Palliative care (PC) support has been broadened in the last few years to include patients with advanced-stage disease. Although heart failure (HF) has a poor prognosis, very few patients are actually included in PC programs1 due to a lack of integration of PC in HF management and its unpredictable clinical trajectory. Currently, prognostic markers in HF are highly focused on heart disease and have major limitations, since they do not include multimorbidity or other parameters such as dependence and frailty. PC involves support of physical, emotional and spiritual needs to both patients and their families and is not limited to end-of-life care. Nowadays, PC in HF is an unresolved challenge and identifying those patients who might require some type of palliative intervention is mandatory. The aim of our study was to evaluate theoretical PC requirements in HF by a simple scale that integrates predictive variables of HF severity with palliative approach elements according to patient needs; secondarily, we assessed its prognostic value in predicting mortality.
The NECPAL CCOMS-ICO questionnaire2 is a validated easy-to-use tool that identifies patients with advanced chronic palliative needs due to any cause. It includes 4 blocks: a) surprise question (SQ) for clinicians/nurses: “Would you be surprised if this patient died within 12 months?”; b) request for PC care by health professionals or the patient/family; c) generic clinical markers of health status severity and frailty (nutritional/functional markers, emotional distress, comorbidities); and d) disease-specific clinical prognostic markers for oncological, pulmonary, heart, neurological, liver, and renal diseases or dementia. For this study, we used the chronic heart disease-specific markers (from now on, NECPAL-HF). A patient was considered NECPAL-HF+when the SQ response was ‘No’ and ≥ 1 blocks were positive (at least 1 positive answer in blocks 2 and/or 3, or at least 2 positive answers in block 4).
All consecutive ambulatory patients attended in the HF clinics of 3 university hospitals during a 4-month period were enrolled. The NECPAL-HF questionnaire was applied by a nurse and/or a physician at a scheduled visit. Each patient's vital status was assessed at 1 year via hospital records, other hospital records, or by contacting the patient's relatives. Data were verified using the local health system databases. The study was conducted in accordance with the principles of the Declaration of Helsinki.
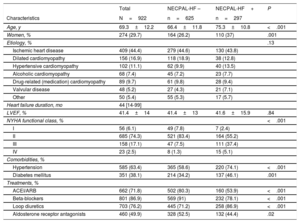
A total of 922 patients were included. The patients’ demographic, clinical, and treatment data are shown in Table 1. One third of the patients included were NECPAL-HF+(32.1%). NECPAL-HF+patients were older, predominantly women, mainly in New York Heart Association (NYHA) functional class III, and with higher diuretic treatment. Clinicians and nurses answered ‘No’ to the SQ in 35.2% of cases. Nevertheless, only 6.1% of patients had at least 1 positive answer in block 2 (4.1% by patients/families and 4.4% by clinician request). This finding may reflect the difficulty and extended avoidance of topics related to PC and/or death in noncancer patients in our environement. By contrast, 70.5% of patients had at least 1 positive answer in block 3 (having ≥ 2 concomitant diseases was the most usual criteria). Regarding block 4 (HF-specific items), only 16.9% had ≥ 2 positive indicators among the 6 evaluated by the questionnaire: “left ventricular ejection fraction (LVEF) <30% or pulmonary artery pressure> 60 mmHg” in 18.5% of the patients, and “NYHA functional class III/IV or severe valve disease or inoperable coronary disease” in 24.4%.
Demographic, Clinical, and Pharmacological Treatment Data of the Study Population
| Total | NECPAL-HF – | NECPAL-HF+ | P | |
|---|---|---|---|---|
| Characteristics | N=922 | n=625 | n=297 | |
| Age, y | 69.3±12.2 | 66.4±11.8 | 75.3±10.8 | <.001 |
| Women, % | 274 (29.7) | 164 (26.2) | 110 (37) | .001 |
| Etiology, % | .13 | |||
| Ischemic heart disease | 409 (44.4) | 279 (44.6) | 130 (43.8) | |
| Dilated cardiomyopathy | 156 (16.9) | 118 (18.9) | 38 (12.8) | |
| Hypertensive cardiomyopathy | 102 (11.1) | 62 (9.9) | 40 (13.5) | |
| Alcoholic cardiomyopathy | 68 (7.4) | 45 (7.2) | 23 (7.7) | |
| Drug-related (medication) cardiomyopathy | 89 (9.7) | 61 (9.8) | 28 (9.4) | |
| Valvular disease | 48 (5.2) | 27 (4.3) | 21 (7.1) | |
| Other | 50 (5.4) | 55 (5.3) | 17 (5.7) | |
| Heart failure duration, mo | 44 [14-99] | |||
| LVEF, % | 41.4±14 | 41.4±13 | 41.6±15.9 | .84 |
| NYHA functional class, % | <.001 | |||
| I | 56 (6.1) | 49 (7.8) | 7 (2.4) | |
| II | 685 (74.3) | 521 (83.4) | 164 (55.2) | |
| III | 158 (17.1) | 47 (7.5) | 111 (37.4) | |
| IV | 23 (2.5) | 8 (1.3) | 15 (5.1) | |
| Comorbidities, % | ||||
| Hypertension | 585 (63.4) | 365 (58.6) | 220 (74.1) | <.001 |
| Diabetes mellitus | 351 (38.1) | 214 (34.2) | 137 (46.1) | .001 |
| Treatments, % | ||||
| ACEI/ARB | 662 (71.8) | 502 (80.3) | 160 (53.9) | <.001 |
| Beta-blockers | 801 (86.9) | 569 (91) | 232 (78.1) | <.001 |
| Loop diuretics | 703 (76.2) | 445 (71.2) | 258 (86.9) | <.001 |
| Aldosterone receptor antagonists | 460 (49.9) | 328 (52.5) | 132 (44.4) | .02 |
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association. Data are expressed as mean±standard deviation, median [P25–P75], or absolute number (percentage).
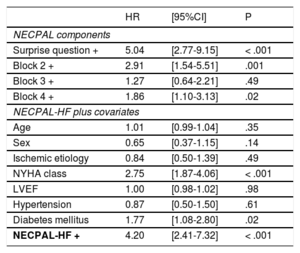
Although the tool was not designed to predict mortality, we also analyzed the association between NECPAL-HF+and prognosis. Cohort mortality at 1 year was 9.7% and was significantly higher in NECPAL-HF+patients (21.9% vs 3.8% in NECPAL-HF -; P <.001). Indeed, 73% of deaths occurred in NECPAL-HF+patients. The area under the ROC curve (AUC) for the NECPAL-HF+questionnaire and SQ+for predicting all-cause 1-year mortality were 0.73 (95% confidence interval [95%CI] 0.68-0.78) and 0.74 (95%CI 0.69-0.79), respectively. Table 2 (top) shows the hazard ratios of NECPAL-HF blocks regarding 1-year mortality in a multivariate binomial regression analysis. Remarkably, block 3, which was the most prevalently positive, showed the lowest prognostic value. The highest prognostic significance was found for the SQ, followed by request for PC care. Indeed, on multivariate regression analysis with other covariables, NECPAL-HF+remained independently associated with 1-year all-cause death (hazard ratio [HR] 4.20 [95%CI 2.41-7.32], P <.001), together with NYHA functional class and the presence of diabetes mellitus (Table 2, bottom).
Multivariate Binomial Regression Analyses for 1-year Mortality
| HR | [95%CI] | P | |
|---|---|---|---|
| NECPAL components | |||
| Surprise question + | 5.04 | [2.77-9.15] | < .001 |
| Block 2 + | 2.91 | [1.54-5.51] | .001 |
| Block 3 + | 1.27 | [0.64-2.21] | .49 |
| Block 4 + | 1.86 | [1.10-3.13] | .02 |
| NECPAL-HF plus covariates | |||
| Age | 1.01 | [0.99-1.04] | .35 |
| Sex | 0.65 | [0.37-1.15] | .14 |
| Ischemic etiology | 0.84 | [0.50-1.39] | .49 |
| NYHA class | 2.75 | [1.87-4.06] | < .001 |
| LVEF | 1.00 | [0.98-1.02] | .98 |
| Hypertension | 0.87 | [0.50-1.50] | .61 |
| Diabetes mellitus | 1.77 | [1.08-2.80] | .02 |
| NECPAL-HF + | 4.20 | [2.41-7.32] | < .001 |
95%CI, 95% confidence interval; HR, hazard ratio; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
No data on the NECPAL-HF questionnaire has been reported previously. The main result of our study was that one third of HF outpatients might require some type of palliative intervention when a tool that includes criteria of severity and extreme frailty is used, even considering that most were stable patients, in NYHA functional class II, had HF with mid-range ejection fraction, and were relatively young. This finding suggests the need for a holistic medical and social approach to the management of these patients. Secondarily, we found a reasonable predictive capacity of the tool for 1-year mortality (AUC 0.73), the predictive negative value being the most robust finding (96.2). Most of our patients were NECPAL-HF+due to block 3 (severe and extreme frailty criteria), far ahead of patients with positive specific severity HF items (block 4) or request for PC request (block 2), although this block 3 showed the lowest prognostic power. The SQ has been previously evaluated in many settings. In a recent meta-analysis that included 17 cohorts with heterogeneous conditions (cancer, renal failure and end-stage heart or lung disease) the SQ was worse at discriminating patients with noncancer illness (AUC 0.77) than patients with cancer (AUC 0.83).3 This AUC in noncancer patients was similar to that in our study (0.74).
In conclusion, the high prevalence found in our study for the need to receive PC suggests that a palliative approach should be implemented in multidisciplinary HF clinics to improve HF care, and that the evaluation of such patients should include elements such as comorbidity, functional and nutritional markers and frailty, beyond classic prognostic factors in HF. Further studies are needed to define how and when PC interventions in HF programs should be initiated, since the PAL-HF study4 showed the benefits of a longitudinal PC intervention on quality of life, emotional distress, and spiritual well-being compared with usual care.
FUNDINGThis work was supported by SGR 2014 and PERIS Programme-SLT002_16_00209, TerCel (RD16/0011/0006) and CIBER Cardiovascular-CB16/11/00403, and by FEDER.
We would like to acknowledge the work of the HF unit nurses in collecting the data and their invaluable patient care: Laura Ollè, María José Barbosa, Beatriz González, Roser Cabanes. Our thanks to Elba Beas and María Luisa Martínez-Muñoz; Josep Lupón for his critical and statistical analysis, and to Antoni Bayes-Genis for the developement of the idea for this study.