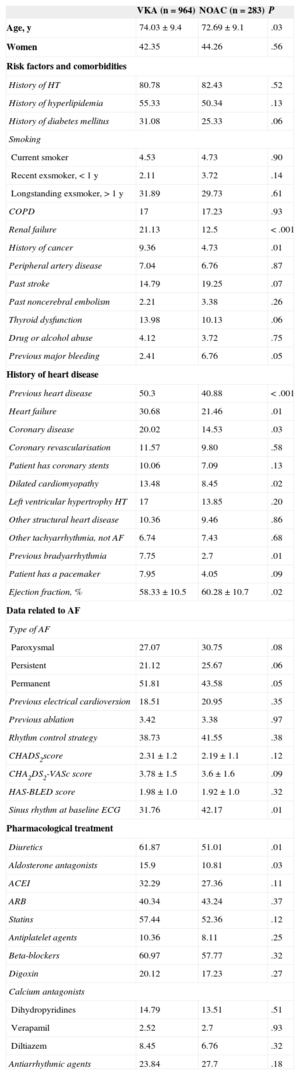
Oral anticoagulants (OAC) significantly reduce the risk of thromboembolism in patients with nonvalvular atrial fibrillation. In addition to oral anticoagulation with the traditional vitamin K antagonists (VKA), for the past few years, new oral anticoagulants (NOAC) have been available, whose efficacy and safety are at least similar to those of VKA.1 One of the advantages of these drugs lies in the stability of their anticoagulant action, obviating the need for systematic follow-up and thus making them more convenient for patients to use. It is important to determine patients’ opinion of the treatment and care provided to them, but this is often overlooked. The objective of our study was to analyze satisfaction among patients with nonvalvular atrial fibrillation with OAC-related medical care and to compare those receiving VKA or NOAC. To do this, we studied the first 1247 patients included in the FANTASIIA registry.2 This per-protocol analysis included consecutive patients treated with VKA and NOAC (at a proportion of 4:1) who had received OAC for at least 6 months prior to the inclusion visit in 50 Spanish centers between June 2013 and March 2014. A total of 964 patients took VKA and 283 took NOAC. Their baseline characteristics are listed in Table 1. All the patients completed the SAFUCA questionnaire3 on satisfaction with medical care, which includes 25 items grouped under 7 domains (efficacy of medication, convenience of medication, anticoagulation monitoring, interference of the medication with daily life, undesirable effects, medical follow-up, and general satisfaction) (Table 2). Each item is scored from 0 to 4 (0 = not at all; 4 = a lot), which is integrated to obtain a global score of 0 to 100 for each domain and for a global summary of the score.3 In domains 1 (efficacy of medication), 2 (convenience of medication), 6 (medical follow-up) and 7 (general opinion on medication), the closer to 100 the score, the greater the satisfaction. For domains 3 (coagulation monitoring), 4 (interference of medication with daily life) and 5 (undesirable effects), the closer to 0 the score, the lower the degree of concern, but for the interpretation to be the same for all domains, and for the global score, the score was “normalised” for domains 3, 4 and 5 by inverting the score (100 minus the value obtained), so that for all domains, the closer to 100 the score, the greater the satisfaction (Table 2). This score had an adequate Cronbach's alpha (0.861) and had a high test-retest reliability coefficient (0.935) in previous studies.3 The global results and the results by OAC subgroups are listed in Table 2. Overall, satisfaction with the medical care was high (score of 74.74/100), and satisfaction was lowest for “coagulation monitoring”. In the OAC subgroups, the scores were significantly higher in all domains and the global score of patients with NOAC (Table 2). Therefore, it seems that satisfaction with medical care, or at least the perception of OAC in patients with nonvalvular atrial fibrillation receiving this treatment, is generally good; satisfaction was higher among patients receiving NOAC and was slightly lower, with statistically significant differences, among those who receiving VKA. The parameter with the worst score for patients taking VKA was the need for regular coagulation check-ups. This was also the case in patients taking NOAC, although satisfaction was significantly higher than with VKA. This finding was surprising, since these patients were not taking VKA and therefore, theoretically, did not require systematic anticoagulation monitoring. Despite the explanations given prior to distributing the questionnaire, these patients may have put themselves in the situation of when they needed check-ups (those who had previously taken VKA) or imagined that they would need them if they were to take VKA in the future.
General Characteristics of Patients Taking Vitamin K Antagonists and New Oral Anticoagulants in the FANTASIIA Study
| VKA (n = 964) | NOAC (n = 283) | P | |
|---|---|---|---|
| Age, y | 74.03 ± 9.4 | 72.69 ± 9.1 | .03 |
| Women | 42.35 | 44.26 | .56 |
| Risk factors and comorbidities | |||
| History of HT | 80.78 | 82.43 | .52 |
| History of hyperlipidemia | 55.33 | 50.34 | .13 |
| History of diabetes mellitus | 31.08 | 25.33 | .06 |
| Smoking | |||
| Current smoker | 4.53 | 4.73 | .90 |
| Recent exsmoker, < 1 y | 2.11 | 3.72 | .14 |
| Longstanding exsmoker, > 1 y | 31.89 | 29.73 | .61 |
| COPD | 17 | 17.23 | .93 |
| Renal failure | 21.13 | 12.5 | < .001 |
| History of cancer | 9.36 | 4.73 | .01 |
| Peripheral artery disease | 7.04 | 6.76 | .87 |
| Past stroke | 14.79 | 19.25 | .07 |
| Past noncerebral embolism | 2.21 | 3.38 | .26 |
| Thyroid dysfunction | 13.98 | 10.13 | .06 |
| Drug or alcohol abuse | 4.12 | 3.72 | .75 |
| Previous major bleeding | 2.41 | 6.76 | .05 |
| History of heart disease | |||
| Previous heart disease | 50.3 | 40.88 | < .001 |
| Heart failure | 30.68 | 21.46 | .01 |
| Coronary disease | 20.02 | 14.53 | .03 |
| Coronary revascularisation | 11.57 | 9.80 | .58 |
| Patient has coronary stents | 10.06 | 7.09 | .13 |
| Dilated cardiomyopathy | 13.48 | 8.45 | .02 |
| Left ventricular hypertrophy HT | 17 | 13.85 | .20 |
| Other structural heart disease | 10.36 | 9.46 | .86 |
| Other tachyarrhythmia, not AF | 6.74 | 7.43 | .68 |
| Previous bradyarrhythmia | 7.75 | 2.7 | .01 |
| Patient has a pacemaker | 7.95 | 4.05 | .09 |
| Ejection fraction, % | 58.33 ± 10.5 | 60.28 ± 10.7 | .02 |
| Data related to AF | |||
| Type of AF | |||
| Paroxysmal | 27.07 | 30.75 | .08 |
| Persistent | 21.12 | 25.67 | .06 |
| Permanent | 51.81 | 43.58 | .05 |
| Previous electrical cardioversion | 18.51 | 20.95 | .35 |
| Previous ablation | 3.42 | 3.38 | .97 |
| Rhythm control strategy | 38.73 | 41.55 | .38 |
| CHADS2score | 2.31 ± 1.2 | 2.19 ± 1.1 | .12 |
| CHA2DS2-VASc score | 3.78 ± 1.5 | 3.6 ± 1.6 | .09 |
| HAS-BLED score | 1.98 ± 1.0 | 1.92 ± 1.0 | .32 |
| Sinus rhythm at baseline ECG | 31.76 | 42.17 | .01 |
| Pharmacological treatment | |||
| Diuretics | 61.87 | 51.01 | .01 |
| Aldosterone antagonists | 15.9 | 10.81 | .03 |
| ACEI | 32.29 | 27.36 | .11 |
| ARB | 40.34 | 43.24 | .37 |
| Statins | 57.44 | 52.36 | .12 |
| Antiplatelet agents | 10.36 | 8.11 | .25 |
| Beta-blockers | 60.97 | 57.77 | .32 |
| Digoxin | 20.12 | 17.23 | .27 |
| Calcium antagonists | |||
| Dihydropyridines | 14.79 | 13.51 | .51 |
| Verapamil | 2.52 | 2.7 | .93 |
| Diltiazem | 8.45 | 6.76 | .32 |
| Antiarrhythmic agents | 23.84 | 27.7 | .18 |
ACEI, angiotensin-converting enzyme inhibitors; AF, atrial fibrillation; ARB, angiotensin receptor blocker; COPD, chronic obstructive pulmonary disease; ECG, electrocardiogram; HT, hypertension; NOAC, new oral anticoagulants; VKA, vitamin K antagonists.
Data are expressed as mean ± standard deviation (quantitative variables) and percentages (qualitative variables).
Domains and Items of the SAFUCA (A) Questionnaire and Global Results and the Results of Score Comparisons Between Patients Receiving Vitamin K Antagonists and New Anticoagulants (B)
| A. Domains and items of the SAFUCA questionnaire |
| Domain 1. Efficacy of medication |
| Item 1. I think that my disease is currently well controlled |
| Item 2. I think that the treatment I am taking will solve the problem |
| Item 3. I am convinced that using anticoagulants is good for me |
| Domain 2. Convenience of medication |
| Item 4. I find taking my medication convenient |
| Item 5. I find it easy to take my medication in its current format (taste, size, etc.) |
| Item 6. I find it convenient to take the drug once a day |
| Domain 3. Coagulation monitoring |
| Item 7. Coagulation check-ups involve travelling and wasting a lot of time |
| Item 8. I prefer an anticoagulant that does not need to be continuously monitored |
| Item 9. I find it inconvenient to depend on the doctor and nurse to regulate my anticoagulant interference of medication |
| Item 10. I find it difficult to control my dose if I am away for a few days |
| Domain 4. Interference of medication with daily life |
| Item 11. My anticoagulant medication interferes with my personal hygiene (shaving, brushing my teeth, etc.) |
| Item 12. The medication I use interferes with my work or profession |
| Item 13. The medication I use interferes with my family life |
| Item 14. I find it difficult to control meals that can interfere with the anticoagulant (green vegetables, alcohol, etc.) |
| Item 15. I am bothered that I have to pay attention to the anticoagulant all day |
| Item 16. I have stopped doing certain things for fear of bruises and bleeding |
| Domain 5. Adverse effects caused by the anticoagulant medication |
| Item 17. The undesirable effects of the treatment (bleeding, haemorrhage, bruising, etc.) bother me |
| Item 18. The side effects of the anticoagulant medication interfere with my leisure activities and free time |
| Item 19. The side effects of the medication interfere with my activities of daily life |
| Domain 6. Medical follow-up of the disease |
| Item 20. The health care staff have informed me in detail of my arrhythmia |
| Item 21. The health care staff have informed me on how to treat my arrhythmia correctly |
| Item 22. I trust the healthcare staff treating me |
| Domain 7. General opinion on the medication and health condition |
| Item 23. I feel happy with the medication |
| Item 24. In general, I am satisfied with the medication |
| Item 25. I am convinced that the treatment I am taking is the best option available |
| B. Scores and comparisons | ||||
|---|---|---|---|---|
| All (n = 1247) | VKA (n = 964) | NOAC (n = 283) | P | |
| Efficacy of medication | 73.83 ± 21.49 | 72.70 ± 22.08 | 77.63 ± 18.94 | .0026 |
| Convenience of medication | 75.39 ± 22.74 | 73.72 ± 23.23 | 80.99 ± 20.07 | < .0001 |
| Coagulation monitoring | 58.72 ± 29.16 | 57.66 ± 27.32 | 62.35 ± 34.49 | .0018 |
| Interference of medication | 83.83 ± 19.88 | 81.97 ± 20.37 | 90.08 ± 16.70 | < .0001 |
| Undesirable effects | 80.82 ± 23.67 | 79.21 ± 24.31 | 86.20 ± 20.51 | < .0001 |
| Medical follow-up | 79.12 ± 22.14 | 77.90 ± 22.34 | 83.19 ± 20.99 | .0001 |
| General satisfaction | 71.89 ± 22.47 | 69.38 ± 22.80 | 80.30 ± 19.09 | < .0001 |
| Total score | 74.74 ± 15.69 | 73.22 ± 16.06 | 79.91 ± 13.12 | < .0001 |
VKA, vitamin K antagonists; NOAC, new oral anticoagulants.
Data are expressed as mean ± standard deviation.
These results indicate that it is necessary to determine patients’ perception of the care given and their satisfaction with this care, as well as the efficacy and safety of the treatments, as the findings may lead to better therapeutic adherence, which is always important, but even more so when using drugs that are difficult to control, such as OAC. It is therefore essential to have specific tools for atrial fibrillation, such as the SAFUCA questionnaire, and other validated quality of life scales for this disease.4
FUNDINGThis study was funded by an unconditional grant from Pfizer S.L.U.