To the Editor:
We appreciate the comments from Carrillo et al. We will try to respond to the questions raised.
Regarding point 1, the number of multivessel patients is quite low. This is due to the inclusion process1 from the electrocardiogram (ECG) at admission which showed the most acute ischaemic changes, and which have been described as suggesting left coronary artery (LCA) disease.2,3 Out of a total of 840 patients with acute coronary syndrome (ACS), 57 patients who met the electrocardiographic criteria and had coronary angiography in the acute phase were included. We agree that multivessel involvement is more prevalent than the LCA in ACS, but its prevalence is revealed by coronary angiography, which does not necessarily correlate with the extension of the ischaemia; for example, one patient may be admitted for ACS caused by obstruction of a marginal artery and three-vessel disease is found on coronary angiography.
We agree with point 2 that the ECG can be normal in the absence of acute ischaemia even though coronary involvement is severe. Space limitations do not permit commenting on aspects that are well-known.
On point 3, it is true that all patients with LCA involvement have ST-segment depression in II. In the 20 patients with LCA involvement, the extensive ischaemia of the endocardium creates an ST-vector directed towards quadrant-A (between -90o and -180º), which is why the ST segment has to be elevated in aVR and depressed in II. Coronary artery disease is a diffuse process and significant involvement in other territories cannot be ruled out despite having a "luminogram" on the coronary angiography that does not show severe stenosis.4,5
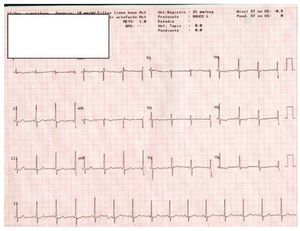
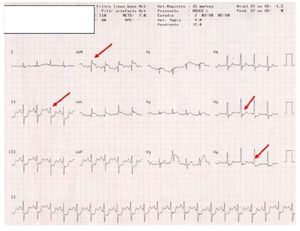
We agree with point 4, that the ECG of the LCA and multivessel involvement may be similar.2,3 The ST vector in multivessel disease will vary depending on the artery that causes the acute ischaemia and on the intensity and extension of the ischaemia, which is why the ST vector in multivessel disease may be similar if there is extensive ischaemia in the territory of the left anterior descending and circumflex arteries.3 The following recent case illustrates the value of vector analysis of the ECG in "pure" ischaemia due to LCA obstruction: a young woman with central chest pain with effort. Sudden death preceded by chest pain upon carrying bags up a slope in front of the hospital and resuscitated successfully. The ECG on admission to the ICU only showed nonspecific changed in repolarisation (Figure 1); neurological recovery is complete and the coronary angiography is "normal." A stress test is performed in which extensive ischaemia compatible with LCA involvement is seen: a large ST vector towards quadrant-A is seen in the frontal plane and anterior in the horizontal plane, and the QRS vector is shifted to the left with an anterior hemiblock (Figure 2). Coronary angiography is repeated with subselective injection in the left coronary sinus and a "mass" impacting the LCA with severe obstruction is seen; when the catheter is introduced, the "mass" is displaced and the coronary angiography appears normal. A transoesophageal echocardiogram revealed a papillary fibroelastoma. She was operated on successfully.
Figure. 1. Electrocardiogram at admission in which nonspecific repolarisation changes are seen.
Figure 2. Electrocardiogram during induced ischaemia on the stress test. An ST-segment vector towards quadrant-A is generated in the frontal plane and anterior in the horizontal plane. The QRS vector is shifted to the left due to an anterior hemiblock.
Regarding point 5, we completely agree that in the majority of patients, the artery that causes the posteroinferior MI can be located.3,6,7
Finally, we once again thank Carrillo et al for their comments and their interest in our article.