by the low risk of SB compromise, which limits the potential benefit of FKB. LM bifurcations have larger caliber vessels and a wider bifurcation angle than non-LM bifurcations.6 These characteristics could be protective factors for plaque and carina shift, a known mechanism of SB ostial lumen loss after MV stenting.18–20 In non-LM bifurcations, Koo et al.21 demonstrated that only 37% of lesions were functionally significant among jailed SBs with> 75% stenosis and that no lesion with a jailed SB with <75% stenosis was functionally significant. In LM bifurcations, a significant SB compromise occurs in only 7% of cases after MV stenting and in 17% when the SB has> 50% stenosis.22,23 In the quantitative coronary analysis of our study, the observed rate of SB stenosis> 50% after MV stenting without FKB was just 9.3%. In addition, the minimal lumen diameter of the SB ostium was similar for MV stenting alone and MV stenting with FKB. Therefore, routine FKB may be an unnecessary procedure after MV stenting in LM non-true bifurcation lesions.
Among true bifurcation lesions, clinical outcomes were not significantly different between the 1-stenting strategy with a provisional SB approach and elective 2-stenting. SB ostial disease is a major predictor of SB compromise and adverse outcomes in bifurcation PCI.8,20 In our study, a true bifurcation lesion was also an independent predictor of 1-year TLF. Several studies have compared the provisional 1-stent strategy and elective 2-stent strategy in the presence of significant SB ostial disease in LM bifurcation lesions. The DEFINITION study reported that the 2-stent strategy is required in lesions with SB stenosis> 70% and lesion length> 10mm, although the study included a small proportion of LM bifurcation lesions.24 The recent DKCRUSH-V randomized study25 demonstrated that the elective 2-stent strategy with double kissing crush technique resulted in a lower rate of TLF than provisional SB stenting in LM true bifurcation lesions. However, the DKCRUSH-V study had a different criterion for additional SB stenting (residual SB stenosis> 75% after kissing balloon inflation) vs our study. The European Bifurcation Coronary TWO (EBC) study,26 which included true bifurcation lesions with large-caliber SBs (≥ 2.5mm), determined that provisional T stenting had similar outcomes with a shorter procedure time to the culotte technique, as well as lower costs. The results of the EBC study support our findings that the 1-stent strategy with a provisional SB approach may be feasible in patients with a true LM bifurcation lesion.
The rate of periprocedural MI was higher than that of previous trials.27 A recent study reported that the rate of periprocedural MI varied substantially according to the MI definition applied, with periprocedural MI related to long-term adverse outcomes irrespective of its definition.28 Therefore, the incidence of periprocedural MI in our study would be explained by the lower threshold of periprocedural MI29 and have clinical implications.
This study has several limitations. First, the number of enrolled patients was much smaller than originally designed because patient enrollment was prematurely terminated due to slow enrollment. The statistical power was low because of the small study population, particularly patients with a true bifurcation lesion. Although there were no significant differences in 1-year TLF between the 2 different strategies, the application of the current results to real-world practice should be individualized based on patient and lesion characteristics. A large randomized study is needed to substantiate our findings. Second, operators possibly included patients with favorable anatomy for this study. However, because the quantitative coronary analytical results of the present study were not largely different from those of real-world data,8 the current results would not be significantly biased by the population selection. Third, intravascular ultrasound parameters were not provided, despite its high use (76.7%). Although most bifurcation studies have provided quantitative coronary analytical results as a main parameter, quantitative coronary analysis is sensitive to several factors, such as angiogram quality and projection angle. Intravascular ultrasound identifies the exact vessel size, plaque burden, and stent optimization. However, functionally significant flow disturbance in SBs is poorly associated with both quantitative coronary analysis and intravascular ultrasound parameters.23 Fourth, there was no information on the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score. However, considering the number of diseased vessels and treated lesions, the patients included in the present study appear to have been suitable candidates for PCI. Fifth, the fractional flow reserve measurement of SBs was at the operator's discretion and was not recorded. Given the controversy surrounding fractional flow reserve-guided PCI in bifurcation lesions,30 a randomized trial is needed to investigate the clinical benefit of the fractional flow reserve-guided strategy in LM bifurcation lesions. Sixth, clinical outcomes might be affected by the scheduled follow-up angiography. However, this type of bias is unlikely to explain our results because only 3 target lesion revascularizations were performed due to restenosis incidentally found in follow-up angiography and there was no significant difference in the rate of follow-up angiography between the conservative and aggressive strategies. Seventh, this was an open-label trial. This lack of blinding may have introduced bias in the symptom assessment during follow-up and in the clinical outcomes. Finally, various 2-stenting techniques were used in this study, which might have affected the clinical outcomes. However, the primary purpose of this study was to compare the 2 different strategies, not to compare specific stenting techniques in LM bifurcation lesions. In addition, because the study protocol was not limited to specific stenting techniques, the operators would have used the most familiar techniques, as in real-world practice.
CONCLUSIONSIn patients with LM bifurcation lesions, a conservative strategy for SB intervention had similar clinical outcomes to that of an aggressive strategy. However, the study was underpowered and inconclusive due to premature termination of patient enrollment. Larger studies are required to establish the optimal treatment strategy for LM bifurcation lesions.
- •
A 1-stent technique with provisional SB approach is considered the standard treatment for bifurcation lesions.
- •
However, in LM bifurcation lesions, when and how to perform SB intervention after MV stenting during the provisional approach have not been established.
- •
In this prospective, randomized, multicenter trial, a conservative strategy for provisional SB intervention had similar clinical outcomes to an aggressive strategy for LM bifurcation lesions.
- •
Because this trial was underpowered due to a relatively small sample size, larger studies are required to establish the optimal treatment strategies for LM bifurcation lesions.
There are no conflicts of interest.
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2020.06.011