Unless contraindicated, the treatment of choice for ST-segment elevation acute coronary syndrome (STEACS) is dual antiplatelet therapy with aspirin and a potent P2Y12 platelet receptor antagonist. Acute complications of STEACS include infarction-related complications (heart failure, mechanical complications, and arrhythmias) and early stent thrombosis. Complications from dual antiplatelet therapy are not uncommon, and the risk of gastrointestinal and intracranial bleeding is a particular concern. We describe the case of a patient who developed spontaneous spinal epidural hematoma during treatment with aspirin and ticagrelor.
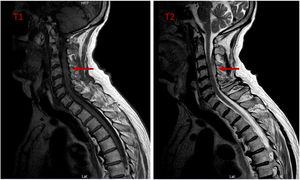
The patient, who provided verbal consent for the publication of this report, was a 69-year-old hypertensive, dyslipidemic man admitted with previously untreated posterior STEACS, Killip class I. Coronary angiography showed a critical lesion in the proximal circumflex artery, which was revascularized with a drug-eluting stent. The patient was administered 8000 IU of unfractionated heparin, 300mg of aspirin, and 180mg of ticagrelor. This was followed by aspirin 100mg/d and ticagrelor 90mg/12 h. Forty-eight hours after stent placement, the patient's kidney function deteriorated to Acute Kidney Injury Network class II due to contrast agent-induced nephrotoxicity. On day 5, while awaiting discharge and with a normal-functioning kidney, the patient developed intense nontraumatic interscapular pain radiating to the upper left leg and worsening with cervical movement. He was conscious and had adequate oxygen perfusion and saturation values, a heart rate of 60 bpm, and a blood pressure of 180/110 mmHg. His blood pressure had been normal on the previous days even though he had not been restarted on hypertensive medication because of the kidney failure. An electrocardiogram and transthoracic echocardiogram ruled out acute changes and mechanical complications. The results of abdominal and neurological examinations were also normal. The patient was administered intravenous analgesia, which partly relieved the pain and lowered his blood pressure to 100/60mmHg. Just minutes later, he developed progressive paresis in his arms and legs and general hyporeflexia without sensory dysfunction. He was started on fluid therapy and noradrenaline to treat the markedly low blood pressure. Once stable, he underwent computed angiography of the brain, chest, and abdomen, which showed hyperdense material consistent with epidural hematoma in the cervical spinal canal. Emergency magnetic resonance imaging (MRI) of the spine confirmed the presence of epidural hematoma in the posterior region extending from C2-C3 to C5-C6 and compressing the anterior cord (figure 1). The patient was treated with emergency laminectomy, hematoma evacuation, and control of epidural bleeding. No vascular lesions or malformations that could explain the bleeding were identified.
Several diagnoses were considered as the patient's condition progressed. The initial observation of radiating interscapular pain in a recently revascularized patient suggested early stent thrombosis, but this was ruled out by the electrocardiographic and echocardiographic findings. Muscle contracture was also contemplated as the pain had mechanical characteristics, but this possibility was rejected because of the intensity of the pain and the subsequent hemodynamic and neurological manifestations. The shooting back pain combined with hypertension followed by hypotension and neurological involvement led us to consider the possibility of acute aortic dissection with spinal cord ischemia and, as was ultimately confirmed by imaging, spinal cord compression due to epidural bleeding in the context of antiplatelet therapy.
Spontaneous epidural hematoma is rare (0.1 cases per 100 000 inhabitants a year).1 Typical manifestations are shooting cervical, dorsal, or lumbar pain accompanied by motor or sensory deficits due to spinal cord compression showing variable progression over time.2
Spontaneous epidural hematoma in the context of STEMI is very rare. There have been some reports of cases occurring immediately after catheter placement in patients treated with glycoprotein IIb/IIIa inhibitors3 or unfractionated heparin,4 and fundamentally in the context of emergency fibrinolysis.4,5 Few cases associated with long-term aspirin or clopidogrel use have been described,6 and to our knowledge, this is the first report of spontaneous epidural hematoma in a patient being treated with aspirin and ticagrelor. Spontaneous epidural hematoma was not attributable to catheter placement in our case as the events were not linked in time.
MRI is the diagnostic test of choice for spontaneous epidural hematoma1 and the gold-standard treatment is laminectomy and hematoma evacuation. Conservative treatment produces good outcomes in patients with few symptoms.2 Mortality is around 1.3%, but morbidity is high. Thirty percent of patients develop neurological deficits, and those with a more severe presentation or with predisposing factors for bleeding have a worse prognosis.2
The patient in our case recovered mobility in all four extremities following the laminectomy. After 7 days of monitoring and rehabilitation, he was restarted on aspirin monotherapy because of the spontaneous nature of the bleeding. He was discharged 3 days later without motor deficits and with minimal general hyporeflexia. There have been no ischemic or neurological complications in 6 months of follow-up.
Although rare, shooting spinal pain associated with neurological deficits in a patient on antiplatelet therapy should raise suspicion of spontaneous epidural hemorrhage. Prompt diagnosis and treatment is important. Nonetheless, because this condition is so rare, we do not believe it necessary to modify the current antiplatelet strategy for patients with STEACS.
FundingThis study received no funding.
Authors’ contributionsP. Vela Martín and C. Parra Esteban conceived the idea for this manuscript, reviewed the literature, and wrote the first and last draft of the manuscript. M. Carretero Rodrigo and I. Lipperheide Vallhonrat contributed to the discussion of the case and revised the first and final draft of the manuscript. J. Ortega Marcos and L. Silva Melchor contributed to drafting the manuscript and revised both the draft and final version.
Conflicts of InterestThe authors declare that they have no conflicts of interest in relation to this manuscript.