Complex percutaneous coronary intervention (PCI) typically involves the treatment of severe and extensive coronary artery disease that has been deemed unsuitable for coronary artery bypass grafting after a Heart Team discussion.1 In this clinical context, PCI is challenging and often requires complex techniques as well as the implantation of multiple stents. However, the outcomes of PCI can be compromised by clinical complications that are either directly (eg, stent thrombosis, periprocedural myocardial infarction) or indirectly related to the procedure (eg, acute kidney injury, bleeding complications). Although the definition of complex PCI may vary slightly among trials,2,3 there is a current consensus to include at least 1 of the following characteristics: 3 vessels treated, ≥ 3 lesions treated, total stent length >60mm, bifurcation with 2 stents implanted, use of any atherectomy device, left main as the target vessel, and surgical bypass graft or chronic total occlusion as target lesions.4 These features have previously been associated with an increased ischemic risk after PCI.5–7 The combination of complex PCI in patients with comorbidities and complicated heart disease defines a complex high-risk and indicated patient (CHIP).8 In this scenario, a CHIP-PCI score was developed from the British Cardiovascular Intervention Society (BCIS) database.9 Among a total of 313 054 patients, 7 patient factors (age >80 years, female sex, previous stroke, previous myocardial infarction, peripheral vascular disease, ejection fraction <30%, and chronic kidney disease) and 6 procedural factors (rotational atherectomy, left main PCI, 3-vessel PCI, dual arterial access, planned left ventricular mechanical support, and total lesion length >60mm) were independently associated with adverse in-hospital major adverse coronary or cerebrovascular events. These factors were used to construct a score, and a cutoff value of 5 or more was proposed to define a CHIP case.9
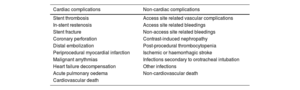
As mentioned above, percutaneous treatment of CHIP carries an increased risk of complications (table 1). Complex PCI requires the use of a higher number of stents in difficult anatomies (eg, bifurcations, calcified vessels, chronic total occlusions). Compared with noncomplex PCI, complex procedures usually require larger bore sheaths, additional nonradial access sites, increased contrast volume, and higher doses of heparin. They also demand more resources, such as intravascular imaging, ablative techniques, microcatheters, and specialized wires, and are associated with longer procedural times and higher radiation exposure. Consequently, the periprocedural risk of adverse events is elevated. Historically, the rate of major adverse cardiovascular events following complex PCI has been higher than that of noncomplex PCI.4
Complications during or following complex high-risk and indicated patient procedures
| Cardiac complications | Non-cardiac complications |
|---|---|
| Stent thrombosis | Access site related vascular complications |
| In-stent restenosis | Access site related bleedings |
| Stent fracture | Non-access site related bleedings |
| Coronary perforation | Contrast-induced nephropathy |
| Distal embolization | Post-procedural thrombocytopenia |
| Periprocedural myocardial infarction | Ischemic or haemorrhagic stroke |
| Malignant arrythmias | Infections secondary to orotracheal intubation |
| Heart failure decompensation | Other infections |
| Acute pulmonary oedema | Non-cardiovascular death |
| Cardiovascular death |
In a study involving 998 complex PCIs, those performed in CHIP showed a higher rate of in-hospital major complications compared with non-CHIP. The use of immunosuppressive drugs (odds ratio [OR], 3.040; 95% confidence interval [95%CI], 1.251–7.386; P=.014), unstable hemodynamics (OR, 5.753; 95%CI, 1.217–27.201; P=.027), and frailty (OR, 2.039; 95%CI, 1.108–3.751; P=.022) were identified as independent predictors of in-hospital complications among CHIP.10
In a recent article published in Revista Española de Cardiología, Avvedimento et al.11 assessed the outcomes of patients who were candidates for transcatheter aortic valve replacement (TAVR) and required complex PCI. Compared with noncomplex PCI, patients undergoing complex PCI had higher rates of cardiovascular death, nonperiprocedural myocardial infarction, coronary revascularization, and stent thrombosis. Notably, these procedures were staged and mostly performed before TAVR (94%). In a multivariable model, complex PCI was identified as an independent predictor of major adverse cardiac events together with other factors such as prior myocardial infarction, previous bypass graft, chronic kidney disease, nontransfemoral access, and incomplete revascularization.
An interesting aspect of the study is that differences in outcomes were not observed during the periprocedural period up to 30 days; rather, they appeared during long-term follow-up (median 2 years). This finding underscores on the one hand, the acute-subacute (30 days) safety of complex PCI procedures performed in patients with severe aortic stenosis before TAVR. But, on the other hand, adverse events accumulated during follow-up when other clinical conditions associated with the patient or technical considerations derived from the index procedure could contribute to the late increase in events. In this context, patients who underwent complex PCI had more extensive coronary artery disease, more frequent chronic obstructive pulmonary disease, lower ejection fraction, and higher residual SYNTAX scores—all of which are negative prognostic factors.11
In line with these finding, Fujimoto et al.12 identified several predictors of adverse events during follow-up after complex PCI, including active malignancy, pulmonary disease, hemodialysis, unstable hemodynamics, left ventricular ejection fraction, and valvular disease. Similarly, Brener et al.13 demonstrated that PCI performed in CHIP had a 2.5-fold higher risk of 1-year mortality, with 4 factors independently associated with 1-year mortality: age >80 years, dialysis, low ejection fraction, and treatment of multiple lesions.
Quoting Mahatma Gandhi, “The future depends on what we do in the present.” In line with this, the treatment of bifurcation lesions, calcified lesions, ostial lesions, chronic total occlusions, the use of ablative techniques (eg, cutting balloon, rotational atherectomy), and the total number of stents implanted were significantly higher in complex PCI patients.11 Consequently, at long-term follow-up, the rates of stent thrombosis and target lesion revascularization were 10 times and 3 times higher, respectively, in the complex PCI group compared with the noncomplex PCI group. Ultimately, the rate of cardiac death was roughly 40% higher in the complex PCI group.11
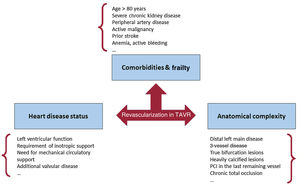
When considering the treatment of coronary artery disease in patients requiring TAVR, physicians should take into account noncardiac comorbidities (eg, chronic obstructive pulmonary disease, chronic kidney disease, frailty, peripheral artery disease, anemia), the status of the heart (ejection fraction, other associated valvulopathies), and the extent and complexity of coronary artery disease (figure 1). Often, coronary stenoses identified incidentally during pre-TAVR angiography may not require percutaneous revascularization in patients without angina and/or located in nonproximal segments or in secondary vessels.
A recent consensus document from the European Association of Percutaneous Cardiovascular Interventions on managing patients with coronary artery disease undergoing TAVR suggests that PCI should be performed before TAVR in patients with severe coronary artery disease (defined as stenosis >50% in the left main or >70% in all other coronary arteries) only in proximal segments, particularly in those presenting with acute coronary syndromes (ACS) or symptomatic angina.14 Challenging these recommendations, a recent study demonstrated that TAVR can be safely performed in stable patients even in the presence of untreated high or extreme degrees of chronic coronary artery disease. However, during follow-up, patients with untreated obstructive coronary artery disease showed a higher rate of unplanned revascularization or ACS.15
In summary, the revascularization of complex coronary artery disease in patients with severe aortic stenosis requiring TAVR should be individualized, taking into account concomitant comorbidities, life expectancy, and procedural and technical factors, with the aim of optimizing outcomes without compromising their future.
FUNDINGNone.
CONFLICTS OF INTERESTThe author is a consultant for Abbott Vascular and iVascular, stent manufacturers, outside the scope of this manuscript.