The present article reports the characteristics and results of heart transplants in Spain since this therapeutic modality was first used in May 1984.
MethodsWe describe the main features of recipients, donors, surgical procedures, and results of all heart transplants performed in Spain until December 31, 2015.
ResultsA total of 299 cardiac transplants were performed in 2015, with the whole series comprising 7588 procedures. The main transplant features in 2015 were similar to those observed in recent years. A remarkably high percentage of transplants were performed under emergency conditions and there was widespread use of circulatory assist devices, particularly continuous-flow left ventricular assist devices prior to transplant (16% of all transplants). Survival has significantly improved in the last decade compared with previous time periods.
ConclusionsDuring the last few years, between 250 and 300 heart transplants have consistently been performed each year in Spain. Despite a more complex clinical context, survival has increased in recent years.
Keywords
Since 1991, the Spanish Heart Transplantation Registry (Registro Español de Trasplante Cardiaco [RETC]) has published an annual description of the clinical and surgical characteristics and general results of all heart transplant procedures performed in Spain1–26. The current article reports data on the transplant population until 31 December 2015. As is already well-known, the main strength of the RETC lies in its inclusion and comprehensive updating of all heart transplant procedures performed in all Spanish hospitals since May 1984, regardless of the procedural characteristics and results. In addition, data collection is prospectively performed using a shared database developed and updated by all transplant teams.
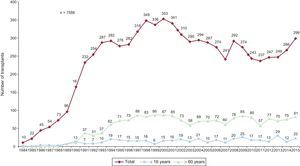
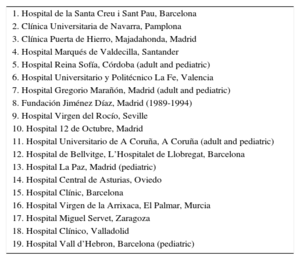
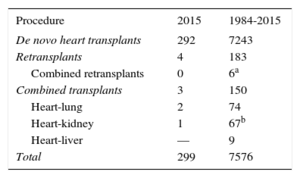
METHODSPatients and CentersOf the 19 centers that have contributed data to the RETC, 18 are currently active (Table 1). Two centers are entirely dedicated to pediatric transplantation while another 3 perform both pediatric and adult transplantation. The numbers of procedures performed annually are summarized in Figure 1. The whole series comprises 7588 procedures. Data were lost on 12 patients, including follow-up information. These patients have been omitted from the analysis, giving a final sample size of 7576 patients. Of the 299 procedures performed in 2015, 22 (7.4%) were performed in pediatric patients (age<16 years). The types of procedures performed in 2015 and in the whole series are summarized in Table 2.
Centers (by Order of First Transplantation Performed) Participating in the Spanish Heart Transplantation Registry (1984-2015)
| 1. Hospital de la Santa Creu i Sant Pau, Barcelona |
| 2. Clínica Universitaria de Navarra, Pamplona |
| 3. Clínica Puerta de Hierro, Majadahonda, Madrid |
| 4. Hospital Marqués de Valdecilla, Santander |
| 5. Hospital Reina Sofía, Córdoba (adult and pediatric) |
| 6. Hospital Universitario y Politécnico La Fe, Valencia |
| 7. Hospital Gregorio Marañón, Madrid (adult and pediatric) |
| 8. Fundación Jiménez Díaz, Madrid (1989-1994) |
| 9. Hospital Virgen del Rocío, Seville |
| 10. Hospital 12 de Octubre, Madrid |
| 11. Hospital Universitario de A Coruña, A Coruña (adult and pediatric) |
| 12. Hospital de Bellvitge, L’Hospitalet de Llobregat, Barcelona |
| 13. Hospital La Paz, Madrid (pediatric) |
| 14. Hospital Central de Asturias, Oviedo |
| 15. Hospital Clínic, Barcelona |
| 16. Hospital Virgen de la Arrixaca, El Palmar, Murcia |
| 17. Hospital Miguel Servet, Zaragoza |
| 18. Hospital Clínico, Valladolid |
| 19. Hospital Vall d’Hebron, Barcelona (pediatric) |
The database comprises 175 clinical variables, established by consensus among all the teams, and records data on recipients, donors, surgical techniques, immunosuppression, and follow-up. Since 2013, the data have been electronically introduced and updated in real time using a web-based program specifically designed for this purpose. The database support is a Microsoft Excel file. This procedure replaces the previous method, in which each center sent data to the registry director in Microsoft Access file format via email. An external CRO (contract research organization), currently ODDS S.L., performed database maintenance, quality control, and statistical analysis.
Ethics committee approval, auditing, and registration with the Ministry of Health were performed in accordance with the Spanish Organic Law on Data Protection 15/1999.
StatisticsContinuous quantitative variables are presented as mean ± standard deviation; categorical variables are presented as percentages. The results are categorized according to the year of transplantation and the total sample has been divided into 4 time periods (1984-1993, 1994-2003, 2004-2013, and 2014-2015). Some variables were also analyzed according to the annual data from the whole series, such as donor age, emergency transplants, and ischemia time. Differences among groups were analyzed using a nonparametric test for temporal trends (Kendall τ) for categorical variables and analysis of variance test with polynomial fit for continuous variables. Survival curves were calculated using the Kaplan-Meier test and were compared using a log rank test. A P value <.05 was considered statistically significant.
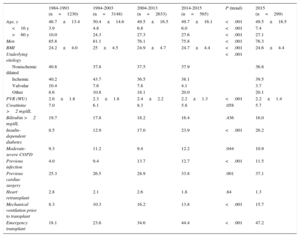
RESULTSRecipient CharacteristicsIn 2015, the recipients had a mean age of 49.5±16.5 years (range, 0.14-73 years); 76% were men, with the following underlying diagnoses: ischemic cardiomyopathy (21.4%), nonischemic dilated cardiomyopathy (30.4%), valvular heart disease (4.0%), and other etiologies (44.2%). Recipient characteristics by transplant period are summarized in Table 3. There were significant trends toward older recipients, female sex, atypical causes of underlying heart disease, and an increase in pretransplant conditions with known prognostic effects, such as insulin-dependent diabetes mellitus, infection, cardiac surgery, and mechanical ventilation prior to transplant. Although the difference was not statistically significant, the proportion of retransplants fell below 2% in 2014-2015, comprising 2.4% of the total series. In contrast, there was a significant decrease in pretransplant values of pulmonary vascular resistance and an almost significant decrease in pretransplant severe renal dysfunction throughout the time series.
Recipient Characteristics in the Spanish Heart Transplantation Registry (1984-2015)
| 1984-1993 (n=1230) | 1994-2003 (n=3148) | 2004-2013 (n=2633) | 2014-2015 (n=565) | P (trend) | 2015 (n=299) | |
|---|---|---|---|---|---|---|
| Age, y | 46.7±13.4 | 50.4±14.6 | 49.5±16.5 | 49.7±16.1 | <.001 | 49.5±16.5 |
| <16 y | 3.9 | 4.8 | 6.8 | 6.0 | <.001 | 7.4 |
| >60 y | 10.0 | 24.3 | 27.3 | 27.6 | <.001 | 27.1 |
| Men | 85.8 | 81.1 | 76.1 | 75.8 | <.001 | 76.3 |
| BMI | 24.2±4.0 | 25±4.5 | 24.9±4.7 | 24.7±4.4 | <.001 | 24.6±4.4 |
| Underlying etiology | <.001 | |||||
| Nonischemic dilated | 40.8 | 37.8 | 37.5 | 37.9 | 36.8 | |
| Ischemic | 40.2 | 43.7 | 36.5 | 38.1 | 39.5 | |
| Valvular | 10.4 | 7.6 | 7.8 | 4.1 | 3.7 | |
| Other | 8.6 | 10.8 | 18.1 | 20.0 | 20.1 | |
| PVR (WU) | 2.6±1.8 | 2.3±1.8 | 2.4±2.2 | 2.2±1.3 | <.001 | 2.2±1.4 |
| Creatinine >2 mg/dL | 7.0 | 6.1 | 8.3 | 5.8 | .058 | 5.7 |
| Bilirubin >2 mg/dL | 19.7 | 17.8 | 18.2 | 16.4 | .436 | 16.0 |
| Insulin-dependent diabetes | 8.5 | 12.9 | 17.0 | 23.9 | <.001 | 26.2 |
| Moderate-severe COPD | 9.3 | 11.2 | 9.4 | 12.2 | .044 | 10.9 |
| Previous infection | 4.0 | 9.4 | 13.7 | 12.7 | <.001 | 11.5 |
| Previous cardiac surgery | 25.3 | 26.5 | 28.9 | 33.8 | .001 | 37.1 |
| Heart retransplant | 2.8 | 2.1 | 2.6 | 1.8 | .84 | 1.3 |
| Mechanical ventilation prior to transplant | 8.3 | 10.3 | 16.2 | 13.8 | <.001 | 15.7 |
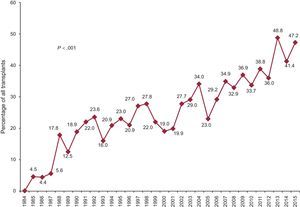
| Emergency transplant | 18.1 | 23.6 | 34.6 | 44.4 | <.001 | 47.2 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; PVR, pulmonary vascular resistance.
The values in the Underlying etiology section were obtained from previous reports due to updating of the database and recoding of the various categories. Values expressed are percentages or mean±standard deviation.
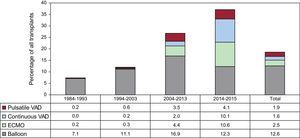
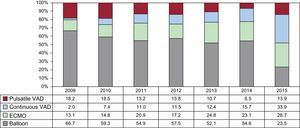
Compared with 2014, there was a slight uptick in 2015 in emergency transplants, reaching almost half of all procedures. Thus, the use of emergency transplants has remained above 40% since 2013 (Figure 2). In 2015, there was another increase in the use of ventricular assist devices prior to transplantation, whose use was first recorded in 2009 (P<.001) (Figure 3). Moreover, there was increased use of continuous-flow left ventricular assist devices (33.9%) and reduction of almost one-half in the use of balloon pumps vs 2014 (Figure 4).
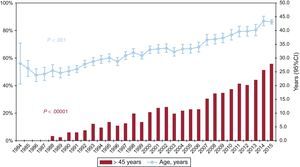
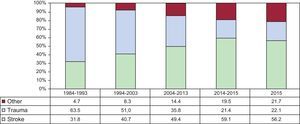
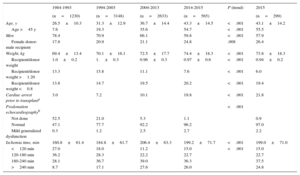
The characteristics of the donors in 2015 and according to time interval are summarized in Table 4. Donor age has been significantly increasing throughout the series, with 55% of donors considered suboptimal (age >45 years) in 2015 (Figure 5). There has been an increase in female donors and the percentage of female-to-male transplants (26.4%), as well as cardiac arrest prior to donation (21.8% in 2015). In addition, there was an increase in donors who died from stroke, with a consequent decrease in deaths from trauma (Figure 6).
Donor Characteristics and Ischemia Times in the Spanish Heart Transplantation Registry (1984-2015)
| 1984-1993 | 1994-2003 | 2004-2013 | 2014-2015 | P (trend) | 2015 | |
|---|---|---|---|---|---|---|
| (n=1230) | (n=3148) | (n=2633) | (n=565) | (n=299) | ||
| Age, y | 26.5±10.3 | 31.3±12.9 | 36.7±14.4 | 43.3±14.5 | <.001 | 43.1±14.2 |
| Age >45 y | 7.6 | 19.3 | 35.6 | 54.7 | <.001 | 55.5 |
| Men | 78.4 | 70.9 | 66.1 | 59.8 | <.001 | 57.9 |
| Female donor-male recipient | 17.8 | 20.9 | 21.1 | 24.8 | .008 | 26.4 |
| Weight, kg | 69.4±13.4 | 70.1±16.1 | 72.5±17.7 | 74.4±18.3 | <.001 | 73.8±18.3 |
| Recipient/donor weight | 1.0±0.2 | 1.±0.3 | 0.96±0.3 | 0.97±0.6 | <.001 | 0.94±0.2 |
| Recipient/donor weight >1.20 | 13.3 | 15.8 | 11.1 | 7.6 | <.001 | 6.0 |
| Recipient/donor weight <0.8 | 13.8 | 14.7 | 19.5 | 20.2 | <.001 | 19.4 |
| Cardiac arrest prior to transplanta | 3.0 | 7.2 | 10.1 | 19.8 | <.001 | 21.8 |
| Predonation echocardiographyb | <.001 | |||||
| Not done | 52.5 | 21.0 | 5.3 | 1.1 | 0.9 | |
| Normal | 47.1 | 77.7 | 92.2 | 96.2 | 97.0 | |
| Mild generalized dysfunction | 0.3 | 1.2 | 2.5 | 2.7 | 2.2 | |
| Ischemia time, min | 160.8±61.4 | 184.8±61.7 | 206.4±63.3 | 199.2±71.7 | <.001 | 199.0±71.0 |
| <120 min | 27.0 | 18.0 | 11.2 | 15.0 | <.001 | 15.0 |
| 120-180 min | 36.2 | 28.3 | 22.2 | 22.7 | 22.7 | |
| 180-240 min | 28.1 | 36.7 | 39.0 | 36.3 | 37.5 | |
| >240 min | 8.7 | 17.1 | 27.6 | 26.0 | 24.8 |
Values expressed are percentages or mean±standard deviation.
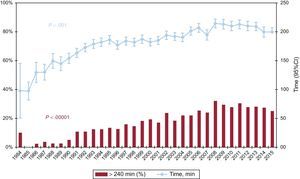
Ischemia time has increased throughout the time series. In 2015, as in the previous decade, the ischemia time was greater than 240min in about a quarter of recipients (Table 4 and Figure 7).
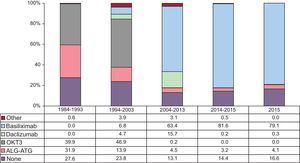
ImmunosuppressionIn 2015, 83.4% of recipients received some type of induction immunosuppressive therapy, mainly involving basiliximab (79.1%) (Figure 8), confirming the tendency observed since 2009.
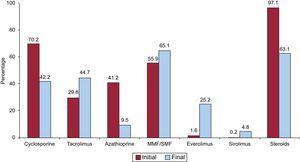
The drugs used in the initial immunosuppression and at the end of follow-up for the whole series are summarized in Figure 9. In a mean follow-up of 7.2 years, 63.1% of patients continued to receive corticoid therapy. At last follow-up, 30% of patients were under treatment with mTor inhibitors (everolimus or sirolimus).
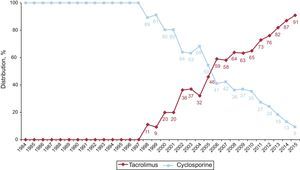
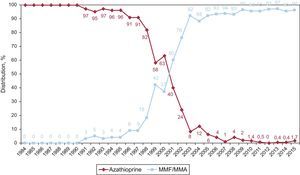
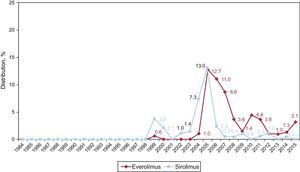
In 2015, initial immunosuppression predominantly consisted of tacrolimus (89.3%) as the calcineurin inhibitor, mycophenolate mofetil or mycophenolic acid (98.3%) as the antiproliferative agent, and steroids (98.3%). The annual changes in the use of the various calcineurin inhibitors and antimitotics are shown in Figure 10 and Figure 11, respectively. The annual changes in the use of the mTor inhibitors (sirolimus, everolimus) in the initial immunosuppression are shown in Figure 12.
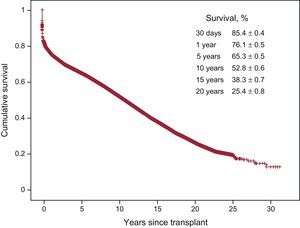
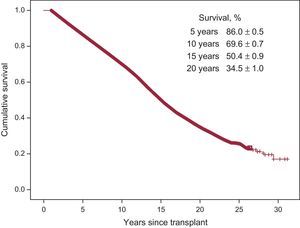
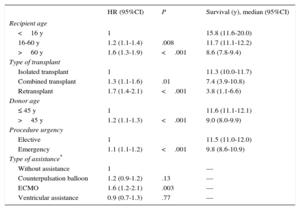
With the most recent update from December 31, 2015, the 1-, 5-, 10-, 15-, and 20-year actuarial survivals in the entire time series are summarized in Figure 13. The survival curves indicate a mean annual mortality of about 2% to 3% after the first posttransplant year, with a median survival of 11.1 years. The 1-year conditional survival is shown in Figure 14. The conditional median survival after the first posttransplant year was 15.1 years. There were significant differences according to recipient age, donor age, type of procedure (isolated transplant, combined transplant, and retransplant), transplanturgency, and type of circulatory assistance at the time of transplant (without assistance, balloon pump, extracorporeal membrane oxygenation [ECMO], ventricular assist device). The most notable finding was the similar survival between elective transplants and transplants performed with balloon pump or ventricular assist devices. Transplants performed with prior ECMO showed significantly worse survival than those performed with no such device.
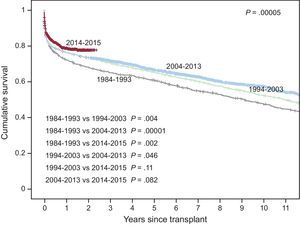
The survival results have constantly improved throughout the time series (Figure 15). Compared with the 1984 to 1993 decade, there were highly significant differences with the second decade and the period 2014 to 2015. Compared with the first decade, there was improved survival in the first posttransplant year in the following 2 decades. Compared with procedures performed between 1993 and 2013, there was an additional improvement in 1-year survival in 2014 and 2015 (Table 5). The improved survival in the 2004 to 2013 decade vs 1994 to 2014 was observed at a longer term (from the second posttransplant year) (Figure 15). The median survival improvement is continuous: 9.1 years (1984-1993), 10.9 years (1994-2003), and 12.0 years (2004-2013). In addition, the 2014 to 2015 period shows a clear tendency for improved survival vs the previous decade (2004-2013), even if this result is not statistically significant due to the relatively small sample size of the later group.
Univariable Survival Analysis by Baseline Characteristics of the Recipient, Donor, and Procedure (1984-2015)
| HR (95%CI) | P | Survival (y), median (95%CI) | |
|---|---|---|---|
| Recipient age | |||
| <16 y | 1 | 15.8 (11.6-20.0) | |
| 16-60 y | 1.2 (1.1-1.4) | .008 | 11.7 (11.1-12.2) |
| >60 y | 1.6 (1.3-1.9) | <.001 | 8.6 (7.8-9.4) |
| Type of transplant | |||
| Isolated transplant | 1 | 11.3 (10.0-11.7) | |
| Combined transplant | 1.3 (1.1-1.6) | .01 | 7.4 (3.9-10.8) |
| Retransplant | 1.7 (1.4-2.1) | <.001 | 3.8 (1.1-6.6) |
| Donor age | |||
| ≤ 45 y | 1 | 11.6 (11.1-12.1) | |
| >45 y | 1.2 (1.1-1.3) | <.001 | 9.0 (8.0-9.9) |
| Procedure urgency | |||
| Elective | 1 | 11.5 (11.0-12.0) | |
| Emergency | 1.1 (1.1-1.2) | <.001 | 9.8 (8.6-10.9) |
| Type of assistance* | |||
| Without assistance | 1 | — | |
| Counterpulsation balloon | 1.2 (0.9-1.2) | .13 | — |
| ECMO | 1.6 (1.2-2.1) | .003 | — |
| Ventricular assistance | 0.9 (0.7-1.3) | .77 | — |
95%CI, 95% confidence interval; ECMO, extracorporeal membrane oxygenation; HR, hazard ratio.
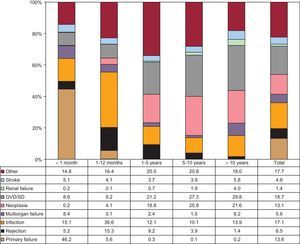
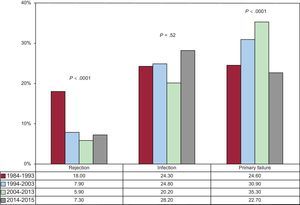
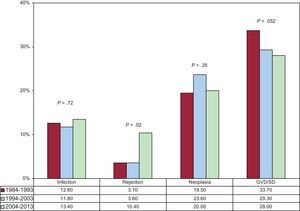
In the total population, the most frequent cause of death was graft vascular disease/sudden death (18.7%), followed by infections (17.1%), primary graft failure (13.6%), and neoplasia (13.1%) (Figure 16). The causes of death depended on the time after transplant (Figure 16). In the first posttransplant month, almost 50% of deaths were due to primary graft failure. After the first month and until 1 year, acute rejection (15.3%) and, above all, infections (36.6%) were the main causes of death. After the first year, the main causes were various manifestations of graft vascular disease (30.2%) and tumors (22.0%). The main causes of death in the first year have changed significantly over time, with fewer deaths due to acute rejection and more deaths due to primary graft failure, even if the latter decreased in the 2014 to 2015 period (Figure 17). In deaths occurring between the first and fifth posttransplant years, there was a tendency for fewer deaths due to graft vascular disease/sudden death and significantly more deaths due to acute rejection (Figure 18).
With the historical perspective provided by more than 30 years of RETC activity, with data on practically all heart transplant recipients in Spain, the most important finding of this registry is the change in the survival results. After the improved early survival in the second decade of activity (1994-2003), which was maintained in the subsequent decade (2004-2013), there has been an additional improvement in the last 2 years, with 1-year survival rates close to 80%. In addition, the improvement has been constant in the mid- to long-term, and it is hoped that this improvement will be maintained, given the tendency of the 2014 to 2015 curve. Both the values and the tendencies practically mirror those published by the registry of the International Society for Heart and Lung Transplantation for the 1982 to 2013 period27. Nonetheless, despite including more than 100 000 patients from the entire world, this registry has a selection bias, in contrast to the RETC, because information is not collected on all patients due to its voluntary nature.
The notable survival improvement in the RETC has been obtained in the context of growing recipient, donor, and surgical procedure complexity and has been maintained since about 2009. Accordingly, the high percentage of transplants performed under emergency conditions (practically half of all procedures) is interesting, as well as the growing use of circulatory assist devices. In 2015, less than a quarter of all emergency transplants were performed with a balloon pump, a supportive measure that predominated until 2014. The use of ECMO prior to transplant has been largely stable since 2013, with a doubling in the use of continuous-flow left ventricular assist devices. Although the need for pretransplant circulatory support and the use of ECMO as a supportive measure increases early mortality, the prudent use of continuous-flow left ventricular assist devices and appropriate care of recipients receiving them is probably responsible for the decreased early mortality from primary graft failure. This factor would explain why the short- and mid-term survival is statistically similar for elective transplants and transplants performed with the prior use of these last devices.
Another interesting observation is that the improved survival in recent periods is not only due to improvements in early mortality (in the first year). Conditional survival curves show a separation from the second year, a trend that seems to be accentuated for patients transplanted in the last 2 years, although a longer clinical course is required to confirm this finding. The cause of this observation is undoubtedly multifactorial but there was a notable decrease in mid-term deaths due to graft vascular disease in more recent periods.
CONCLUSIONSHeart transplant activity has been stable in Spain in recent years, with about 250 procedures per year. Despite the worsening of the current clinical setting and its growing complexity (eg, increased use of suboptimal donors and circulatory support), Spanish transplant teams have managed to maintain the mortality results and to progressively improve the mid-term prognosis.
FUNDINGThe RETC is partially funded by an unconditional grant from Novartis.
CONFLICTS OF INTERESTF. González-Vílchez receives remuneration for participating in the Comité de Control y Análisis Estadístico from Roche and Astellas, remuneration for educational presentations and travel expenses from Roche, Astellas, and Novartis, and unconditional support from the Instituto de Investigación Marqués de Valdecilla.
We appreciate the statistical support of ODDS, S.L. Many of the researchers and participating centers are part of the Red de Investigación Cardiovascular of the Instituto de Salud Carlos III.
| Clínica Universitaria Puerta de Hierro, Majadahonda, Madrid | Manuel Gómez-Bueno, Francisco Hernández-Pérez, Luis Alonso-Pulpón, Alberto Forteza-Gil, Santiago Serrano-Fiz, Raúl Burgos-Lázaro, Carlos García-Montero, Evaristo Castedo-Mejuto |
| Hospital Universitario y Politécnico La Fe, Valencia | Ignacio Sánchez-Lázaro, Luis Martínez-Dolz, Mónica Cebrián-Pinar, Soledad Martínez-Penades |
| Hospital Universitario de A Coruña, A Coruña | María J. Paniagua-Martin, Eduardo Barge-Caballero, Jose J. Cuenca-Castillo, Francisco Estevez-Cid, Gonzalo Barge-Caballero |
| Hospital Universitario Reina Sofía, Córdoba | Amador Lopez-Granados, Juan Carlos Castillo-Diéguez |
| Hospital Universitario Marqués de Valdecilla, Santander | Manuel Cobo, Miguel Llano-Cardenal, José A. Vázquez de Prada, Francisco Nistal-Herrera |
| Hospital Gregorio Marañón (adults), Madrid | Paula Navas, Eduardo-Zataraín, Juan Fernández-Yáñez, Adolfo-Villa, Manuel Martínez-Sellés |
| Hospital Universitario Doce de Octubre, Madrid | Miguel Ángel Gómez-Sánchez, Laura Morán-Fernández |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Viçens Brossa, Sònia Mirabet, Laura López |
| Hospital Universitario Virgen del Rocío, Seville | Ernesto Lage-Gallé, Diego Rangel-Sousa |
| Hospital Universitario de Bellvitge, L’Hospitalet de Llobregat, Barcelona | Nicolás Manito, Josep Roca-Elías, Joel Salazar-Mendiguchía |
| Clínica Universitaria de Navarra, Pamplona | Cristian Delgado-Domínguez, Ignacio Bibiloni-Lage |
| Hospital Clínic Universitari, Barcelona | M. Ángeles Castel, Marta-Farrero, Ana García-Álvarez |
| Hospital Universitario Central de Asturias, Oviedo | José Luis Lambert, Beatriz Díez de Molina, María José Bernardo-Rodríguez |
| Hospital Universitario Gregorio Marañón (pediatric), Madrid | Manuela Camino, Constancio Medrano |
| Hospital Universitario Virgen de la Arrixaca, Murcia | Domingo Pascual-Figal, Iris Garrido-Bravo, Francisco Pastor-Pérez |
| Hospital Universitario Miguel Servet, Zaragoza | Teresa Blasco-Peiró, Marisa Sanz-Julvé, Ana Pórtoles-Ocampo |
| Hospital Clínico Universitario, Valladolid | Luis de la Fuente-Galán, Javier López-Díaz, Ana María Correa Fernández |
| Hospital Universitario La Paz, Madrid | Luis García-Guereta, Luz Polo, Carlos Labrandero |
| Hospital Universitario Vall d’Hebron, Barcelona | Dimpna C. Albert-Brotons, Ferrán Gran-Ipiña, Raúl Abella |