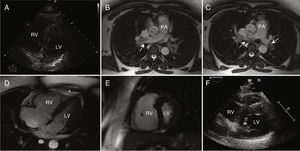
We present the case of a 29-year-old woman, 11 weeks pregnant, who sought treatment due to chest pain, dyspnea, and palpitations, with no other relevant history. Although the physical examination was unremarkable, an electrocardiogram revealed sinus tachycardia and blood tests showed elevated high-sensitivity troponin T but normal D-dimer (DD) levels. Transthoracic echocardiography revealed a normal left ventricle (LV) but dilated right ventricle (RV) with signs of overload (figure 1A). Doppler echocardiography of the lower limbs ruled out deep vein thrombosis. Because of a suspected pulmonary embolism (PE) and in order to avoid exposure of a pregnant patient to ionizing radiation, cardiac magnetic resonance imaging was performed instead of computed tomography angiography (CTA). The scan confirmed the presence of bilateral PE with subocclusive thrombi in both pulmonary arteries (arrows) and a dilated RV (RV/LV ratio > 1.0) with severely depressed systolic function (29%), McConnell sign (asterisk), and diastolic flattening of the interventricular septum (figure 1B-E; ).
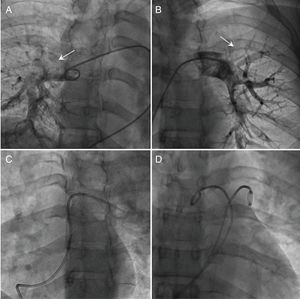
At admission, the patient had a Pulmonary Embolism Severity Index (PESI) score of 49. Despite anticoagulant therapy with intravenous unfractionated heparin, she showed a poor clinical course during the first 4hours with persistent hypotension, need for low-dose noradrenaline (0.2μg/kg/min), and respiratory deterioration. For the latter, she required high-flow oxygen therapy (FiO2 99%). Her PESI score was now 119. After consideration of the risks and benefits of the various reperfusion therapy strategies available, the multidisciplinary team with experience in treating PE in our hospital (comprising an intensivist, cardiologist, and, in this case, a gynecologist) decided to perform emergency percutaneous treatment of the high-risk PE (HR-PE). At the start of the procedure, the patient had pulmonary hypertension [40/25(30) mmHg] with reduced aortic pressure [88/49(62) mmHg]. Pulmonary angiography (figure 2A and B) confirmed the presence of subocclusive thrombi in both pulmonary arteries. Accordingly, mechanical fragmentation and manual thrombus aspiration were performed (figure 2C). This approach stabilized the hemodynamic situation. However, because the pulmonary hypertension persisted, the procedure was completed with local low-dose catheter-directed thrombolysis at 1mg/h for 12hours per catheter (figure 2D). After 24hours, the pulmonary hypertension [30/15(20) mmHg] and aortic pressure [122/64(83) mmHg] had recovered and follow-up echocardiography revealed normalized function and RV diameters (figure 1F). At 6 months and under anticoagulant therapy with enoxaparin 80mg/12h, the patient's pregnancy was proceeding as normal.
Pregnancy is a procoagulant state that increases the risk of PE by up to 10 times. PE has high mortality (20% in developed countries) and is the leading cause of cardiovascular death in pregnant women.1,2 The specific characteristics of pregnancy result in scientific evidence that is slight and rarely validated. Dyspnea, palpitations, and lower limb swelling are frequent symptoms during pregnancy and the DD is also physiologically elevated, which is why the diagnosis of PE is typically complex.1,2 A peculiarity of our patient is that, despite a DD within normal limits and suggestive echocardiographic findings, our suspicion was confirmed using cardiac magnetic resonance imaging, a promising but as yet unvalidated technique in this field that avoids diagnostic exposure of the fetus to ionizing radiation and iodine contrast. Nonetheless, due to the low radiation administered by modern systems and their widespread availability and validity, CTA is currently the technique of choice, even in pregnant patients.
After PE confirmation, the risk should be stratified and the corresponding treatment initiated without delay.2 In this case, the patient initially had moderate-to-high–risk PE (without shock/hypotension but with RV dysfunction and elevated high-sensitivity troponin T) and, despite the early initiation of anticoagulation, experienced respiratory deterioration with persistent hypotension, worsening to HR-PE. Accordingly, because pregnancy is a contraindication for systemic fibrinolysis (SF), rescue percutaneous reperfusion therapy was performed instead. The teratogenicity of SF is currently unknown. However, its use during pregnancy is associated with high rates of maternal bleeding (up to 18% during pregnancy and 58% in the immediate postpartum period), together with nonnegligible fetal mortality and premature birth rates (12% and 36%, respectively).2 Nonetheless, these rates can be significantly reduced with prolonged lower-dose administration of local catheter-directed thrombolysis (24mg in 12-24hours vs 100mg in 2hours in SF).
The objective of the percutaneous treatment of HR-PE is to resolve the acute thrombotic obstruction and re-establish the flow in the main pulmonary arteries to decrease the RV overload, thereby stabilizing the hemodynamic situation and improving patient survival without appreciably increasing the bleeding risk. There is currently no evidence from randomized trials that have evaluated this therapeutic modality, least of all in pregnant women. However, its use has spread in recent years and it has been shown to be an effective and safe alternative in selected patients. Indeed, in the latest European guidelines, percutaneous treatment as an alternative to rescue SF in patients with hemodynamic deterioration under treatment with anticoagulation has been upgraded from a class IIb recommendation to a class IIa.2 Nonetheless, it is still an invasive technique that requires the use of ionizing radiation and iodine contrast. Accordingly, every effort must be made to minimize exposure through the use of lead protection, optimized fluoroscopy, and minimal quantities of contrast agent (20mL).
Our case shows that percutaneous treatment of HR-PE can be a safe and effective alternative strategy during pregnancy, when the potential complications from SF can be devastating.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.10.018