Keywords
INTRODUCTION
Coronary heart disease (CHD) is the main cause of death in most industrialized countries,1,2 and myocardial infarction (MI) the most dominant manifestation of the disease. In Spain, 11.2% of deaths in males and 9.6% of deaths in females were related to CHD in 2004.3 Although mortality from CHD has declined steadily both in men and women,4,5 it still remains one of the most important mortality causes and it is considered it will be a major public health problem during the decades ahead.6
CHD is also a very frequent cause of hospitalization in Spain. The number of hospitalized patients discharged with the diagnosis of CHD has tripled in the last 5 years.7 This has made it a priority of health-care policy, not only because of its social repercussions, but also because of its impact on the health-care system.8 Incidence studies conducted in the Spanish adult population indicate that CHD is a frequent disease, with rates of 200 and 50 new MI cases per 100 000 in men and women respectively.9-15 At present, the higher incidence can be observed in the older age group, being the primary cause of death in those older than 65 years-old (15% of total mortality).3 In Spain more than 58% of discharged patients with the diagnosis of cardiovascular disease are over 65 years and 60% of MI patients admitted to hospitals are over this age.7 Although rates are higher after the age of 65,3,7 most epidemiological studies focused on the middle-aged adult population, with scarce representation of the elderly.16 In fact, only few studies include participants older than 65 years old and very few older than 75.17 The impact of the striking demographic changes in the Spanish elderly population, with 10 million of new elderly during the last 10 years, on the incidence of CHD needs to be evaluated.
The aim of this paper is to estimate the age- and sex-specific incidence and mortality rates of MI and CHD in a cohort of Spanish elderly during 10 years of follow-up (1995-2004).
METHODS
Study Population
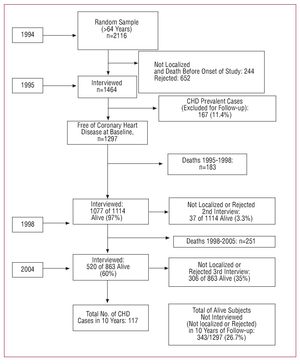
The EPICARDIAN project is a multicentre, population-based, epidemiological, cohort study of cardiovascular diseases in the elderly population of 3 Spanish areas: Lista district (Madrid city); Arévalo county (Avila); and Begonte county (Lugo). Study design and methods in the 3 study areas has been previously published.18,19 In this article we report the results available for the Lista district. According to the official census of Madrid City, on March 31, 1991 Lista district comprised 5540 subjects older than 64 years. An age- and sex-matched random sample of residents older than 64 years was selected in 1994 (n=2116). Subjects with evidence of relevant disabilities and handicaps, life-threatening diseases (ie, end-stage cancer), or institutionalized were excluded. In 244 cases (11.5%) no answer was obtained due to registration errors, changes of residence or death prior to the study's commencement. A total of 652 subjects (30.8%) rejected or could not be found after several attempts. In total, it was possible to perform baseline evaluation (year 1995) on 1464 subjects. Of those, 167 subjects (11.4%) were excluded because they had previous history of clinical cardiovascular disease (prevalent cases). The prevalence of possible MI was 4%, possible stroke 3.5%, and peripheral vascular disease 1.5%. The final sample was composed by 1297 subjects free of clinical cardiovascular diseases. The same clinical examinations were repeated in 1998 and 2004. Follow-up information (medical information and vital status) was updated every year. All participants were followed until the occurrence of the first MI, until death or until December 31, 2004 if alive (Figure 1).
Figure 1. Flow-chart EPICARDIAN study (1994-2004). CHD indicates coronary heart disease (CHD).
Field Study Procedures
The fieldwork was organized into 2 phases. First phase included a home interview. Registered nurses were trained and certified in performing the interview and the examination. Demographic and social data, personal and family history of major cardiovascular diseases, lifestyle information, and regular drug consumption were obtained using questionnaires adapted and validated in Spanish by the MONICA project.20 The interview also included the Rose questionnaire on chest pain and dyspnea.21 Those subjects who rejected the home interview received a self-administered questionnaire by mail, and their relatives were contacted in order to obtain information about their general health, particularly risk factors and cardiovascular diseases. We also periodically requested information from the Madrid office of the National Institute of Statistics for those subjects unreachable or dead at the time of the interview.
The second phase pertained to those individuals who responded positively to the questions about cardiac disease or angina in the first phase. We used the methods previously used and validated in the MONICA Project,20 and modified and adapted in Spain by the REGICOR and the IBERICA projects.22,23 These pursuit and follow-up procedures were adapted to local characteristics of Lista district. Follow-up information was updated every year through emergency services, public and private hospital and primary care centres within the area, in all members of the cohort regardless of they were localized or rejected the follow-up interviews. Phone calls to the subjects and their relatives were held for those not contacted and rejections. Information on vital status of the cohort members was annually updated with the National Institute of Statistics in Madrid. In 1998 and 2004 interviews and clinical examination were repeated using the same contact procedures and interview methods as in 1994.
Definition of Myocardial Infarction (MI)
The criterion was based on symptoms, enzyme changes, electrocardigraphic (ECG) changes (Minnesota code),24,25 and post-mortem findings defined in the WHO coding criteria.26 The validity of the diagnosis was ensured by intra-observer studies.27
We considered definite MI in those subjects who presented a definite ECG or typical/atypical symptoms, together with a probable ECG and abnormal enzymes, or those with typical symptoms, abnormal enzymes, and ischemic ECG.
Possible MI or coronary death was considered in living subjects with typical symptoms where enzymes and ECG did not allow classification into the definite category, with no evidence of other diagnosis; or death patients with no clear evidence of other cause of deceased.
No MI was established in living patients when the symptoms and diagnostic tests combinations did not allow classification into the possible MI or when the event could be explained by means of other causes. In fatal events, MI was rejected when death was related to different clinical diagnosis or autopsy.
Statistical Methods
Basic statistics of centralization (mean, median and its standard deviation, and distribution values) were used to describe continuous variables. For the calculation of rates and proportions, the distribution of relative frequencies with confidence intervals at 95% by the Poisson approximated method was used.28
To compare proportions the Pearson c2 test or the c2 for lineal trend for several categories were used. A P value less than .05 was considered significant. The Kaplan-Meier29 actuarial method was used in order to estimate the cohort survival and crude incidence rates. Crude incidence rates were standardized by the direct method using the standard European population in 2006 as reference.30
Incidence rate is the number of first fatal and/or non-fatal events divided by midyear population at risk. Mortality rate is the number of fatal events divided by midyear population at risk. Case fatality is the proportion of fatal MI in all MI. Incidence and mortality rates are presented per 100 000 person-years, and case-fatality as a percentage by age and sex groups for the 10-year follow-up.
RESULTS
The general characteristics of the initial cohort (n=1297 persons) are described in Table 1. There were 509 men (39.2%) and 788 (60.8%) women free of clinical cardiovascular disease. The majority of participants (87.7%) were aged less than 84 years at baseline. The mean age at baseline was 75 (0.39) years (75 in women and 74.9 in men). Approximately 50% of the sample was married, 30% were widowed, 17% were single, and 3% were divorced. There was 1.6% illiteracy. The 56.8% of subjects meet clinical criteria of hypertension according to the V Joint National Committee (JNC-V) definition; 26.6% had hypercholesterolemia by the National Cholesterol Education Program (NCEP) criteria, 6.7% meet the WHO criteria of diabetes, 59.7% were obese (body mass index ≥30 kg/m2) and 13.9% were smokers by the WHO criteria (Table 1).
The initial cohort of 1297 subjects accounted for a total 9987 persons/year of follow-up. Mean follow-up for the entire cohort was 7.7 years. During the 10-year follow-up period 434 persons (33.4%) died and 343 persons (26.7%) could not be interviewed personally. Nevertheless, we obtained cardiovascular information through secondary sources (primary-care centres, hospital reports, mail, phone calls, etc) for those subjects not contacted or who rejected the scheduled clinical interview. Death certificates were obtained through the Madrid INE office for all those individuals not localized, who rejected the interviews or died before December 31, 2004 (n=777). In total, 117 coronary events occurred in the entire cohort during the 10-year follow-up period. There were 33 cases of non-fatal definite MI; 38 of fatal definite MI; 19 of possible MI; and 27 of sudden death (Table 2). Men showed a higher and significant cumulative risk of ischemic events (P<.001) and sudden death (P<.001) and a higher, but not significant, risk of definite MI (P=.181). Risk of definitive acute myocardial infarction reaches significance when analyzed by age (P<.01). The analysis by age also showed that differences by gender decrease as men and women get older, except for the case of sudden death.
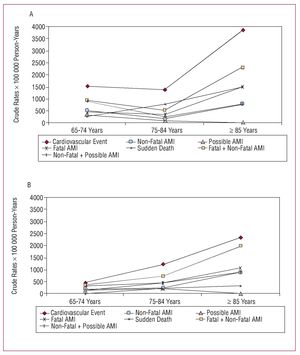
Incidence rates (first event) by sex and age of different acute myocardial infarction diagnostic categories are shown in Figure 2. Males older than 85 years showed the highest incidence rates (P<.001). Incidence of first definite (fatal and non fatal) MI was 710.9 (95% CI, 555.6-895.9) per 100000 person-years, greater in men (889.3; 95% CI, 609.1-1253.2) than in women (610.4; 95% CI, 434.4-833.5) (P<.001). Age-adjusted incidence rate for MI was 883 per 100 000 person-years in men and 696 per 100 000 person-years in women.
Figure 2. Rates by sex and age of different acute myocardial infarction diagnostic categories. A: men. B: women.
Four hundred and thirty four out of 1297 subjects died of any cause during the 10-year follow-up period, which represents a total mortality of 33.5% (95% CI, 30.9-36.1). Mortality was higher in men 42.2% (95% CI, 37.9-46.6) than in women 27.8% (95% CI, 24.7-31.1) (P<.001) and higher in older groups than in younger groups in both sexes (P<.001). The specific mortality for CHD, MI, or sudden death, was 5% (95% CI, 3.8-6.3), higher in men 7.1% (95% CI, 5.0-9.6) than in women 3.7% (95% CI, 2.5-5.2) (P<.01) and increased significantly with age (P<.001). Finally, MI as a definite cause of death was confirmed only in 38 subjects, which resulted in a specific MI mortality of 2.9% (95% CI, 2.1-3.9). MI mortality was higher, but not significantly, in men than in women (P=.482) and among the older groups (P<.01). Case fatality increase with age and was higher in men than in women of all age groups, except in the 75-84 age-group, but it did not reach statistical significance (Table 3).
CHD mortality rate was 650 cases per 100000 person-years with higher figures in men (1000 per 100000 person-years) than in women (453 per 100 000 person-years) (P<.001). MI mortality rate was 380 (95% CI, 269-521) cases per 100 000 person-years, greater in men (472; 95% CI, 248-697) than in women (328; 95% CI, 188-469) (P<.001). Age-adjusted mortality rate for MI was 470 per 100000 person-years in men and 386 per 100000 person-years in women. MI mortality rate in the population aged ≥85 years old reached the highest value with 1241 cases per 100000 person-years, almost 3 times more than in 75-84 age-group (445 per 100 000 person-years), and 6 times higher than in 65-74 years old (232 per 100 000 person-years) (P<.001).
DISCUSSION
In the present study we show that in subjects older than 65 years, the incidence and mortality rates for MI are much higher than in thes middle-age adult population (<65 years old).31,32 The cohort includes a significant proportion of subjects older than 80 years (22.4%), an aspect of interest, given the scarce data on this subgroup of age.
During the last few years, several epidemiological studies have been initiated in Spain to estimate the MI incidence and mortality. However, they9,22,23 were limited to middle-age subjects and included few participants from the older age groups. A recent registry, the REGICOR-65 plus, provides information on MI incidence, mortality rates, and case-fatality in the elderly population of Girona, but only MI cases occurring between 1996 and 1997 were registered, which may not represent exactly the real change in risk over time.33 To our knowledge, this is the first population-based cohort study in the elderly in Spain, with individual follow-up of study participants for a long period of time.
In order to compare our results with other studies we adopted previously used and validated international epidemiological procedures and criteria for the identification and classification of MI.34,35 Nevertheless, almost all epidemiological studies share similar limitations when trying to identify cardiac events. One important limitation is the difficulty to identify silent ischemia. The proportion of silent ischemia reaches 30% in some special populations, being particularly high in the elderly and the postmenopausal women.36-38 We tried to minimize this potential underestimation using multiple specific strategies such as reviewing clinical reports. Such a limitation should especially be taken into account in this study, with an elderly population in which there is a large proportion of women. Other particular limitation is the possible underestimation of ischemic events, especially during the third period of follow-up (1998-2004), due to the elevated proportion of subjects not contacted (n=343; 26%). Nevertheless we used secondary sources of information in order to detect possible cases of MI in all of these subjects. It should be also emphasized that the diagnosis of MI was not only based on the ECG, but also on the clinical symptoms and the results of laboratory testing (CK-MB elevations). One might always speculate that the application of more recent diagnostic tools, such as troponin levels, might have revealed a higher proportion of MI cases, as has been estimated by other studies.39
Once these potential limitations are assumed, the incidence of definite MI seems to be in accordance with other studies carried out in Spain. These studies show that incidence rates amongst the elderly are much higher than rates in middle aged-adults. This may be related to longer exposure to risk factors and to the increased extension of atherosclerosis. This finding is of crucial importance since elderly people are the fastest growing population segment in western countries and, in consequence, demand for health resources of diagnosis and treatment is bound to increase.40 MI incidence rates were significantly higher in men than in women. The incidence increases dramatically from the age group of 65 years to ≥84 years old. This increase was progressive in women but not in men. Other studies in the elderly have observed a similar pattern, with a concentration of MI cases in men in the age group 65-7441 and over this age (after 75 years old) in women.33 The question arises of whether males prematurely develop CHD because of a gender-related genetic predisposition or whether their occurrence is delayed in women because of a shorter exposure to relevant cardiovascular risk factors. In our study, the burden of cardiovascular risk factors is bigger in the elderly women than in the elderly men (Table 1), and this could also affect to the gender differences observed in the CHD incidence and mortality, with a relative higher increase in women.
When comparing our results to those of the REGICOR-65 plus study,33 a registry in a Spanish elderly population, we observed higher absolute values in our study but similar age- and sex- distribution, confirming an exponential increase with age, and higher risk in men than in women. The differences in absolute values could be explained by geographic differences in MI incidence between Mediterranean and Central areas of Spain. These geographic variations have also been demonstrated in the middle-age adult population by the IBERICA study.23 Besides this, both studies have different designs: REGICOR-65 Plus estimations are based on the registry of MI cases in the elderly of an area of Girona during 1 calendar year. In contrast, the EPICARDIAN study accounted for the total number of cases appearing during a period of 10 years. This approach consider the increase in individual risk as the population gets older. Of interest is also that differences between men and women are narrower as they become older. The same pattern has also been observed in other population-based studies.
Incidence rates in our study are also lower than other European36,42 and American43-45 cohort studies, but ageand sex- distributions are quite similar. This finding can be explained by a real higher MI incidence in north-European and American elderly populations, as has been described for a middle-aged adult population in the International MONICA study. In the Rotterdam study for instance, incidence rates were 1200 cases per 100 000 person-years for males and 700 for females.36
In the US Cardiovascular Health study, incidence was 2070 cases per 100 000 person-years in men and 790 per 100 000 person-years in women. The incidence of MI was also strongly associated with age, increasing from 780 in subjects aged 65-69 to 2560 in subjects aged 85 years and older.43 Other international published studies42,44,45 have showed similar rates. Therefore, incidence due to definite coronary events is lower in our study than in other international studies in an elderly population. Since the Spanish elderly, as middle-aged adults, show a high prevalence of cardiovascular risk factors,19 the intriguing paradox of a low MI incidence and mortality in southern Europe despite the high cardiovascular risk factor prevalence46 is likely to hold in older ages.
In Spain, mortality information is usually obtained from official vital statistics published by the National Institute of Statistics. Previous studies47,48 have validated death certificate information showing a detection rate of approximately 90%. In the EPICARDIAN study, as in the IBERICA study, when MI could not be confirmed as the cause of death, the case was referred to as "sudden death." Under this epigraph were included those subjects who died within the first 24 hours from the onset of clinical symptoms, deaths without witness or when the subject was well in the previous 24 hours. In our study the proportion of sudden death was similar to the one found by Bayés de Luna et al,49 which is amongst the lowest described in the international literature. After taking this into account, we found more similar mortality rates in, men and women than those in the REGICOR-65 plus study.33 Increased mortality with age may be related to lower effectiveness of life-saving treatments, lower hospitalization rates, lower use of diagnostic and therapeutics procedures, longer delay between onset of symptoms and admission to the emergency room and more co-morbidity in the elderly.50-53 Men showed a significantly higher CHD mortality compared with that of women, but gender differences are less evident when specific mortality rates (MI rates instead of CHD rates) are considered.
In summary, we conclude that incidence of fatal and non-fatal myocardial infarction is very high in the elderly population of Madrid. Incidence and mortality rates increase dramatically with age after 64 years. Men show higher rates than women at any age but, gender differences diminish with age.
ACKNOWLEDGMENTS
To Ana Isabel Ortega for writing and editing assistance; to Eva Martínez-Renedo for statistical assistance; to Javier Muñiz, and Saturio Vega members of the EPICARDIAN Study Group (Lugo and Arévalo), ERICE and RECAVA networks; to Carlos Brotons (member of ERICE and RECAVA networks), to Francisco Fernández-Avilés (coordinator of RECAVA), and to Pedro Luis Sánchez (secretary of RECAVA) for reviewing and improving this paper with their comments.
ABBREVIATIONS
CHD: coronary heart disease
ECG: echocardiography
MI: myocardial infarction
This Project has been supported by Fondo de Investigaciones Sanitarias (FIS): PI. 93/0012; 96/1993; and 02/0896; Ministry of Science and Education: PB94-1255-C04 and by Instituto de Salud Carlos III: Red ERICE (Reference: G03/065) and Red RECAVA (Reference:RD06/0014/0015).
Correspondence: Dr. R. Gabriel Sánchez.
Unidad de Investigación. Hospital Universitario La Paz.
P.o de la Castellana, 261. 28046. Madrid. España.
E-mail: rgabriel.hulp@salud.madrid.org
Received July 25, 2007.
Accepted for publication June 9, 2008.