Coronary atherosclerosis is a significant cause of death in the developed world that quite frequently presents as a fatal event, hence the interest in detecting it in its subclinical stages.1 In practice, risk stratification scales are used in population-wide screening to enable us to initiate primary prevention measures. In some parts of Spain, an adapted Framingham scale has been developed,2 which facilitates screening for high- and low-risk patients. However, it has known limitations in screening low to intermediate-risk patients, for whom other approaches to stratification (biomarkers, imaging techniques) are more useful. In particular, detecting and quantifying coronary wall calcium with multidetector computed tomography (MDCT) has been shown to increase the predictive value of risk scores in asymptomatic patients at intermediate risk but fails to identify patients with noncalcified atherosclerosis.3
Our objective was to determine the prevalence of subclinical coronary disease by using noninvasive coronary angiography (NCA) with MDCT in asymptomatic patients and associate this with the adapted Framingham-REGICOR scale of coronary risk levels.
From 2004 thru 2011, we studied 207 consecutive patients (160 men) in the Mediterranean area of Spain who were asymptomatic, aged from 33 to 75 (mean, 54.6 [10]) years, and undergoing a voluntary general check-up including NCA-MDCT (Toshiba Aquilion 64 or 320 detector CT systems). Mean follow-up was 28 (26.4) months.
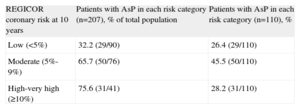
Atherosclerotic plaques (AsP) were identified in 110 patients (53%; 95% confidence interval [95%CI], 49.6%-60.9%), with 1 vessel affected in 33/110 (30%), 2 vessels in 37/110 (33.6%) and 3 vessels in 40/110 (36.3%). The left main coronary artery was involved in 33/110 patients, left anterior descending artery in 101/110, circumflex artery in 48/110, and right coronary artery in 75/110 patients. In 22/110 (20%), AsP were not calcified. We found significant luminal obstruction (≥70%) in 13/110 patients (11.8%), with no calcification in 2 of them. In the group with AsP, 52/110 (47.2%) patients were young (men aged ≤55 or women aged ≤65 years), with noncalcified plaques in 17/52 (32.6%). The patients with AsP presented a mean REGICOR risk score of 7.7% (4.4%) versus 4.5% (3.3%) in the group without evidence of AsP (Table 1). Consequently, the REGICOR risk function significantly associated with presence of AsP (P=.001) with an area under the ROC curve of 0.75. Population-wide analysis by risk category shows 32.2% of patients with low REGICOR risk presented AsP, as did 65.7% of moderate-risk and 75.6% of high-risk patients; differences between the groups were statistically significant (Tables 1 and 2). In 95.5% of patients with noncalcified plaques (21/22), REGICOR risk levels were low or moderate. The REGICOR risk levels in patients with significant lesions varied: in 3/13 (23.1%) risk was low; in 6/13 (46.2%), moderate; and in 4/13 (30.8%), high-very high.
Atherosclerotic Plaques Odds Ratio in Noninvasive Coronary Angiography Using Multidetector Computed Tomography for the Characteristics of Patients Included in the Study
| Total population (n=207) | NCA-MDCT | P | OR (95%CI) | ||
| Without AsP (n=97) | With AsP (n=110) | ||||
| Age, years | 54.6±10 | 50.1±9 | 58.5±84 | <.001 | 1.1 (1.07-1.15) |
| BMI | 27.3±4.4 | 27±4.7 | 27.6±4 | .439 | 1.03 (0.96-1.10) |
| Men | 160 (77.2) | 68 (70.1) | 92 (83.6) | .016 | 2.18 (1.11-4.24) |
| HT | 53 (25.6) | 20 (20.6) | 33 (30) | .151 | 1.6 (0.87-3.12) |
| DLP | 123 (59.4) | 49 (50.5) | 74 (67.2) | .016 | 2.01 (1.14-3.53) |
| Diabetes mellitus | 13 (6.3) | 4 (4.1) | 9 (8.2) | .264 | 2.07 (0.62-6.95) |
| Smokers | 108 (49) | 37 (38.1) | 71 (64.5) | <.001 | 2.95 (1.67-5.20) |
| REGICOR scale, % | 6.2±4.2 | 4.5±3.3 | 7.7±4.4 | <.001 | 1.27 (1.15-1.39) |
| REGICOR <5% | 90 (43.4) | 61 (62.9) | 29 (26.4) | <.001 | 0.21 (0.11-0.38) |
| REGICOR 5%-9% | 76 (36.7) | 26 (26.8) | 50 (45.5) | .006 | 2.27 (1.26-4.08) |
| REGICOR ≥10% | 41 (19.8) | 10 (10.3) | 31 (28.2) | .002 | 3.41 (1.57-7.41) |
95%CI, 95% confidence interval; AsP, atherosclerotic plaque; BMI, body mass index; DLP, dyslipidemia; HT, hypertension; NCA-MDCT, noninvasive coronary angiography using multidetector computed tomography; OR, odds ratio.
Data are expressed as mean±standard deviation or no. (%).
REGICOR Coronary Risk at 10 Years
| REGICOR coronary risk at 10 years | Patients with AsP in each risk category (n=207), % of total population | Patients with AsP in each risk category (n=110), % |
| Low (<5%) | 32.2 (29/90) | 26.4 (29/110) |
| Moderate (5%-9%) | 65.7 (50/76) | 45.5 (50/110) |
| High-very high (≥10%) | 75.6 (31/41) | 28.2 (31/110) |
AsP, atherosclerotic plaque.
In the follow-up, 1.5% of patients had coronary events (1 sudden death due to infarction; 2 unstable angina, 1 of them with percutaneous treatment). All the patients who had events during follow-up, showed nonobstructive AsP in the NCA-MDCT, 1 of them without presence of coronary calcium, with low risk in 1 patient and moderate risk in the other 2.
Prevalence of silent AsP in our series was high (53%). Among the few publications on the topic, the largest study (n=4320) showed 24% prevalence,4 less than in our series, in a population that was younger, of Asiatic origin, with a higher proportion of women and lower prevalence of risk factors.
In our series, risk factors—except hypertension, body mass index and diabetes mellitus—associated significantly with AsP (Table 1). However, in the coronary risk analysis, 26% of patients with AsP had a low REGICOR risk score and just over 45% of affected patients were in the moderate-risk group (Table 2). Although the principal objective of risk functions is to estimate mid-term cardiovascular events, it is recognized that they have limitations when used to improve stratification of intermediate risk patients, who constituted most of those with events in our series.
In conclusion, the results obtained are in accordance with scientific evidence that highlights the important prognostic role of the presence and extent of AsP,5 including nonobstructive and noncalcified plaques (20% in our series), as potential underlying factors in acute coronary events. Although coronary lesions are highly prevalent in the high-risk group in our series, as we would expect, the moderate-risk group includes the higher absolute number of patients with lesions due to the high proportion of the population classified at this level. This supports the earlier observation that the higher number of coronary events also occurred in this group, underscoring the need to improve stratification of intermediate-risk patients. To achieve this, the use of NCA-MDCT may prove important as, in contrast to coronary calcium studies, it identifies ≤11% of patients with noncalcified plaques with potential clinical implications. Notwithstanding, to be able to systematically recommend NCA-MDCT in this risk group we still need to conduct population-wide studies to prove it benefits on prevention.
The authors would like to thank Dr Jaume Marrugat and Dr Roberto Elosua (Institut Municipal d’Investigació Mèdica [IMIM]) for their much appreciated comments that enabled us to improve the present manuscript, and Toshiba Medical Systems for their generous help in financing the principal researcher (M.D.) through a clinical research grant.