In infective endocarditis (IE), decisions on surgical interventions are challenging and a high percentage of patients with surgical indication do not undergo these procedures. This study aimed to evaluate the short- and long-term prognosis of patients with surgical indication, comparing those who underwent surgery with those who did not.
MethodsWe included 271 patients with left-sided IE treated at our institution from 2003 to 2018 and with an indication for surgery. There were 83 (31%) surgery-indicated not undergoing surgery patients with left-sided infective endocarditis (SINUS-LSIE). The primary outcome was all-cause death by day 60 and the secondary outcome was all-cause death from day 61 to 3 years of follow-up. Multivariable Cox regression and propensity score matching were used for the analysis.
ResultsAt the 60-day follow-up, 40 (21.3%) surgically-treated patients and 53 (63.9%) SINUS-LSIE patients died (P <.001). Risk of 60-day mortality was higher in SINUS-LSIE patients (HR, 3.59; 95%CI, 2.16-5.96; P <.001). Other independent predictors of the primary endpoint were unknown etiology, heart failure, atrioventricular block, and shock. From day 61 to the 3-year follow-up, there were no significant differences in the risk of death between surgically-treated and SINUS-LSIE patients (HR, 1.89; 95%CI, 0.68-5.19; P=.220). Results were consistent after propensity score matching. Independent variables associated with the secondary endpoint were previous IE, diabetes mellitus, and Charlson index.
ConclusionsTwo-thirds of SINUS-LSIE patients died within 60 days. Among survivors, the long-term mortality depends more on host conditions than on the treatment received during admission.
Keywords
Infective endocarditis (IE) is a serious, unpredictable, and complex entity with high morbidity and mortality (20%-30%), despite recent advances in diagnostic and therapeutic strategies.1–4 The epidemiology of left-sided infective endocarditis (LSIE) has changed5–9 for institutionalized patients with multiple comorbidities. Cardiac surgery is an established treatment for IE, required in approximately half of the patients because of severe complications.10–12 During the active phase, surgery is associated with significant risk and it is difficult to determine whether if should be performed and, if so, its timing. Recent studies have demonstrated that less than 50% of all LSIE patients with surgical indications undergo surgery after evaluation of their perioperative risk.13–15 Classical surgical risk scores (STS/EuroSCORE) are not accurate for IE, and new risk scores are being scrutinized.16–18 The identification of specific risk factors is mandatory for this disease, in which surgery carries a non-negligible risk.
There is little information on the clinical characteristics and short- and long-term outcomes of surgery-indicated not undergoing surgery patients with left-sided infective endocarditis (SINUS-LSIE). Several studies13,19,20 have compared surgically and nonsurgically-treated patients. It is presumed that in-hospital mortality in SINUS-LSIE patients is high; however, this presumption has not been prospectively examined in a rigorous manner. In addition, the outcomes are uncertain for those who survive hospitalization and are strictly followed up by a multidisciplinary team. Accordingly, the present study of a contemporary cohort of patients with LSIE was designed to evaluate the short- and long-term prognosis of patients with surgical indications, according to current clinical practice guidelines,21 comparing those who underwent surgery with those who did not.
METHODSStudy design and populationThis prospective, observational consecutive cohort study was performed at Hospital Germans Trias i Pujol, a 650-bed tertiary-care hospital that serves a population of ∼850 000 inhabitants. The institution has a multidisciplinary endocarditis team (created in 2009) that includes specialists in cardiology, infectious diseases, internal medicine, neurology, microbiology, cardiac imaging, and cardiac surgery. This multidisciplinary IE team holds regular meetings to discuss and evaluate the therapeutic strategies for IE patients. We enrolled all consecutive adult patients (≥ 18 years of age) with a definite diagnosis of LSIE (Modified Duke criteria/ESC 2015 modified criteria since 2015) admitted to our center from January 2003 to March 2018. We excluded patients with right-sided and cardiac device-related IE. For patients who were admitted more than once for LSIE during the study period, we recorded only the first admission episode.
Demographic, clinical, diagnostic (imaging, microbiological, and analytical parameters) and follow-up data were obtained from the patients’ medical charts using standardized reporting forms. Health care-associated endocarditis was defined as either IE that developed more than 48hours following hospital admission, or IE acquired as a result of an invasive procedure within the previous 8 weeks before the development of signs and symptoms or diagnosed within the first 48hours of admission in patients with extensive out-of-hospital contact with the health care system (intravenous therapy or hemodialysis).22 The Charlson index23 was used at admission to stratify overall comorbidity. The estimated glomerular filtration rate was measured using the Chronic Kidney Disease-Epidemiology Collaboration method. Moderate or severe renal disease is defined by an estimated glomerular filtration rate less than 60mL/min/1.73 m2 at admission. Surgery was defined as replacement or repair of the affected valve during the index hospitalization. Indications for surgery were validated prospectively during the index episode by the multidisciplinary endocarditis team and included the following: heart failure, embolic event, persistent bacteremia, local/paravalvular complications, severe acute valvular regurgitation, vegetation size, early prosthetic valve IE, and multiresistant microorganisms. The reasons for the lack of surgery were also collected. Patients discharged with a plan for readmission for surgery later during the course of treatment were included in the surgery group.
Study outcomes and follow-upThe primary outcome of this study was all-cause mortality by day 60. The secondary outcome was all-cause death from day 61 to the 3-year follow-up (follow-up begins from the day of the start of antibiotic treatment for endocarditis). After discharge, survivors were prospectively followed up with regular predefined visits (at 1, 3, and 6 months, 1 year, and 3 years) by the IE team. An echocardiogram was performed at each regular visit. Patients not attending a regular visit were contacted by telephone. Otherwise, information was obtained from the patient's clinical record and by consulting the regional government death registry. This study was performed in compliance with the Helsinki Declaration and was approved by the local Ethics Committee of Hospital Universitario Germans Trias i Pujol (Badalona, Barcelona).
Statistical analysisCategorical variables are expressed as the number and percentage. Continuous variables are expressed as the mean and standard deviation (SD) or median and 25–75 percentiles, according to their distribution (normal or nonnormal). Normal distribution was assessed using normal Q-Q plots. Statistical significance for comparisons between groups was determined with the chi-square test or Fisher's exact test for categorical variables and Student t tests or Wilcoxon rank sum test for continuous variables. The characteristics of surgically-treated patients were compared with those of SINUS-LSIE patients. Univariate Cox regression analyses were performed including all database variables potentially associated with primary and secondary endpoints.
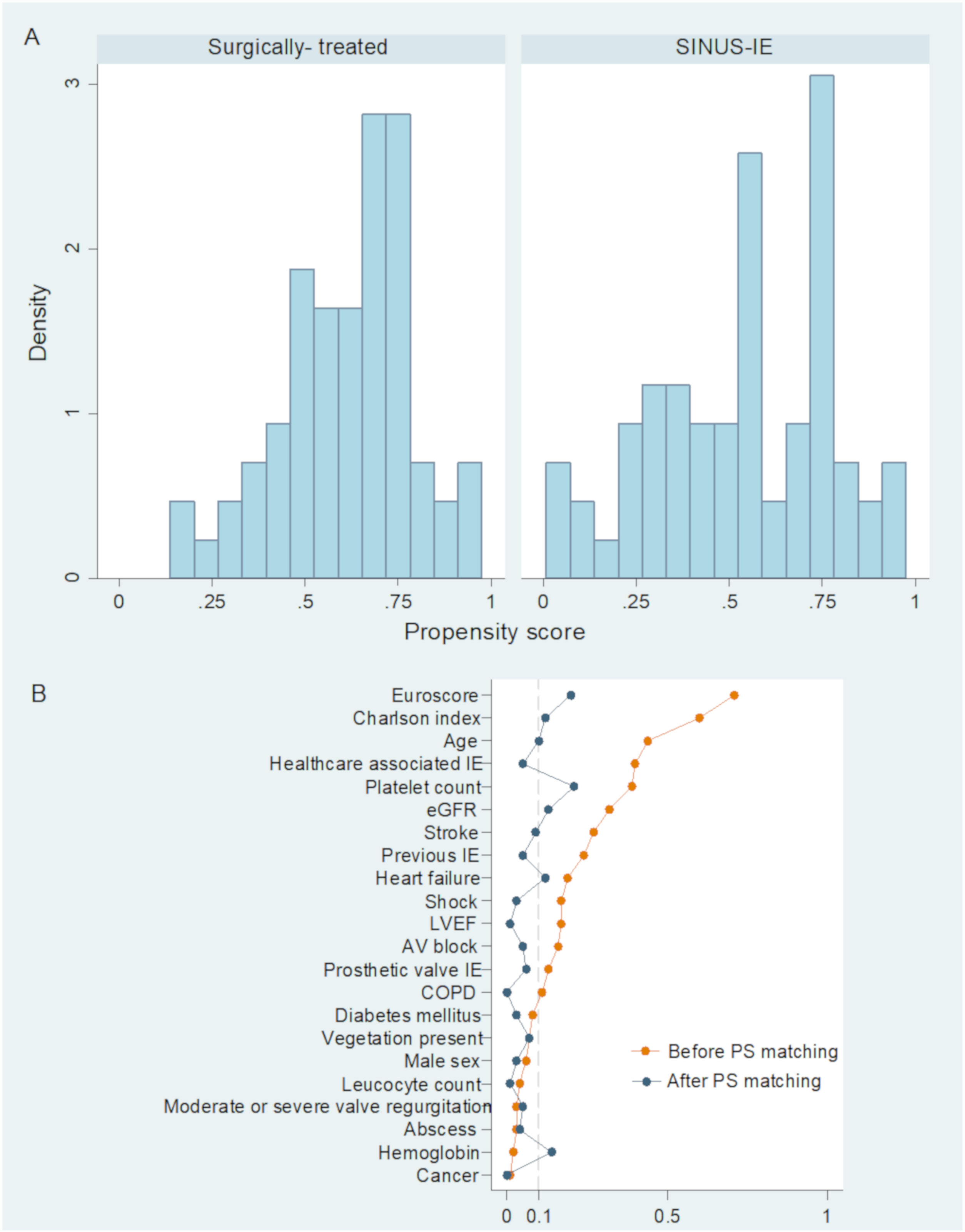
A multivariable Cox regression model was performed with adjustment for variables that were significantly associated with the outcome (P <.05) and other confounders. Covariates in the multivariable model for 60-day mortality were age, sex, health care-associated IE, unknown etiology, leukocyte count, platelet count, estimated glomerular filtration rate, heart failure, atrioventricular block, shock, Staphylococcus aureus infection, Enterococcus infection, and EuroSCORE. Covariates in the multivariable model for the secondary endpoint were age, sex, previous IE, coronary artery disease, diabetes mellitus, Charlson index, hemoglobin, estimated glomerular filtration rate, shock, Enterococcus infection, and EuroSCORE. Considering the difficulty of quantifying the prognostic impact of surgery in an unbiased manner, a propensity score analysis was also performed with a logistic regression model. The dependent variable was the performance of cardiac surgery for IE during the index hospitalization and a total of 24 covariates were selected (). The prediction accuracy of the logistic model was assessed with an area under the receiver-operating characteristic curve (c-statistic), which was 0.82.
According to the propensity score, patients were selected by 1:1 matching without replacement using the nearest neighbor method. A caliper width of 0.2 standardized differences was used for matching. Furthermore, we assessed the balance of the distribution of the baseline characteristics between the 2 groups by evaluating the absolute standardized differences. Among SINUS-LSIE patients, Cox regression analyses were used to identify variables associated with the 60-day mortality. Cumulative survival probability plots were generated. All comparisons of statistical significance were 2-sided, and a P value <.05 was considered significant. STATA V.13.0 (College Station, Texas, United States) was used for all analyses.
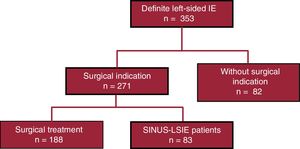
RESULTSBaseline characteristicsDuring the study period, 353 patients with LSIE were admitted to our institution and 271 had surgical indications and were included in the analysis. The flowchart of the study is depicted in figure 1. Median follow-up among survivors was 4.3 (2.3-8.4) years. The overall cohort included 201 (74.2%) males and the mean age was 64.3 years. Health care-associated IE was noted in 37.3% of patients and 96 (35.4%) had prosthetic valve IE. About 50% of our LSIE patients were transferred from other community hospitals. There was evidence of previous antibiotic administration in 28% of patients and in 65% of subjects with unknown etiology. The baseline characteristics of the surgical and nonsurgical patients (unmatched and propensity score matched cohorts) are detailed in table 1. Surgery was performed in 188 patients (53%), while 83 patients did not undergo surgical treatment despite having indications for it. SINUS-LSIE patients more frequently had a history of IE and health care-associated IE and had higher comorbidities as expressed by the Charlson index than patients who underwent surgical treatment. They also had greater deterioration of renal function and higher levels of C-reactive protein at admission. There were no differences between the groups regarding cardiac valvular involvement of IE, such as new moderate or severe aortic regurgitation, valve perforation, abscess, or paravalvular complications. Patients who underwent surgery were more likely to have infection caused by Streptococcus species in contrast to SINUS-LSIE patients who were more frequently infected with S. aureus. During admission, stroke and systemic embolization were more frequent in SINUS-LSIE patients. Severe valvular regurgitation, local complications, and heart failure were the main indications for cardiac surgery in both groups (). In SINUS-LSIE patients, the main reasons for the lack of surgery, despite indication, were high surgical risk (66.7%), death before surgery (13.1%), stroke (10.7%), and patient refusal (2.4%).
Baseline demographic, clinical, and microbiological characteristics of the study subjects
| Unmatched cohort | Matched cohort | ||||||
|---|---|---|---|---|---|---|---|
| Overall (n=271) | Surgery(n=188) | SINUS-LSIE(n=83) | P | Surgery(n=66) | SINUS-LSIE(n=66) | P | |
| Age, y | 64.3±13.7 | 62.5±12.8 | 68.4±14.9 | .001 | 66.8±11.4 | 68.3±14.2 | .514 |
| Male sex | 201 (74.2) | 141 (75) | 60 (72.3) | .638 | 48 (72.7) | 49 (74.3) | .844 |
| Health care-associated IE | 101 (37.3) | 59 (31.4) | 42 (50.6) | .003 | 31 (46.7) | 33 (50) | .728 |
| Prosthetic valve IE | 96 (35.4) | 63 (33.5) | 33 (39.8) | .322 | 27 (40.9) | 29 (43.9) | .725 |
| Clinical History | |||||||
| Previous IE | 16 (6.0) | 8 (4.3) | 8 (9.9) | .074 | 7 (10.6) | 6 (9.1) | .770 |
| Coronary artery disease | 48 (22.4) | 29 (19.5) | 19 (29.2) | .115 | 15 (25.9) | 16 (30.8) | .568 |
| COPD | 61 (22.5) | 45 (23.9) | 16 (19.3) | .397 | 13 (19.7) | 13 (19.7) | 1.000 |
| Diabetes mellitus | 81 (30.0) | 54 (28.9) | 27 (32.5) | .546 | 22 (33.3) | 21 (31.8) | .853 |
| Cancer | 32 (11.8) | 22 (11.7) | 10 (12.1) | .935 | 8 (12.1) | 8 (12.1) | 1.000 |
| HIV | 7 (2.6) | 3 (1.6) | 4 (4.8) | .123 | 3 (4.6) | 2 (3.0) | .648 |
| Charlson index | 2 [1-5] | 2 [1-4] | 4 [2-6] | <.001 | 3 [1-5] | 3 [2-6] | .482 |
| Laboratory tests | |||||||
| Leukocyte count, x 109/L | 12.2±6.6 | 12.1±6.5 | 12.4±7.1 | .718 | 12.5±7.5 | 12.5±7.5 | .952 |
| Hemoglobin, g/dL | 10.5±2.2 | 10.5±1.8 | 10.5±2.8 | .814 | 10.2±1.8 | 10.6±2.9 | .393 |
| Platelet count, x109/L | 214±105 | 226±102 | 186±106 | .003 | 199±92 | 178±104 | .208 |
| CRP, mg/L | 86 [41-148] | 82 [30-134] | 101 [48-181] | .033 | 85 [33-141] | 116 [50-175] | .168 |
| EGFR, mL/min/1.73m2 | 58.7±30.9 | 61.7±29.4 | 51.8±33.4 | .016 | 56.8±31.8 | 52.3±32.3 | .423 |
| Echocardiography | |||||||
| Vegetation present | 220 (82.1) | 151 (81.2) | 69 (84.1) | .560 | 52 (78.8) | 54 (81.8) | .662 |
| New moderate or severe valve regurgitation | 232 (89.6) | 161 (89.9) | 71 (88.8) | .771 | 56 (84.9) | 59 (89.4) | .436 |
| Perforation | 59 (21.8) | 45 (23.9) | 14 (16.9) | .194 | 8 (12.1) | 11 (16.7) | .457 |
| Abscess | 97 (35.8) | 68 (36.2) | 29 (34.9) | .846 | 27 (40.9) | 23 (34.9) | .473 |
| Fistula | 1 (0.4) | 1 (0.5) | 0 | .506 | 1 (1.5) | 0 | .315 |
| Dehiscence | 11 (4.1) | 8 (4.3) | 3 (3.6) | .805 | 1 (1.5) | 3 (4.6) | .310 |
| LVEF, % | 60.1±11.5 | 60.7±11.1 | 58.8±12.2 | .245 | 59.2±10.4 | 58.9±12.5 | .909 |
| Microbiology | |||||||
| Staphylococcus aureus | 97 (35.8) | 61 (32.5) | 36 (43.4) | .084 | 26 (39.4) | 29 (43.9) | .596 |
| Streptococcus species | 76 (28.0) | 59 (31.4) | 17 (20.5) | .066 | 15 (22.7) | 12 (18.2) | .517 |
| Enterococcus species | 43 (15.9) | 27 (14.4) | 16 (19.3) | .307 | 11 (16.7) | 13 (19.7) | .652 |
| Gram-negative | 8 (3.0) | 8 (4.3) | 0 | .056 | 2 (3.0) | 0 | .154 |
| Fungal | 5 (1.9) | 2 (1.1) | 3 (3.6) | .150 | 1 (1.5) | 3 (4.6) | .310 |
| Unknown | 32 (11.8) | 24 (12.8) | 8 (9.6) | .462 | 7 (10.6) | 6 (9.1) | .770 |
| Complications | |||||||
| Heart failure | 155 (60.6) | 111 (63.4) | 44 (54.3) | .166 | 37 (56.1) | 33 (50) | .485 |
| AV block | 35 (13.7) | 27 (15.4) | 8 (9.9) | .229 | 7 (10.6) | 6 (9.1) | .770 |
| Shock | 60 (23.4) | 37 (21.1) | 23 (28.4) | .203 | 21 (31.8) | 20 (30.3) | .851 |
| Stroke | 61 (22.5) | 30 (16.0) | 31 (37.4) | <.001 | 22 (33.3) | 23 (34.9) | .854 |
| Embolization | 151 (58.8) | 96 (54.6) | 55 (67.9) | .043 | 41 (62.1) | 45 (68.2) | .465 |
| EuroSCORE I, % | 20 [9-39] | 14 [7-28] | 34 [16-54] | <.001 | 25 [12-41] | 28 [15-47] | .304 |
| Outcome | |||||||
| 0 to 60-d mortality | 93 (34.3) | 40 (21.3) | 53 (63.9) | <.001 | 16 (24.2) | 40 (60.6) | <.001 |
| 61-d to 3-y mortality | 32 (11.8) | 21 (11.1) | 11 (13.3) | .624 | 11 (16.7) | 8 (12.1) | 0.457 |
AV, atrioventricular; COPD, chronic obstructive pulmonary disease; CRP, C reactive protein; EGFR, estimated glomerular filtration rate; HIV, human immunodeficiency virus; IE, infective endocarditis; LVEF, left ventricular ejection fraction; SINUS-LSIE, surgery-indicated not undergoing surgery patients with left-sided infective endocarditis.
Unless otherwise indicated, the data are presented as No. (%), mean±1 standard deviation, or median [interquartile range].
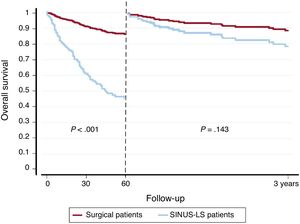
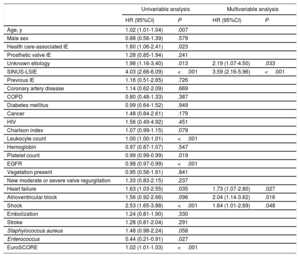
At the 60-day follow-up, 40 patients (21.3%) who underwent surgical treatment and 53 SINUS-LSIE patients (63.9%) died (P <.001, figure 2). From day 61 to the 3-year follow-up, 21 patients (11.1%) who underwent surgical treatment and 11 SINUS-LSIE patients (13.3%) died (P=.624). Among all surgery-indicated patients, multivariable Cox regression analyses showed that unknown etiology (hazard ratio [HR], 2.19; 95% confidence interval [95%CI], 1.07–4.50; P=.033), SINUS-LSIE (HR, 3.59; 95%CI, 2.16-5.96; P <.001), heart failure (HR, 1.73; 95%CI, 1.07-2.80; P=.027), atrioventricular block (HR, 2.04; 95%CI, 1.14-3.62; P=.016), and shock (HR, 1.64; 95%CI, 1.01–2.69; P=.048) were independent predictors of the occurrence of the primary endpoint (table 2).
Univariable and multivariable Cox regression analysis for 0- to 60-day mortality
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| HR (95%CI) | P | HR (95%CI) | P | |
| Age, y | 1.02 (1.01-1.04) | .007 | ||
| Male sex | 0.88 (0.56-1.39) | .579 | ||
| Health care-associated IE | 1.60 (1.06-2.41) | .023 | ||
| Prosthetic valve IE | 1.28 (0.85-1.94) | .241 | ||
| Unknown etiology | 1.98 (1.16-3.40) | .013 | 2.19 (1.07-4.50) | .033 |
| SINUS-LSIE | 4.03 (2.66-6.09) | <.001 | 3.59 (2.16-5.96) | <.001 |
| Previous IE | 1.16 (0.51-2.65) | .726 | ||
| Coronary artery disease | 1.14 (0.62-2.09) | .669 | ||
| COPD | 0.80 (0.48-1.33) | .387 | ||
| Diabetes mellitus | 0.99 (0.64-1.52) | .949 | ||
| Cancer | 1.48 (0.84-2.61) | .179 | ||
| HIV | 1.56 (0.49-4.92) | .451 | ||
| Charlson index | 1.07 (0.99-1.15) | .079 | ||
| Leukocyte count | 1.00 (1.00-1.01) | <.001 | ||
| Hemoglobin | 0.97 (0.87-1.07) | .547 | ||
| Platelet count | 0.99 (0.99-0.99) | .019 | ||
| EGFR | 0.98 (0.97-0.99) | <.001 | ||
| Vegetation present | 0.95 (0.56-1.61) | .841 | ||
| New moderate or severe valve regurgitation | 1.33 (0.83-2.15) | .237 | ||
| Heart failure | 1.63 (1.03-2.55) | .035 | 1.73 (1.07-2.80) | .027 |
| Atrioventricular block | 1.56 (0.92-2.66) | .096 | 2.04 (1.14-3.62) | .016 |
| Shock | 2.53 (1.65-3.88) | <.001 | 1.64 (1.01-2.69) | .048 |
| Embolization | 1.24 (0.81-1.90) | .330 | ||
| Stroke | 1.28 (0.81-2.04) | .291 | ||
| Staphylococcus aureus | 1.48 (0.98-2.24) | .058 | ||
| Enterococcus | 0.44 (0.21-0.91) | .027 | ||
| EuroSCORE | 1.02 (1.01-1.03) | <.001 | ||
95%CI, 95% confidence interval; COPD, chronic obstructive pulmonary disease; EGFR, estimated glomerular filtration rate; HIV, human immunodeficiency virus; HR, hazard ratio; IE, infective endocarditis; SINUS-LSIE, surgery-indicated not undergoing surgery patients with left-sided infective endocarditis.
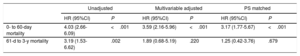
Similarly, and in multivariable model, the independent variables associated with all-cause death from day 61 to the 3-year follow-up were previous IE (HR, 15.54; 95%CI, 4.44-54.4; P <.001), diabetes mellitus (HR, 3.17; 95%CI, 1.13-8.90; P=.028), and the Charlson index (HR, 1.27; 95%CI, 1.07-1.51; P=.007), as shown in . Of note, mortality rates from day 61 to the 3-year follow-up were similar in surgically-treated and SINUS-LSIE patients (figure 2) and no significant differences in the risk of death between surgically-treated and SINUS-LSIE patients were found (HR, 1.89; 95%CI, 0.68-5.19; P=.220) (table 3). The characteristics of patients included in the long-term analysis are shown in .
Unadjusted and adjusted risk for short- and long-term mortality in surgery-indicated not undergoing surgery patients with left-sided infective endocarditis patients
| Unadjusted | Multivariable adjusted | PS matched | ||||
|---|---|---|---|---|---|---|
| HR (95%CI) | P | HR (95%CI) | P | HR (95%CI) | P | |
| 0- to 60-day mortality | 4.03 (2.66-6.09) | <.001 | 3.59 (2.16-5.96) | <.001 | 3.17 (1.77-5.67) | <.001 |
| 61-d to 3-y mortality | 3.19 (1.53-6.62) | .002 | 1.89 (0.68-5.19) | .220 | 1.25 (0.42-3.76) | .679 |
95%CI, 95% confidence interval; HR, hazard ratio; PS, propensity score.
Propensity score matching yielded 66 matched pairs of patients from the 2 groups. The distribution of created propensity score and the absolute standardized differences in the unmatched and matched patients are presented in . Risk of 60-day mortality was higher in SINUS-LSIE patients (HR, 3.17; 95%CI, 1.77-5.67; P <.001), but there were no significant differences in the risk of death from day 61 to the 3-year follow-up (HR, 1.25; 95%CI, 0.42-3.76; P=.679) (table 3).
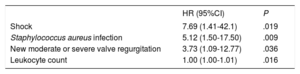
Predictors of short-term mortality in SINUS-LSIE patientsIn the subgroup of SINUS-LSIE patients and after multivariable Cox regression analysis, the variables independently associated with 60-day mortality were shock, S. aureus infection, new moderate or severe valve regurgitation, and leukocyte count (table 4). Exploratory analyses of SINUS-LSIE patients infected by S. aureus showed that this infection was more frequently related to health care-associated IE ().
Variables independently associated with 60-day mortality among surgery-indicated not undergoing surgery patients with left-sided infective endocarditis patients
| HR (95%CI) | P | |
|---|---|---|
| Shock | 7.69 (1.41-42.1) | .019 |
| Staphylococcus aureus infection | 5.12 (1.50-17.50) | .009 |
| New moderate or severe valve regurgitation | 3.73 (1.09-12.77) | .036 |
| Leukocyte count | 1.00 (1.00-1.01) | .016 |
95%CI, 95% confidence interval; HR, hazard ratio.
The present study describes the clinical characteristics and evaluates the short- and long-term prognoses of LSIE patients with surgical indications. The main finding was that nearly one-third of these patients do not undergo surgery during their initial hospitalization. These SINUS-LSIE patients are at increased risk of mortality in the short-term compared with surgically-treated patients, but with similar rates of death from day 61 to the 3-year follow-up.
We found that the 60-day mortality rate was 34.3% in all LSIE patients with surgical indications. This is a higher proportion than that reported in other studies that estimated in-hospital mortality rates from 15% to 20%.14,24,25 This difference could be explained by the widely-described epidemiological changes in IE over time.8,9,26 These changes include higher rates of health care-related episodes22,27 and largely involve frail patients with multiple comorbidities who have an inherently high risk of death, regardless of the type of IE and treatment received.
Consensus guidelines outline specific conditions for which surgery is recommended.21 Decisions about surgical interventions are complex and, although cardiac surgery can be life-saving, it also carries significant risk. Thus, surgery is sometimes withheld, even when indicated, due to severe comorbidities or severe multiorgan failure at the time of the decision. Remarkably, in our study, SINUS-LSIE patients represented 30.6% of all patients with surgical indications, well within the range reported by others (24% reported in the study by Chu et al.13 and 45% reported in the study by Fernández-Hidalgo et al.14). The clinical profile of SINUS-LSIE patients is characterized by older patients, higher comorbidities, worse renal function, and more frequent stroke and embolization. The combination of all these patient-related factors and clinical complications give rise to a prohibitive surgical risk resulting in non-performance of surgery in these patients. Consequently, the short-term prognosis among SINUS-LSIE patients is poor (up to 64% mortality in our cohort).
The decision to perform early surgery in IE has always been a challenge; however, there is growing evidence suggesting that early surgical intervention in IE increases short-term survival when compared with conservative management and/or delayed surgery.28,29 Traditional cardiac surgery scores (STS, EuroSCORE) are not specific or accurate for IE, and previous studies have reported conflicting results.17,19,30,31 These findings indicate that new research is needed to assess operative risk to aid clinical decisions regarding surgical treatment in LSIE.
The role of early surgery as a prognostic factor for long-term survival is controversial.24,32 Contemporary studies show a potential benefit of early surgery13,14,20,33 on mid- and long-term mortality compared with a medically-treated group. Other studies have demonstrated higher mortality rates in IE patients beyond the index hospitalization predominantly due to noncardiac conditions.34–36 In our study, we found no differences in mortality beyond day 60 of discharge between surgically-treated and SINUS-LSIE patients and we found that diabetes mellitus, Charlson index, and a previous history of IE were independent predictors of long-term mortality. These findings support the hypothesis that long-term prognosis depends more on host conditions and comorbidities than on the treatment received during admission.17,37,38 Some of the SINUS-LSIE patients who survived beyond 60 days could benefit from prolonged treatment with suppressive antibiotics. The role of oral antibiotic therapy in left-sided IE is not well established. Oral antibiotics appear effective for shortening intravenous treatment in selected cases of uncomplicated left-sided IE.39 There is a lack of information regarding long-term suppressive antibiotic treatment among SINUS-LSIE patients with only 1 description of case reports40 and brief mentions of such treatment in some contemporary series.7,14 In this setting, as previously reported,41,42 a multidisciplinary approach has been shown to improve in-hospital and short-term mortality in native IE with less evidence on long-term outcomes on prosthetic valve IE.43 A managed-based approach with close follow-up and individualized treatment could be of special relevance in this SINUS-LSIE cohort to improve long-term prognosis.
Among all the patients with surgical indications, we also found that the absence of microbiological diagnosis is an independent predictor of short-term mortality. Likewise, Díez Vilanueva et al.44 previously reported that the absence of microbiological diagnosis is an independent predictor of in-hospital mortality due to delayed diagnosis and difficulty in determining adequate treatment. Not surprisingly, among SINUS-LSIE patients, S. aureus infection was independently associated with a worse short-term outcome. This is a relevant finding considering that S. aureus has become the predominant species responsible for IE in developed countries45 and is frequently associated with lower rates of surgery due to hemodynamic or end-organ complications that increase surgical risk.13
Our present study has some limitations. First, some patients were transferred to our tertiary center and their data may be affected by referral bias. Second, we only included patients rejected for surgery in the index hospitalization and not patients with complications or surgical indications who were rejected for surgery in the follow-up. Third, the mode of death was not recorded; consequently, estimates of the proportion of cardiovascular death are lacking. Finally, the major limitation in the assessment of the prognostic impact of surgical treatment in this clinical setting lies in the difficulty of obtaining an unbiased estimate of this effect despite the statistical adjustment performed.
CONCLUSIONSIn this study, performed in a contemporary cohort of LSIE patients with surgical indications, nearly one third of patients did not undergo surgery during the initial hospitalization. SINUS-LSIE patients were at higher risk of short-term mortality than surgically-treated patients but had similar rates of death from day 61 to the 3-year follow-up. A multidisciplinary approach in this population is crucial and should be considered mandatory for these patients with severe comorbidities. More studies are needed to determinate real operative risk among these patients concerning long-term outcome, which could help in the decision to perform surgery.
FUNDINGA. Bayés-Genís was supported by grants from the Ministerio de Educación y Ciencia (SAF2014–59892), Fundació La MARATÓ de TV3 (201502, 201516), CIBER Cardiovascular (CB16/11/00403), and AdvanceCat 2014.
CONFLICTS OF INTERESTNone declared.
- –
Previous studies have evaluated clinical risk factors for mortality in IE without addressing surgical indication. The role of surgery in IE is controversial, especially concerning long-term mortality. Risk scores and surgical criteria take into account in-hospital mortality.
- –
A multidisciplinary approach has been shown to improve prognosis in IE.
- –
This study, performed in a Spanish tertiary hospital with an IE team and close multidisciplinary follow-up, provides the most detailed information available on patients with surgical indication not undergoing surgery.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.09.011